Gait analysis and Single-event Multi
advertisement

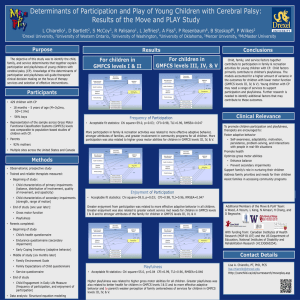
Gait analysis and Single-event Multi-level surgery The Melbourne Experience Richard Baker Professor of Clinical Gait Analysis Clinical scientist • Member of IPEM • Registered with HPC Me! • MA Physics and Theoretical Physics • PhD Biomechanical Engineering • 7 years Gait Analysis Service Manager Musgrave Park Hospital, Belfast • 9 years Gait Analysis Service Manager Royal Children’s Hospital, Melbourne Melbourne, Victoria Population Victoria Melbourne 5.5 million 4.1 million (Greater Manchester 2.6 million) 120 new cases of CP annually Royal Children’s Hospital Optimising gross motor function for children with CP Doing the simple things well Optimising gross motor function for children with CP • • • • • GMFCS (Gross motor classification system) Age Unit/bilateral involvement Motor type (CP like conditions) Level I Level II GMFCS Level III Level IV Level V Palisano et al. DMCN 1997 Revised and extended Palisano et al. DMCN 2008 Robin et al. JBJR-Br 2008 GMFCS and age Impairments and age Muscle Contracture Joint contracture Spasticity Bony deformity Botox ITB SDR SEMLS Weakness Exercise? Strenghtening? Diet? Physiotherapy and orthoses SEMLS • Minimum of one procedure at two levels (hip/knee/ankle) on both sides Typical SEMLS • • • • • Psoas recession Femoral derotation osteotomy Semitendinosus transfer Gastrocnemius recession Calcaneal lengthening SEMLS – who for • • • • • GMFCS I GMFCS II GMFCS III GMFCS IV GMFCS V rare (too good) rare (too bad) never SEMLS – Why? ICF WHO 2001 SEMLS – Why? • Improve gross motor function (not just walking) • Prevent deterioration • Increase activity and participation? • Improve quality of life? SEMLS – When? • After – maturation of gross motor performance – consolidation of skeleton (particularly feet) • Before – increased education demands – grumpy adolescence Pre-operative Processes • Spasticity management in early childhood • Surgeon decides surgery is required (8-10 years old) • Pre-op gait analysis to determine nature of surgery Pre-admission clinic • Admitted as “day case” • Child and family get to meet ward staff • Equipment arranged(orthoses, walking aids, other OT) • Rehabilitation discussed • Consultation with community physio In-patient In-patient • 7 days • No rehab • Appropriate lying 0-3 months Restricted mobility and therapy • Non weight-bearing 3 weeks • Cast change at 3 weeks • Orthoses delivered 6 weeks. • 6-12 weeks back on feet with Solid AFOs walking with frame or crutches • 12 weeks: 1st post-op video session 3-6 months Intensive therapy • Community based (home/school) • Move off frame/crutches • Extending walking distances • Maintain knee extension • 6 months: 2nd post-op video 6-12 months Routine therapy • Community based (home/school) • Maintain progress • Move off crutches/sticks • Move to hinged orthoses? • 9 months: 3rd post-op video session • 12 months: post-op gait analysis (outcome assessment) 12-24 months • Optimum function will not generally be achieved until into the second year. Video sessions • Standardised video recording and simplified clinical exam. • Review by specialist physiotherapist in person and surgeons by video. • Review progress (walking aids and orthoses) • Ensure knee extension. PIP fund INTERVENTION HOURS PROVIDED Botox – calves only 6 hours Botox – multilevel 12 hours Single level surgery – hemiplegia 6 hours Single level surgery – diplegia 12 hours Two level surgery – hemiplegia 12 hours Two level surgery – diplegia 18 hours Non-ambulant – hip surgery 12 hours SEMLS – hemiplegia (bony and soft) 30 hours SEMLS – diplegia (bony and soft) 70 hours Gait analysis • To identify impairments • Basis for planning surgery • Outcome assessment Impairment focussed assessment • Aims to identify impairments • Clearly link this to evidence from: – Instrumented gait analysis – Physical examination Report Report Report Movement Analysis Profile Movement Analysis Profile RCT OF SEMLS Thomason et al. JBJR-Am 2011 Participants • 6-12 years old, GMFCS II or III • 11 in SEMLS group • 8 in control group Results GPS scores for surgery and control groups (median and IQR) 20.0 surgery control GPS (degrees) 15.0 10.0 5.0 0.0 pre 12 24 GMFM scores for surgery and control groups (mean and 95% CI) 90.0 surgery control GMFM 80.0 70.0 60.0 50.0 pre 12 24 CHQ Physical function scores for surgery and control groups (mean and 95% CI) 100.0 surgery 80.0 control GMFM 60.0 40.0 20.0 0.0 pre 12 24 AUDIT OF SEMLS Rutz et al. ESMAC 2011 Participants • All patients having SEMLS 1995-2008 • 121 patients GMFCS II and III • 48 girls, 73 boys • Age 10.7+/- 2.7 GMFCS • • • • 113 (93%) no change in GMFCS 6 children from GMFCS III to II 2 children from GMFCS II to I No child deteriorated by GMFCS level • Children who improved were either marginal or had evidence of earlier deterioration MAP/GPS MAP components 40 Pre 30 Post 20 10 0 Predictors of GPS change • • • • • • • Age at surgery GMFCS GPS pre-op No. of procedures Adverse events Private health insurance Previous surgery GPS MAP 35 Mod Severe Very Severe Improvement in gait variable score (degrees) 30 25 20 15 10 5 0 -5 Pelvic Tilt Hip Flexion Knee Flexion Ankle d'flex Pelvic obliquity Hip Adduct'n Pelvic rotation Hip rotation Foot prog. GPS MAP 20.0 Improvement in GPS Short (1 year) Medium (5 years) 10.0 0.0 0.0 10.0 20.0 N = 47 -10.0 Pre-operative GPS 30.0 MAP 20.0 Short (1 year) Improvement in GPS Long (9 years) 10.0 0.0 0.0 10.0 20.0 N = 28 -10.0 Pre-operative GPS 30.0 Summary • SEMLS does not change GMFCS status (but might restore it) • It can help improve walking (GPS) and more general gross motor functions (GMFM) Summary • Evidence of mild deterioration over 12 months in absence of intervention • Optimal outcomes at 2 years, maintained for ten years • More involved children appear to have more to gain