Internal Medicine Board Review: Nephrology
advertisement

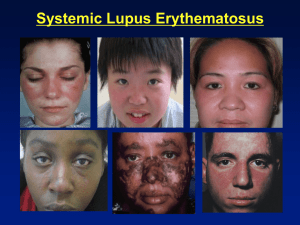
Internal Medicine Board Review: Nephrology Steven Wagner M.D. July 16, 2014 Purpose of board review • • • • Pass the boards Not intended as a complete review “Boards correct” ≠ “real life correct” Pick the right answer and move on And the point is…… • Most questions have a specific teaching point • If you miss the point, you will probably miss the question • Getting the point will not guarantee that you get the correct answer – Still have to understand the rest of the question Inter-nephrologist agreement • Put 10 nephrologists in a room with a patient, and you will receive at least 11 diagnoses • Some might disagree with question format and/or the answers With that in mind, Question 1 A 41-year-old female is seen for follow-up of high blood pressure. She follows a healthy, active lifestyle and does not smoke. She is on no medications or birth control. BP 173/112, BMI 23, other vitals WNL Labs are normal, including renal panel, UA, glucose, and lipids What is the most appropriate NEXT STEP in management of her hypertension? a) Lisinopril / Hydrochlorothiazide b) Diet and exercise c) Norvasc d) See her back in 2 weeks for a blood pressure recheck Key point: manage hypertension • Hypertension is divided into stages • Our patient has stage II hypertension • Will need drug therapy Why the other choices are wrong a) b) c) d) Lisinopril / Hydrochlorothiazide Diet and exercise Norvasc See her back in 2 weeks for a blood pressure recheck • Had a BMI of 23 and a healthy diet • Norvasc is unlikely to be effective alone • She is already “following up” at the current visit. Time to do something. Question 2 A 23-year-old white female is evaluated for 2 months of fatigue, polyarthritis, oral ulcers, and edema. She has no significant medical history and takes no medications. Blood pressure 165/100, other vitals WNL. Ulcers on hard palate and buccal mucose. Erythema and tenderness of the MCP and PIP joints. 2+ LE edema bilaterally. Hb 11, WBC 2.1, PLT 110K, Albumin 3.4, Creat 1.4 UA shows 25-50 RBC, 25 WBC, and erythrocyte casts 24-hour urine protein is 2.5 grams Which of the following is the most likely diagnosis? a) Focal segmental glomerulosclerosis b) IgA nephropathy c) Post-infectious glomeulonephritis d) Proliferative lupus nephritis Key point: diagnose lupus nephritis • Lupus nephritis is characterized by hematuria and proteinuria in the setting of clinical findings of lupus • Diagnosed with: – – – – >500 mg protein in 24 hour sample >10 RBC per HPF RBC or WBC casts in sterile urine (active sediment) OR by kidney biopsy • Remember that lupus is a syndrome • RBC casts indicate GLOMERULAR hematuria Why the other choices are wrong a) b) c) d) Focal segmental glomerulosclerosis IgA nephropathy Post-infectious glomeulonephritis Proliferative lupus nephritis • FSGS generally presents with more proteinuria (nephrotic syndrome) • IgA nephropathy is unlikely in the setting of clinical findings of lupus • The answer can’t be post-infectious without evidence of recent infection (at least on the boards) • NONE of the incorrect answers explain her cytopenias etc Question 3 A 75-year-old man with known alcoholic cirrhosis has 3 weeks of worsening ascites. He still drinks and is not a transplant candidate. Don’t even ask. His only medication is propranolol. He is alert and oriented. BP 109/68, pulse 58, other vitals WNL No neurologic findings, no asterixes Abdominal exam nontender with significant ascites. 1+ LE edema Labs: Albumin 2, BUN 8, Creat 1.6, Na 119, K 3.6, OSM 250 Urine: OSM 156, Na <5 Paracentesis: transudative ascites with WBC 50/uL What is the appropriate management of this patients hyponatremia? a) 3% saline with a goal of correcting Na by 10 in the next 24 hrs b) Conivaptan c) Demeclocycline d) Fluid and sodium restriction Key point: Manage asymptomatic hyponatremia • Management of hyponatremia depends on the symptoms – Increased urgency in the setting of seizures, unresponsiveness, etc • Remember to correct slowly Why the other choices are wrong a) b) c) d) 3% saline with a goal of correcting Na by 10 in the next 24 hrs Conivaptan Demeclocycline Fluid and sodium restriction • 3% saline is too aggressive in this setting • Conivaptan decreases BP and is contraindicated – Tolvaptan also relatively contraindicated now • Demeclocycline is effective in SIADH – This patient has appropriately