Subcutaneous Cladribine for HCL in
the BRAF era
Francesco Forconi (MD, DM, PhD, FRCPath)
Cancer Research UK Centre and Haematology Department
Southampton University Hospital Trust
email: F.Forconi@soton.ac.uk
CLADRIBINE I.V. AND S.C. IN HCL
• Intravenous Cladribine-iv2CdA
– 0.7 mg/kg single cycle
• Continuous 0.1 mg/kg daily over 7
days
• 2-hour 0.1 mg/kg daily over 7 days
• Subcutaneous Cladribine -sc2CdA
– 0.7 mg/kg single cycle
– 100% bioavailability
Juliusson et al, Lancet 1993, J Clin Oncol 1996
Juliusson , NIH, Bethesda, 2010
INFECTIONS WITH CLADRIBINE
Intravenous Cladribine (iv2CdA)
sc2CdA reduction in NHL
– 0.7 mg/kg single cycle
– 42% febrile episodes
0.5 mg/kg/cycle
0.7 mg/kg/cycle
55%
– 13% documented infections
Saven (Scripps), Blood , 1998
Infections (%)
Neutropenia (%)
7
30
8
33
Subcutaneous Cladribine (sc2CdA)
In indolent non-Hodgkin lymphomas other
than HCL:
– at the dose of 0.7 mg/kg/cycle, efficacy of
sc2CdA is similar to iv2CdA
– reduction to 0.5 mg/kg/cycle determines
equivalent efficacy and lower toxicity
p=.003
53
Response (%)
Duration (months)
p=.0001
57
12
7
p=.72
p=.21
Betticher (SAKK), J Clin Oncol 1998
ICGHCL2004 protocol
EudraCT code: ICGHCL2004
2CdA s.c.
0.1 mg/kg/day
Arm A
Arm B
5 days
7 days
PATIENTS
EudraCT code: ICGHCL2004
ARM A
156 patients
(randomised)
24 centers
Central revision
WHO 2001 criteria
• morphology
• HCL phenotype
• CD11c +
• CD19 +
• CD20 +
• CD25 +
• CD27 –
• CD38 –
• CD103 +
• FMC7 +
WHO 2008 criteria
• ANXA1 + (IHC)
- HC>1010/L
- Spleen > 10 cm
- Refractory
Classic HCL
Median follow-up
62 months
ARM B
NON HEMATOLOGICAL GRADE 3-4 TOXICITY
NO
YES
P=,017
Infections or FUO
NO
YES
P=,012
Hospitalization days 7-30
Higher infection rate and hospitalization in standard dose (Arm B) than in reduce dose (Arm A)
RESPONSES TO SUBCUTANEOUS 2CDA
■ CR/PR
■ mR/NR
p=0.7
100
80
60
40
20
0
Arm A
Arm B
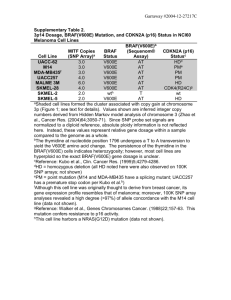
~50% patients investigated for BRAF V600E mutation: no differences in response rates
ENDPOINTS OF SURVIVAL AFTER TREATMENT
TFI: Treatment free interval (2° treatment)
OS: Overall survival
TFI and OS
Arm A
Arm A
Arm B
% surviving
% Treatment free
Arm B
p=0.9
p=0.58
Time to 2° tratment (months)
Overall survival (months)
~50% patients investigated for BRAF V600E mutation: no differences in survivals
MOLECULAR PROGNOSTIC MARKERS OF TFI IN BRAF+ HCL
Multiple Ig isotype
M-IG
IgM
IgD
IgG
UM-IG
IgA
P<.001
AID +
Ongoing SHM
•HCL has a very stabe genomic profile
10
RAF-MEK Pathway
BCR Signaling Pathway
V600E
LYN
RAF
Vemurafenib
PI3K
P
PIP3
P
PDK
AKT
P
Dasatinib
MEK
GS-1101
Ibrutinib
RAS
ERK
PLC
2
BLNK
P
BTK
P
SYK
RAS
CD79B
P
P
CD79A
RTK
IP3
DAG
Ca2+
PKC
Fostamatinib
RAF1
survival
proliferation
transformation
NFAT
survival
ERK
JNK
p38
MYC
JUN
ATF2
apoptosis
proliferation
IKK
NFκB
migration
Conclusions
• Cladribine at reduced doses has lower toxicity and
similar efficacy
• BRAF mutational status: critical to identify patients non
benefiting from Cladribine?
• New effective treatments (if/when required):
• HCL express high levels of multiple Ig isotypes that are functional
• Surface Ig and signaling is irrespective of BRAF V600E
• BCR-inhibitors act on the tumor component that signals through BCR
• BCR-inhibitors as an alternative strategy?
• Markers to identify poor outcome in BRAF+ HCL
Slide 12