When is Dead Really Dead?
Mike McEvoy, PhD, REMT-P, RN, CCRN
EMS Coordinator, Saratoga County, NY
EMS Director - NYS Association of Fire Chiefs
Professor Emeritus - Cardiothoracic Surgery, Albany Medical College
EMS Editor – Fire Engineering magazine
Disclosures
• I have no financial relationships to
disclose.
• I am the EMS technical editor for Fire
Engineering magazine.
• I do not intend to discuss any unlabeled
or unapproved uses of drugs or
products.
Not Suitable for Small Children
www.mikemcevoy.com
Outline
• EMS: Bringing out the dead
– Involvement in field pronouncements
– Problems
• Criteria for death
• Why we screw it up
• How to stay out of hot water
– Standard practice for field pronouncement
– Dealing with difficult cases
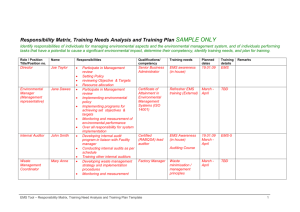
How many?
•
•
•
•
•
Pronounce death?
Declare death?
Honor DNR?
Decide not to initiate resuscitation?
Stop resuscitation someone else
started?
• Terminate field resuscitation?
Case # 1
• R-10, A-15 sent to MVC w/ entrapment
• PD @ scene report single vehicle into
concrete bridge abutment, lone
occupant appears deceased
• R-10 EMT-FF’s find approx 16 yo ♂
lying across front floor of compact car
–
–
–
–
Obvious bilat open femur fx
Rigid, distended belly
Blood with apparent CSF from both ears
No observable resps, no palpable pulses
Case # 1 (continued…)
• R-10 officer cancels ambulance
– Advises police that driver is dead
– Requests Medical Examiner to scene
• ME arrives one hour later
– Finds patient breathing, barely palpable pulse
• EMS recalled
– Patient resuscitated, xpt to trauma center
• Dies 2 days later from massive head inj
• Family calls news media, files complaint
with State EMS office
Case #2
• EMS dispatched to reported obvious
death in low income housing project
• Arriving medics find elderly ♀ supine
on kitchen floor
– Apparent advanced stage of decomposition
– Large areas of skin grotesquely peeled from arms
and torso
– Overwhelming foul odor throughout apartment
• Coroner contacted to remove body
Case #2 (continued…)
• Later that evening, hospital morgue
attendant summon resuscitation team
– Supposedly deceased patient moaning for help
• Patient admitted to ICU
– Massive Streptococcus pyrogenes (“flesh
eating”) bacterial skin infection
• Dies 3 days later
• CNN, national news media prominently
carry the story
Isolated Events?
Death
• 2.4 million Americans die annually
– Most deaths are in hospitals (61%)
– Or nursing homes (17%)
• Smallest # die in community (22%)
• Why does EMS lead news stories
on mistaken pronouncements?
Formal Training
• Physicians are taught & practice
death pronouncement
• EMS is not
What Do People Fear?
1. Public speaking
2. Live burial
Fear of live burial
• 1800’s – coffins equipped with
rescue devices
• 1899 – NY State enacted legislation
requiring a physician pronounce
death
• 1968 – Uniform Anatomic Gift Act
authorized organ donation: worries
about premature pronouncements
Premature Pronouncement
• 1968 – Harvard Ad Hoc Committee
on Brain Death published
definition of “irreversible coma”:
1. Unresponsive – no awareness/response
to external or painful stimuli
2. No movement or breathing
3. No reflexes – fixed & dilated pupils, no
eye movement when turned or cold water
injected into ear, no DTRs
• Currently called “brain death”
1981:
• 170+ pages
• Became death
criteria for all 50
states
• Basis for UDDA
(Uniform Determination
of Death Act)
Why?