high levels of ADH Question 4 A 71-year-old female has a 3-year history of hypertension. She feels well. She is compliant with a low-sodium diet and does not smoke. She takes maximal doses of Chlorthalidone, enalapril, amlodipine, and carvedilol. BP 168/112, pulse 68, BMI 26, other vitals WNL Systolic crescendo-decrescendo murmur at the RUSB Normal carotid upstroke, normal JVP Renal panel, UA, CBC, glucose, and lipids are normal. What is the most appropriate next step? a) Ambulatory blood pressure monitoring b) Echocardiogram c) Addition of a vasodilator such as hydralazine d) Urine metanephrine measurement Key point: Diagnose resistant hypertension • You have to diagnose something before you can treat it • She has hypertension in clinic but will need documentation of hypertension outside the office before proceeding Why the other choices are wrong a) b) c) d) Ambulatory blood pressure monitoring Echocardiogram Addition of a vasodilator such as hydralazine Urine metanephrine measurement • Echo would be appropriate to evaluate her murmur, but is not needed for the workup of her hypertension • Hydralazine might be helpful, but first we need a diagnosis • Metanephrines might be helpful once a diagnosis of resistant hypertension is made Question 5 A 38-year-old black female has 6 months of LE edema and weight gain of 10 kg. Her urine is frothy but no hematuria. She takes no medications and has no significant history. BP 155/105, other vitals WNL. BMI is 30 3+ LE edema, otherwise has a normal exam Labs: Albumin 2.4, creat 1.6, LDL 170, SPEP WNL, RF negative, ANA negative, Hepatitis panel negative 24-Urine protein = 7.8 grams Which of the following is the most likely diagnosis? a) IgA nephropathy b) Focal segmental glomerulosclerosis c) Lupus nephritis d) Post-infectious glomerulonephritis Key point: FSGS is pure nephrotic syndrome • FSGS is a common adult diagnosis • Usually not subtle, with heavy proteinuria and nephrotic syndrome – Low albumin – Hyperlipidemia – Edema Why the other choices are wrong a) b) c) d) IgA nephropathy Focal segmental glomerulosclerosis Lupus nephritis Post-infectious glomerulonephritis • IgA nephropathy is generally less proteinuria and also usually has glomerular hematuria • Lupus nephritis usually has glomerular hematuria. Could be class V lupus, but ANA was negative • Post-infectious glomerulonephritis is wrong because there is no mention of an infection Question 6 A 23-year-old female is seen in the ER with 2 months of progressive weakness. She is no longer ambulatory. No diarrhea or weight loss. She has a history of Sjogren syndrome and takes no medications. Vital sign WNL. BMI 22. Diffuse weakness on exam , no atrophy or tenderness Labs: Albumin 4.5, BUN 13, creat 1.1, Na 141, K 1.9, Cl 117, HCO3 14, Phos 3.5. UA benign, no glucose, no WBC, Anion gap = positive Renal ultrasound: nephrocalcinosis bilaterally Which of the following is the most likely diagnosis? a) Gitelman syndrome b) Distal (type I) renal tubular acidosis c) Laxative abuse d) Proximal (type II) renal tubular acidosis Key point: Diagnose distal RTA • Associated with rheumoatologic diagnoses – Sjogrens, lupus, RA • Ability to excrete H+ ions is impaired – Inappropriately alkaline urine pH • Increased pH leads to kidney stones • pH >6 in the setting of hypokalemic acidosis, Sjogrens, and nephrocalcinosis is HIGHLY SUGGESTIVE of distal RTA – This one is not subtle Why the other choices are wrong a) b) c) d) Gitelman syndrome Distal (type I) renal tubular acidosis Laxative abuse Proximal (type II) renal tubular acidosis • Gitelman syndrome would be hypotensive and lytes would look like HCTZ use • Laxative abuse would have a negative urine anion gap – Compensatory increase in ammonium excretion • Proximal RTA would be expected to have a normal urine pH – Distal acidification still intact • Proximal also often associated with glucosuria, Fanconi syndrome Question 7 A 45-year-old female with a history of frequent UTI’s presents with foul smelling urine, dysuria, and urgency. Her last UTI was Morganella morganii. She has a known history of kidney stones. Vitals are WNL Exam is benign Labs: Creat 1.2, Albumin 4.2, Calcium 9.3, PTH 12 UA: pH 7.2, WBC 2+, leukocyte esterase, no hematuria, no protein Due to frequent infections in the setting of kidney stones, a CT scan is performed, which confirms the presence of bilateral staghorn calculi. She proceeds to Urology. What is the most likely