Cardio4.14INFEC_INFLAMDIS
advertisement

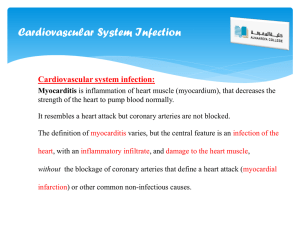
INFECTIVE / INFLAMMATORY CONDITIONS OF THE HEART Infective/inflammatory conditions of the heart may be caused by any of the following: Bacteria Viruses Autoimmune conditions (especially Rheumatic Fever, Rheumatoid Arthritis, SLE) Drug reactions In the immunosuppressed may also be caused by fungus (especially Candida) In all cases RMT should be aware of medication being used by the client because the treatment may have to be adapted if the person is taking anti-inflammatories. ENDOCARDITIS Endocarditis is inflammation and/or infection of the endocardium. The endocardial lining of the heart is a continuation of the intimal layer of the blood vessels and also lines the heart valves. Endocarditis is a relatively uncommon, but not rare condition. Infective endocarditis occurs when microorganisms adhere to the endocardial surface of the heart. It is most commonly bacterial in origin but may also be fungal or viral or secondary to autoimmune disease. Irregular surfaces such as heart valves are most commonly affected. Areas of congenital, septal and mural defects are also susceptible areas. Normally, the smooth inner lining of the heart is inherently resistant to foreign organisms adhering to it. When an infecting agent is able to attach to the endocardium and ‘set up shop’, the person’s blood stream provides an ideal environment for proliferation. Bacterial endocarditis is often caused when bacteria are introduced to the bloodstream during dental surgery or other medical procedures. Anyone with underlying abnormalities of the heart may, therefore, be predisposed. In these instances, prophylactic doses of antibiotics are often given before ‘risky’ procedures. Endocarditis may be classified as ‘acute’ or ‘subacute’ based on how long the infection has been present before it is recognized and treated, or by the nature of the infecting organism (ie. bacterial, fungal, viral). Acute disease is more severe, associated with fever, systemic toxicity, and death from sepsis in several days to weeks. Subacute disease usually occurs in patients with prior valve disease. It is less severe, associated with low grade fever, vague systemic complaints and various embolic phenomena. The endocardium usually repairs well, but there is a risk of valvular damage since the fine tissues of the valve cusps are extensions of the endocardium. Other complications of endocarditis include: Vegetations o Lesions; clusters of the infecting organism or localizations of autoimmune activity o often develop on/inside the cusp (i.e. pockets) of the valves o they can be either stable or unstable vegetations of autoimmune disease are more like erosions of tissue and tend to be quite stable vegetations of bacterial or fungal origin are susceptible to breaking away from the wall/valve under the hemodynamic pressure of the heart. They can create dangerous emboli. This type of unstable vegetation is referred to as friable. Signs and Symptoms of Endocarditis: May have general symptoms of fever, chills, fatigue, weight loss, muscle ache, and sweating Acute valve damage may lead to acute s/s of CHF (pulmonary edema and SOB) The infection may spread, especially to the kidneys, leading to hematuria Constant deep achy chest pain that doesn’t change with rest or activity Treatment: Medical treatment is to treat the cause (infection or autoimmune disease). Infections are usually treated with long-term antibiotics (often four-six weeks, or more). If valve damage has occurred, surgical repair or valve replacement may be required. Complications: 1. Thrombosis, Embolism (thrombus, vegetations, or septic material [may also spread the infection]) 2. Permanent valve damage (heart murmur, and possibly a need for repair or replacement surgery in extreme cases) 3. CCHF secondary to the valve problems RMT Concerns: 1. avoid treatment while the condition is active and the risk of embolism is high (consultation with M.D will be necessary) 2. with a previous history of endocarditis, the RMT should establish whether there is a present risk of embolism 3. client may be taking anticoagulants i.e. increase bleeding/bruising 4. assess for CCHF status and adapt treatment accordingly MYOCARDITIS Myocarditis is an inflammatory condition of heart muscle that can result from a variety of causes. Most cases are viral in nature, but toxins, drug reactions, and autoimmune reactions are also common causes. Myocarditis also commonly occurs post myocardial infarction. It is a rare but serious condition that affects men and women at any age. The most common causes are: viral infection, post myocardial infarction, autoimmune disease and drug reactions Acute myocarditis is a rare inflammatory disease, which may lead to the sudden onset of cardiac failure and death. Myocarditis can cause considerable morbidity and mortality and may lead to dilated congestive cardiomyopathy. The clinical diagnosis of myocarditis is difficult and many times is arrived at only after more common problems including asthma, recurrent vomiting, and chronic viral illness such as mononucleosis are excluded. Viral myocarditis is preceded many times by a flu-like illness or gastroenteritis. When patients present with the classical findings of congestive heart failure (i.e. tachypnea abnormal rapid respiration or tachycardia - abnormal rapid heartbeat), the diagnosis is