• Technology
• Pulselessness and apnea
no longer identified death:
– Mechanical ventilation
– Artificial circulatory support
– ICU patients who would never recover could
be kept “alive” indefinitely
• Main goal = standardize criteria for
irreversible loss of all brain function
Brain Death
• EMS doesn’t pronounce brain
death
• Neither does a lone doc, NP, or PA
• Such decisions require:
– Time
– Specialized testing
– Brain specialists such as neurologists
Who does EMS pronounce?
1. People we find dead
2. People we cease resuscitating
So, what’s the book say?
Dead=irreversible cessation
“An individual with irreversible cessation
of circulatory and respiratory function
is dead. Cessation is recognized by an
appropriate clinical exam,” whereas,
“Irreversibility is recognized by
persistent cessation of functions for an
appropriate period of observation
and/or trial of therapy.” (p. 133)
Appropriate Clinical Exam
“Appropriate Clinical Exam”
ABSOLUTE MINIMUM REQUIREMENTS:
1. General appearance of body
2. No response to verbal/tactile
stimulation
3. No pupillary light reflex (pupils
fixed and dilated)
4. Absence of breath sounds
5. Absence of heart sounds
“Appropriate Clinical Exam”
• Deep, painful stimuli inappropriate
– Nipple twisting, sternal rubs…
• Some suggest testing corneal
reflexes
– Duplicates pupillary reaction to light; both
require some intact brainstem function
• When more sophisticated monitors
are available, they should be used!
Death Traps: Red Flags
• Patients found
dead
• Death not observed
or expected
• Death was sudden
• Resuscitation not
provided
Death Traps
• Massive internal injuries
– Lack invasive testing to confirm
• Massive head trauma or GSW
– Often lack experience with these injuries
• Isolated fatal injuries
– Organ donor potential – attempt resus?
• Drug overdose, hypothermia,
massive infections, total paralysis,
hepatic coma, drowning…
Death Traps
• Pediatric patients
• Drowning
– Less than 2 hours may be survivable
• Hypothermia
– Cannot pronounce until > 90°F
• LVAS (artificial heart) patients
Left Ventricular Assist Systems
• LVAS, or “artificial heart”
• Earlier devices were air driven,
pulsatile pumps
• Next gen devices are centrifugal
– Magnetically levitated impeller propels
blood
– Non-pulsatile flow
Centrifugal LVAS
• The patient has no pulse!
Irreversibility….
the Lazarus Phenomonem
• Autoresuscitation (AR)
• Spontaneous ROSC after failed
resuscitation attempt
• Uncommon, theorized due to:
– Delayed effects of resuscitation meds
– Intrathoracic pressure change once PPV
discontinued
• Warrants prolonged observation
AR: Is He Dead Jim?
• Never reported without CPR
– Unless patient not properly pronounced
• No reported cases in children
• No single AR >7 minutes following
termination of CPR
– When proper times were recorded
• Current best practice is 10 minute
observation following termination
Hornby K, Crit Care Med, 2010, 38: 1246-1253
Death Documentation
1. Describe your exam
–
Include time of exam (this is time of death)
Clinical Exam for Death
1. No response to verbal or tactile
stimulation
2. No pupillary light reflex (pupils
fixed and dilated)
3. Absence of breath sounds
4. Absence of heart sounds
Death Documentation
1. Describe your exam
–
2.
3.
4.
5.
6.
7.
Include time of exam (this is time of death)
Location/position where found
Physical condition of body
Significant medical hx or trauma
Conditions precluding resus
Any medical control contact
Person body left in custody of
Employ every available tool
• ALS if available
– Record 15 second EKG in 2 leads
– Attach AED if no ALS available
– Leave electrodes/pads on the body
• Use ultrasound, stethoscope, etc.
• Make certain that the most senior
EMS provider available confirms
the death
Death Traps
• You will never find something that
you don’t look for!
• Every mistaken pronouncement:
– Jumping to conclusions
– Lack of detailed search for any sign of life
• Don’t be dead wrong; be
DEAD RIGHT