composition of her kidney stones? a) Calcium oxalate b) Uric acid c) Ammonium magnesium phosphate d) Cystine Key point: Diagnose struvite stones in the setting of Urease-splitting bacteria • Common urease splitting bacteria are Proteus and Morganella • The boards will not always give you Proteus in these questions • Urine pH is key: – High pH with mention of infection is almost always struvite stones Why the other choices are wrong a) b) c) d) Calcium oxalate Uric acid Ammonium magnesium phosphate Cystine • Calcium oxalate stones are the most common stone (90%) but not with a high pH • Uric acid stones are almost never seen with alkaline urine. Alkalinization is a TREATMENT for uric acid stones • Cystine stones are seen in Cystinuria, a genetic disorder. Think 6-sided crystals Question 8 A 47-year-old female is seen for diabetes followup. She has CKD, HTN, retinopathy, and neuropathy. She is active and follows a diabetic diet. She is on glyburide, amlodipine, and gabapentin. Vitals: BP 124/80, otherwise WNL Exam: Trace edema, otherwise WNL Labs: Creat 3.1, HCO3 17, BUN 88, K 4.8 Which of the following is the most appropriate addition to her current medical regimen? a) Allopurinol b) Phosphate binder c) Sodium bicarbonate d) Sodium polystyrene Key point: Treat metabolic acidosis in CKD with bicarbonate • Non-gap acidosis with chronic kidney disease • Can have a gap with severe renal failure • Treatment with bicarbonate may reduce bone loss and possibly CV morbidity, and seems to slow CKD progression Why the other choices are wrong a) b) c) d) Allopurinol Phosphate binder Sodium bicarbonate Sodium polystyrene • High uric acid is associated with renal disease progression, but multiple studies have failed to show benefit from allopurinol • Phosphate binder is not needed in the setting of normal phosphorus • Sodium polystyrene is not needed in this patient with a normal serum phosphorus, and has a role ONLY in acute hyperkalemia (if even then) Question 9 A 54-year-old female is seen for followup of diabetes and hypertension. She is overweight and noncompliant with all lifestyle interventions. She is on metformin, glipizide, irbesartan, HCTA, and simvastatin. BP 154/82, BMI 38, other vitals WNL Exam: No LE edema Labs: creat 1.2, K 5.1, Phos 3.8, 24-hour urine protein 200 mg In addition to lifestyle modification, which of the following is the most appropriate next step in management? a) Diltiazem b) Furosemide c) Lisinopril d) Spironolactone Key point: Manage hypertension in a diabetic patient • Diltiazem is the best choice in this patient • She is well above the guideline of 130 systolic in a diabetic patient Why the other choices are wrong a) b) c) d) Diltiazem Furosemide Lisinopril Spironolactone • Furosemide is not needed as she has no evidence of volume overload • Lisinopril is not indicated. Studies show no benefit with dual RAS blockade, and there is an increased risk of hyperkalemia • Spironolactone might be effective, but is relatively contraindicated in the setting of borderline hyperkalemia Question 10 A 54-year-old male is seen for a history of frequent nephrolithiasis. At least 2 of his stones were analyzed and found to be uric acid. After his third stone, potassium citrate was initiated. He also has diabetes, HTN, and hyperlipidemia. No known history of gout. His diet consists of red meat with most meals, and he has inconsistent fluid intake. He is on metformin, metoprolol, atorvastatin, and aspirin. Vitals and exam WNL. BMI 32. Labs: BUN 15, creat 1.1, Uric acid 7.8 24-hour urine (mg): Ca 220, Citrate 400, Oxalate 26, uric acid 710 Urine volume: 1600 mg in 24 hours. Urine pH 6.2 Which of the following is the most appropriate treatment? a) Acetazolamide b) Allopurinol c) Calcium carbonate d) Chlorthalidone Key point: Manage uric acid stones with Allopurinol • Patient has uric acid stones in spite of urinary alkalinization • Serum uric acid is elevated • Other risk factors: – High meat intake – Low urine volume • Dietary modification and increased fluid intake would be helpful as well Why the other choices are wrong a) b) c) d) Acetazolamide Allopurinol Calcium carbonate Chlorthalidone • Acetazolamide would alkalinize the urine but would cause metabolic acidosis • Calcium carbonate is used for oxalate stones • Chlorthalidone is a thiazide diuretic, which will increase serum uric acid levels and might lead to the development of gout Question 11 A 75-year-old female is