more apparent. Signs and Symptoms: Viral infections are often asymptomatic (and may remain undiagnosed) May present as a constant deep pain similar to endocarditis, or with fatigue, SOB, fever, and arthralgia. If the condition persists, CHF may develop Sudden, acute myocarditis may also appear in the form of heart failure or sudden cardiac death May disguise itself as ischemic, valvular, or hypertensive heart disease. Medical Treatment: No medical treatment is necessary with viral infection. Viral causes are generally self limiting. Management is through rest and avoidance of physical exertion (to avoid additional stress to the heart) Fever, chest pain, CHF, arrhythmias, or syncope may develop, requiring medical management If bacterial infection is the cause (rare), antibiotics are introduced Autoimmune causes are usually the most difficult to treat RMT Concerns: o Not considered dangerous for massage in the ‘active’ phases o Awareness of CHF concerns if cardiomyopathy/CHF develop PERICARDITIS Pericarditis is inflammation or irritation or the pericardium; the outer, protective covering of the heart. The pericardium helps anchor the heart in place, preventing excessive movement of the heart in the chest cavity with changes in body position, helps to protect the heart from infections and invading tumors, and may help keep the heart from enlarging. There are many possible causes of pericarditis: trauma or infection from heart surgery, post MI pericardial irritation (esp. if there is a slow bleed through a mural defect [blood is corrosive]), autoimmune disease (rheumatoid arthritis or lupus), cancer (an adjacent lung cancer may irritate or metastatic disease can directly invade the pericardium), kidney failure (irritation due to toxicity of the blood), drug reactions, radiation therapy (due to burn injury). The pericardial space is lubricated by lymph and usually contains 10 to 30 cc of fluid. This fluid provides protection to the heart, and decreases friction with movement/beating of the heart. An increase in pericardial fluid is called an effusion. In patients with a small effusion, a pericardial ‘rub’ may be heard. It is a scratching, grating sound best heard along the left sternal border, with the patient in the sitting position. In the presence of a large pericardial effusion, the heart sounds may be diminished or absent. The reduction of cardiac filling from a large effusion may lead to cardiac tamponade (increased fluid and resultant pressure fully restrict heart filling and pumping, leading to cardiac arrest and death). Certain infections may lead to bacteremia which can spread to the pericardium. Patients then usually present with fever and irritability. Tachycardia, tachypnea, and chest pain with respiration or cough are common. Signs and Symptoms: Systemic symptoms or the original cause may be present (fever etc with infective causes) Constant, extreme chest pain - considered to be the most painful heart condition Pain is generally felt below the sternum and/or below the ribs in the left side of the chest and occasionally into the upper back or neck. Pain is exacerbated by deep breathing and excessive movements Lying may exacerbate, sitting up and forward may relieve symptoms tachycardia and tachypnea are also common Medical Treatment: Is related to the cause Complications o Risk of pericardial effusion leading to cardiac tamponade o Exudate developed in the pericardium can result in adhering between the visceral and parietal layers. Friction during heart beating can cause pain and usually results in reinforcement of the continuously micro damaged adhesion. o Fibrosis in the walls of the pericardial sac can result in thickened nonelastic regions which can cause friction and affect the beat. Concerns for RMT: The condition is not worsened by massage. RMT needs to be aware of overall health concerns in the person whose pericarditis is secondary to another condition. Hx of pericarditis should be followed up for CHF status and intrapericardial; friction problems especially if the heart rate is increased. Valvular Heart Disease Definitions: Valvular regurgitation is the inability of the valve to close properly, resulting in backflow called a heart murmur. Valvular stenosis is the inability of the valve to open properly, resulting in a reduced volume of blood exiting the chamber and considerable pressure in the exit chamber. Valvular incompetence is a non-specific term which just means that the valve is not functioning properly. Most Common Causes: 1. Hypertension/CCHF 2. Complication of MI 3. Rheumatic Fever An autoimmune reaction secondary to infection by streptococcus bacteria. After a period of some weeks, antibodies which have developed to fight the infection appear to sense a chemical similarity between the bacteria and heart tissue. The valves are often particularly aggressively attacked. 4. Endocarditis 5. Congenital Abnormality Concerns for the RMT Mention of heart murmur or any of the causes of valvular disorder on the case hx should lead to the RMT establishing CCHF status. Some heart murmurs are not clinically significant. Adult onset heart murmurs typically indicate some degree of heart failure. Hearts with clinically significant valve problems typically do not adapt easily to increased CO. Watch for signs of dyspnea (i.e. difficult or painful breathing) and increased SNS activity. Watch for increases in BP post treatment.