seen for escalating hypertension. She quit smoking 5 years ago after a TIA. She takes metoprolol, amlodipine, and HCTZ. Six months ago her BP was 148/82, three months ago it was 158/90. Today it is 174/96. Vitals: BP 174/96, pulse 61, otherwise WNL Exam: Carotid bruits, epigastric bruits, s4 gallop, 1+ LE edema Lab: Creat 1.7, Na 14, UA normal Which of the following is the most appropriate next step in management? a) Add an ACE inhibitor b) Increase the metoprolol dose c) Obtain doppler ultrasound of the renal arteries d) Obtain renal angiography Key point: Manage revovascular hypertension • This patient has accelerating hypertension • Severe PVD on exam, including epigastric bruits • Treat renal artery stenosis medically unless there is a hemodynamically significant lesion on imaging • Currently much debate on stent vs medical management Why the other choices are wrong a) b) c) d) Add an ACE inhibitor Increase the metoprolol dose Obtain doppler ultrasound of the renal arteries Obtain renal angiography • An ACE inhibitor might cause significant acute renal failure, especially if she has bilateral disease • Metoprolol would slow her pulse further • Renal angiogram is relatively contraindicated with her GFR of about 30 Question 12 A 25-year-old male has dark urine and oliguria. He has 5 days of a URI with rhinitis, sore throat, and fever. Has mild myalgia and bilateral flank pain but no dysuria. He is taking ibuprofen for pain Vitals: BP 135/88, remainder WNL Exam: Erythematous pharynx without exudate, neck lymphadenopathy, 1+ LE edema Labs: Hb 9.8, WBC 9.9, PLT 258K, C3+C4 WNL, CK 95, Creat 2.3, ASO negative UA: >100 RBC, 2-5 WBC, no bacteria Renal US: Essentially normal Which of the following is the most likely cause of acute renal failure? a) Analgesic nephropathy b) IgA nephropathy c) Post-infectious glomerulonephritis d) Rhabdomyolysis Key point: IgA nephropathy causes renal failure concurrent with URI • Gross hematuria with URI can be the first presentation of IgA nephropathy • Mucosal infection causes production of IgA, with abnormally formed IgA antibodies causing nephropathy • Macroscopic hematuria is a favorable prognostic finding • Worrisome findings include severe AKI, age > 50, crescents or fibrosis on renal biopsy Why the other choices are wrong a) b) c) d) Analgesic nephropathy IgA nephropathy Post-infectious glomerulonephritis Rhabdomyolysis • Hematuria is not a feature of analgesic nephropathy • Post-infectious is similar but generally presents after a latency period • Rhabdomyolysis may lead to AKI, but CK was normal and there was no myoglobin on UA. Question 13 A 54-year-old female has a 4-week history of LE edema and 5 kg weight gain. No hematuria or dysuria. She has a 14-year history of well controlled HTM and DM. She is on lisinopril, metformin, and simvastatin. Vitals: BP 135/85. Otherwise WNL. Exam: Retinal exam WNL. Bilateral 3+ LE edema Labs: Albumin 2.3, BUN 21, Creat 0.7. The following are normal: Complement, cryoglobulin, SPEP, PF, ANA, Hepatitis panel Urine: 24-hour protein 12 grams Kidney biopsy shows subepithelial deposits with foot process effacement. Which of the following is the most likely diagnosis? a) Diabetic nephropathy b) Membranous lupus nephritis c) Minimal change glomerulopathy d) Primary membranous glomerulopathy Key point: Patients are allowed to have 2 diseases • She has a long history of well-controlled diabetes and suddenly presents with nephrotic syndrome • Unusual progression for diabetic nephropathy • Membranous nephropathy is common in this age group • Secondary membranous associated with medications, malignancies, and infections. Why the other choices are wrong a) b) c) d) Diabetic nephropathy Membranous lupus nephritis Minimal change glomerulopathy Primary membranous glomerulopathy • This is an unusual progression for diabetic nephropathy, which generally progresses much slower • Membranous lupus is generally seen in the setting of systemic lupus • Minimal change disease might present similarly but would not have deposits on biopsy Question 14 A 65-year-old male is hospitalized following emergent surgery for perforated bowel. He has stage 4 CKD at baseline. He has HTN treated with amlodipine. Vitals: Temp 38.1, BP 150/95, pulse 102 Exam: Bowel sounds present, colostomy well perfused Serum K increases from 4.8 to 6.9, creatinine increases from 5.4 to 6.4. Bicarbonate is 17. Urine output has fallen to 50 mL over 8 hours and does not improve with fluids. ECG reveals peaked T-waves In addition to calcium and insulin-dextrose, which of the following is the most appropriate treatment? a) Furosemide b) Hemodialysis c) Sodium bicarbonate d) Sodium polystyrene sulfonate Key point: Manage hyperkalemia • Patient has hyperkalemia due to tissue necrosis • Will need to have potassium removed from his body • Options are limited without urine output. • After stabilization, hemodialysis is the best option to quickly remove large amounts of potassium Why the other choices are wrong a) b) c) d) Furosemide Hemodialysis Sodium bicarbonate Sodium polystyrene sulfonate • Lasix is unlikely to be effective in the setting of oligo-anuria unresponsive to fluids • Sodium bicarbonate is seldom effective in acidosis of chronic kidney disease for lowering potassium • Sodium polystyrene sulfonate is contraindicated in the setting of recent bowel surgery. The risk is increased with solutions containing sorbitol. Never give a kayexelate enema. Question 15 A 27-year-old female is evaluated for 4 months of hypertension. She feels well. History is otherwise unremarkable. BP 166/108, other vitals WNL Exam: Bruit in the right epigastric region. Otherwise WNL Labs: Renal panel and UA are unremarkable Renal angiogram shown at right Which of the following is the most appropriate next step? a) ACE inhibitor b) Calcium channel blocker c) PTCA d) Surgical revascularization Key point: PTCA is effective for fibromuscular dysplasia • Medial fibroplasia of the renal artery • Generally in young patients with sudden onset of hypertension • Angiography is the best way to diagnose FMD Why the other choices are wrong a) b) c) d) ACE inhibitor Calcium channel blocker PTCA Surgical revascularization • Drug therapy should not be attempted until after the results of PTCA are apparent. • Surgical revascularization is not first-line therapy but might be needed for difficult anatomy or those who do not respond to PTCA Question 16 A 59-year old man is evaluated for worsening kidney function. He was hospitalized since yesterday with a diabetic foot ulcer, which has been progressing for 4 weeks. He has CKD, HTN, and diabetes. He is on metformin, insulin glargine, lisinopril, and cefipime. Vitals: BP 160/100, otherwise WNL. BP 3 months ago was 130/78 Exam: Erythematous foot ulcer, 2+ LE edema Labs: Albumin 2.3, C3 and C4 decreased, creatinine 4.1 (BL=1.4) Urine: 25 RBC, erythrocyte casts. 24-hour protein 1.5 grams Which of the following is the most likely cause of AKI? a) Diabetic nephropathy b) IgA nephropathy c) Post-infectious glomerulonephritis d) Primary membranous glomerulopathy Key point: Diagnose post-infectious GN • Question stem notes a chronic infection • Low complement • Skin flora are common causes of postinfectious GN • Can manifest as a rapidly progressive glomerulonephritis (RPGN) or a more indolent course • Often progresses to advanced CKD, especially in adults Why the other choices are wrong a) b) c) d) Diabetic nephropathy IgA nephropathy Post-infectious glomerulonephritis Primary membranous glomerulopathy • Diabetic nephropathy progresses slower and is not associated with hematuria • IgA nephropathy is generally seen in association with a mucosal infection • Membranous nephropathy generally presents with more than 1.5 grams of protein and generally has minimal hematuria Question 17 A 51-year-old male is evaluated for 1 year of uncontrolled hypertension. There is no family history of HTN. He never smoked and has no other medical problems. He is on max doses of chlorthalidone, lisinopril, and amlodipine. Vitals: BP 160/94, pulse 76, remainder WNL Exam: Unremarkable. Lab: Creat 1.1, K 4.1, urianlysis WNL Which of the following is the most appropriate next step in management? a) Switch chlorthalidone to furosemide b) Switch lisinopril to aliskiren c) Obtain renal ultrasound with dopplers d) Obtain a plasma renin aldosterone activity ratio Key point: Hyperaldosteronism is a common cause of secondary HTN • This patient has resistant hypertension – BP remains elevated on 3 medications, one of which is a diuretic. • Hypokalemia is not consistently seen with hyperaldosteronism • High aldosteronism in the setting of relatively low renin suggests primary hyperaldosteronism • Confirm with a 24-hour aldosterone collection – High salt diet Why the other choices are wrong a) b) c) d) Switch chlorthalidone to furosemide Switch lisinopril to aliskiren Obtain renal ultrasound with dopplers Obtain a plasma renal aldosterone activity ratio • Switch to a loop diuretic can be helpful in patients with decreased renal function • Aliskerin is not more effective than lisinopril for blood pressure control • While RAS could also cause the patient’s symptoms, he has no other evidence of vascular disease Question 18 A 62-year-old male is hospitalized after being found down. He is confused but thinks he was in a fight a few days ago. He has HTN and hyperlipidemia, as well as alcohol abuse. Vitals: BP 165/85, pulse 102, temp 37.3 Exam: Multiple bruises, confused, orients to self only, membranes are dry, abdomen soft, no edema Labs: Hb 9.3, WBC 6.5, PLT 113K, BUN 85, Creat 4.5, K 5.1, HCO3 21, Phos 5.8, CK 15K Urine: FENA 5.7%, 3+ blood, 3-5 RBC, 5-10 WBC, few granular casts Which of the following is the most likely diagnosis? a) Acute interstitial nephritis b) Hepatorenal syndrome c) Abdominal compartment syndrome d) Pigment nephropathy Key point: Recognize pigment nephropathy as a cause of AKI • Commonly presents with a history of muscle trauma – Fight – Found down • Also with myotoxic drugs, exertion – Statins • Exacerbated by volume depletion • UA with positive heme but no RBC on micro Why the other choices are wrong a) b) c) d) Acute interstitial nephritis Hepatorenal syndrome Abdominal compartment syndrome Pigment nephropathy • Interstitial nephritis generally needs to have a history of an offending agent • There is no evidence of liver disease to suspect hepatorenal syndrome, and he is not hypotensive • Abdomen is soft on exam, making compartment syndrome unlikely Question 19 A 30-year-old female has 2 months of edema and weight gain. She has no history and takes no medications. Exam: BP 132/82. 3+ LE edema, otherwise unremarkable Labs: Albumin 3.1, BUN 19, creat 0.7, cholesterol 237, LDL 147, Hepatitis negative, ANA negative, RF negative, HIV negative Urinalysis: 3+ protein, estimated proteinuria 4 grams/day Kidney biopsy is consistent with membranous glomerulopathy. No evidence of mesangial involvement, glomerulosclerosis, or interstitial changes. Which of the following is the most appropriate treatment? a) ACE and statin b) Calcineurin inhibitor such as tacrolimus c) Corticosteroids d) Cyclophosphamide e) Mycophenolate mofetil Key point: Treat membranous nephropathy • She has primary membranous nephropathy • Risk factors for progression: – Age > 50 – Elevated creatinine – HTN – Glomerulosclerosis, interstitial changes – Persistent proteinuria for 6 months • ACE and statin can control her hypertension and hyperlipidemia of nephrotic syndrome Why the other choices are wrong a) b) c) d) e) ACE and statin Calcineurin inhibitor such as tacrolimus Corticosteroids Cyclophosphamide Mycophenolate mofetil • She has a low risk of progression to ESRD • Immunosuppressive therapy should be reserved for more aggressive cases • She might need in the future if she worsens • Remember to counsel young women regarding fetal risks with ACE and all immune suppressants, esp mycophenolate mofetil Question 20 A 48-year-old female is seen in the ER for fatigue, weakness, and dizziness. She was at an outdoor concert all day. She has a history of lupus without nephritis, as well as HTN. She is on hydroxychloroquine and HCTZ. She took ibuprofen several times today for myalgias. BP 97/52 lying, 90/45 standing. Pulse 108 Exam: No rashes or edema. Mucous membranes dry Labs: BUN 32, creat 1.2 (BL=0.7), FENA 1.2%, urinalysis benign Which of the following is the most likely diagnosis? a) Acute interstitial nephritis b) Acute tubular necrosis c) Lupus nephritis d) Prerenal azotemia Key point: Recognize the clinical and lab findings of prerenal azotemia • History of volume depletion • ACE and NSAIDs can reduce renal autoregulation – Increased risk for azotemia • FENA is >1.2%, but she is on HCTZ Why the other choices are wrong a) b) c) d) Acute interstitial nephritis Acute tubular necrosis Lupus nephritis Prerenal azotemia • There are no other exposures to suspect AIN – Also no WBC or eosinophils on UA • ATN generally displays muddy casts on UA. She is at risk for ATN if hypovolemia continues • Lupus nephritis would have hematuria or some other evidence of lupus activity. Question 21 A 45-year-old female comes to establish care. She is a recent immigrant from Romania. She has CKD and hypertension. Family history includes a cousin with CKD. She has no urinary symptoms, and takes captopril as well as occasional Ibuprofen BP 138/67, BMI 22, other vitals WNL Exam: Trace ankle edema, otherwise nonfocal Labs: creat 2.8, K 4.9, HCO3 21 Urinalysis: Rare granular casts, otherwise normal Renal ultrasound: Small kidneys without hydronephrosis Which of the following is the most likely diagnosis? a) Analgesic nephropathy b) Balkan nephropathy c) Hypertensive nephropathy d) IgA nephropathy Key point: Recognize Balkan nephropathy • Thought to be caused by aristolochia spp that grows with wheat • Results in regional pattern • Increased risk of urothelial cancers – Specific DNA adducts • Also can be caused by chinese herbal remedies Why the other choices are wrong a) b) c) d) Analgesic nephropathy Balkan nephropathy Hypertensive nephropathy IgA nephropathy • Analgesic nephropathy is unlikely without a history of heavy use. Also more likely to present with proteinuria • Hypertensive nephropathy unlikely with wellcontrolled hypertension • IgA nephropathy is unlikely without hematuria or proteinuria, and without a history of hematuria with URI Question 22 A 76-year-old female is seen in the ER with 1 day of nausea, vomiting, weakness, and confusion. She has fallen several times. BP 130/78, pulse 68, BMI 19 Exam: Frail appearing, no edema, JVP normal Labs: Albumin 3.6, BUN 10, creat 0.9, Na 120, K 3.6, Cl 83, HCO3 27, glucose 105, OSM 255 Urine: OSM 408, urinalysis normal Which of the following is the most appropriate treatment? a) 0.9% saline infusion b) 3% saline infusion c) Furosemide d) Tolvaptan Key point: Rapid treatment of symptomatic hyponatremia • The patient has SIADH with CNS symptoms and is in a state of rapid decline • 3% saline infusion is indicated • Aim to raise serum sodium by 4-6 in the first 24 hours • Use D5W if over-correction occurs Why the other choices are wrong a) b) c) d) 0.9% saline infusion 3% saline infusion Furosemide Tolvaptan • 0.9% saline would worsen the situation – Na 155 in 0.9% saline – People are not beakers • Lasix prevents concentration of urine and forces water excretion, which would help in time • Tolvaptan (V2 receptor antagonist) might be helpful but not acutely. Also is difficult to control the rate of correction with “vaptan” agents Question 23 A 60-year-old male comes into clinic as a new patient. He was diagnosed with DM 6 months ago at a health fair. No other history. He is on metformin. BP 145/94, BMI 29. Exam normal Labs: HbA1c 6.8%, BUN 10, creat 0.9, glucose 126 Urine: No protein on UA Echo: LVH Which of the following is the most appropriate next step? a) Add an ACE inhibitor b) Add a b-blocker c) Add a calcium channel blocker d) Add a diuretic e) Continue current regimen Key point: Prevent diabetic renal disease • He has hypertension in the setting of diabetes • Goal blood pressure 130/70 • RAS blockade can help prevent the onset of diabetic renal disease • Independent of BP control • Glomerular hyperfiltration in DM? Why the other choices are wrong a) b) c) d) e) Add an ACE inhibitor Add a b-blocker Add a calcium channel blocker Add a diuretic Continue current regimen • All the other agents listed would control the BP but would have no effect on long term renal function • Continuing with current care is not an option Question 24 A 66 year old female has AKI 4 days after colectomy for perforation. No intra-op hypotension but required 15 L of fluid. Urine output has gradually diminished and she is now oliguric. She received a single dose of tobramycin post-op (just for fun?) and now is on Vancomycin and Imipenem. Intubated and sedated. Temp 37.2, BP 91/52. BMI 35 Cardiopulmonary exam as expected, abdominal exam reveals a tense and distended abdomen with abdominal wall and LE edema. BUN 45, creat 2.9 (up from 0.9 post-op), FENA 1.5% Urinalysis with granular casts, no hematuria or pyuria Renal ultrasound: Normal kidneys without hydronephrosis What is the most likely cause of renal failure? a) Aminoglycoside nephrotoxicity b) Abdominal compartment syndrome c) Pre-renal azotemia d) Urinary onstruction Key point: Abdominal compartment syndrome is an important problem in the ICU • Patient is intubated and on paralytics • Tense abdomen likely from abdominal wall edema as well as bowel edema, fluid resuscitation • Exact pathophysiology of abdominal compartment syndrome causing renal failure is unknown Why the other choices are wrong a) b) c) d) Aminoglycoside nephrotoxicity Abdominal compartment syndrome Pre-renal azotemia Urinary onstruction • Aminoglycoside nephrotoxicity is unlikely with only a single dose • Pre-renal azotemia should have responded to fluids • Urinary obstruction was effectively ruled out with a normal renal ultrasound Question 25 A 54-year-old female is seen for recurrent kidney stones. She had gastric bypass 1 year ago and BMI has fallen from 38 to 33. She has passed 3 stones since surgery, none of which was sent for analysis. She also has diabetes and HTN, and is on metoprolol and glyburide. BP 125/78, remainder of exam is unremarkable Urinalysis: Many crystals (see below) Urine calcium and citrate are normal Which of the following is the most appropriate next step? a) Calcium carbonate supplements b) Chlorthalidone c) Potassium citrate d) Tamsulosin Key point: Oxalate stones can be seen after gastric bypass • Much less frequent with newer procedures • Fat malabsorbtion leads to decreased intestinal calcium, leaving unbound oxalate to be absorbed • Treatment is with supplemental calcium to complex with oxalate and lead to fecal elimination • Also increase fluid intake and decrease oxalate in diet • Also seen with crohn’s or any disease that results in small bowel resection • Cannot happen after colectomy Why the other choices are wrong a) b) c) d) Calcium carbonate supplements Chlorthalidone Potassium citrate Tamsulosin • Thiazides are useful in other types of calcium stones, by decreasing urine calcium • Potassium citrate is helpful in patients with low urine citrate • Tamsulosin and other a-blockers can help move stones through the ureter but will not help prevent future stones Question 26 A 71-year-old female is hospitalized for chest pain. She has DM, HTN, hyperlipidemia, and CKD. She is on lisinopril, rosuvastatin, furosemide, carvedilol, insulin, and aspirin. BP 118/50, pulse 70, cardiac exam is normal. Trace edema Labs: Hb 11, creat 3.1 (baseline), electrolytes normal Nuclear study shows reversible ischemia. Patient is scheduled for cardiac cath. Lisinopril is held prior to the procedure. Which of the following interventions will decrease her risk for contrast-induced nephropathy? a) Isotonic saline b) Isotonic saline with mannitol diuresis c) Oral hydration d) Prophylactic hemodialysis Key point: Better to prevent contract nephropathy • Contrast nephropathy incidence increases in those with pre-existing renal disease • Volume repletion is beneficial for prevention of nephropathy • No clear consensus on whether bicarb is better than normal saline • Decreased dye load, low-osmolar dye, etc • Don’t go squirting any dye into the renal arteries Why the other choices are wrong a) b) c) d) Isotonic saline Isotonic saline with mannitol diuresis Oral hydration Prophylactic hemodialysis • Mannitol diuresis is used to treat physicians, not patients. Best use of mannitol is in situations where increased osmolality is needed (CNS bleeds, etc) • Oral hydration is not more effective, and best to be fasting for a cath • Prophylactic hemodialysis will lower the creatinine but will not prevent the nephropathy. – Contrast dye dialyzes but we can’t remove it fast enough to make any difference Question 27 A 32-year-old male is seen for a new diagnosis of autosomal dominant polycystic kidney disease (ADPKD). His mother had ADPKD, HTN, ESRD on dialysis, and died of a stroke. The patient has HTN and takes metoprolol and losartan. BP 132/82, remainder normal Exam: Kidneys palpable and not tender Labs: Creat 1.2, estimated urine protein 150 mg/day Urinalysis: 5-10 RBC’s Which of the following in the most appropriate next step? a) 24-hour urine collection for protein b) Cerebral MR angiogram c) Genotype testing for ADPKD d) Noncontrast abdominal CT scan Key point: Patients with ADPKD are at risk of cerebral aneurysms • 8% incidence • More common in those with a family history of aneurysm rupture – Mother had a stroke • Also screen if patient has symptoms such as headache etc • Role of screening in patients with no family history of aneurysm is unknown Why the other choices are wrong a) b) c) d) 24-hour urine collection for protein Cerebral MR angiogram Genotype testing for ADPKD Noncontrast abdominal CT scan • Random UA indicated minimal proteinuria, so a 24-hour collection is not needed. Proteinuria is not usually seen in ADPKD. • Genotype testing is not needed. We know he has ADPKD. • Abdominal CT would be indicated if he had complaints of cyst rupture or infection