Physiology of Skin Grafts
advertisement

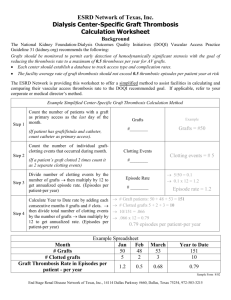
Physiology of Skin Grafts SKIN: Physiology & Function • Epidermis: – protective barrier (against mechanical damage, microbe invasion, & water loss) – high regenerative capacity – Producer of skin appendages (hair, nails, sweat & sebaceous glands) SKIN: Physiology & Function • Dermis: – mechanical strength (collagen & elastin) – Barrier to microbe invasion – Sensation (point, temp, pressure, proprioception) – Thermoregulation (vasomotor activity of blood vessels and sweat gland activity) SKIN: Physiology & Function • Immunological surveillance • Most skin is thin, hair-bearing, has sebaceous glands • Skin of palms/soles/flexor surface of digits is thick, not hair-bearing, no sebaceous glands • Vascular supply confined to dermis SKIN: Anatomy SKIN: Anatomy Skin Grafts: Classification • Full thickness skin grafts: - epidermis & full thickness of dermis • Split skin graft: - epidermis & a variable proportion of dermis - thin, intermediate or thick Skin Grafts: SSG Skin Grafts: Classification Autografts Isografts Allografts Xenografts Skin Grafts: “Process of Take” • Vascularity of donor site • Tolerance to ischaemia • Metabolic activity of the graft Skin Grafts: “Process of Take” • 4 Phases: – Fibrin adhesion – Plasmatic imbibition – Revascularization: Inosculation & capillary ingrowth – Remodelling: Revascularization & fibrous attachment in restoring normal histological architecture Skin Grafts: “Process of Take” • Plasmatic Imbibition: – Initially graft ischaemic (24 – 48 hrs) – Fibrin adhesion – Imbibition allows the graft to survive this period – ? Important for nutrition of graft – ? Stops drying out Skin Grafts: “Process of Take” • Inosculation & capillary ingrowth: – At 48 hrs – Through fibrin layer – Capillary buds from recipient bed contact graft vessels – Open channels (neo-vascularization) pink graft Skin Grafts: “Process of Take” • Revascularization & fibrous attachment: – Connection of graft & host vessels via anastomoses (inosculation) – Formation of new vascular channels by invasion of graft (neovascularisation) – Combination of old & new vessels (revascularisation) – Fibroblast proliferation: conversion of fibrin adhesion fibrous tissue attachment (anchorage within 4 days) Skin Grafts: “Process of Take” Skin Graft Take: Epidermis Days Histological changes 0–4 Epithelium doubles; crusting, scaling of epidermis; swelling of nuclei & cytoplasm; epithelial cell migration to surface; mitosis of follicular & granular cells 3 ++ mitotic activity in SSG not FTSG 4–8 Proliferation & thickening of epithelium (up to 7x) desquamation Week 4 Epidermis returned to normal thickness Skin Graft Take: Epidermis Day Histochemical changes 4 Increased RNA in basal cells, indicating protein synthesis 10 RNA returns to normal Skin Graft Take: Dermis • Fibrous component: Collagen Hyalinized early and progressively replaced with new fibres by 6 weeks; Turned over 3-4X faster than normal skin. Elastin Accounts for resilience; Days 3-7 fragment; Replaced 4-6 weeks. Extracellular matrix Proteins direct the behaviour of keratinocytes; Communication between keratinocytes & fibroblasts. Skin Graft Take: Dermis • Appendages: - sweating dependent on no. of transplanted sweat glands & degree of sympathetic reinnervation; will sweat like recipient site in FTSG only - sebaceous gland activity mostly in thicker grafts: SSG usually dry & shiny - hair grows from FTSG if well taken with no complications Skin Graft Healing • Initially white then pinkens with new blood supply • Lymphatic drainage by day 6 • Collagen replacement from day 7 to week 6 • Vascular remodelling for months Skin Graft Healing • Contraction: - shrinks immediately due to elastic recoil: 40%; medium SSG 20%; thin SSG 10%. - secondary contracture as heals: - FTSG remains same size after above - SSG will contract as much as possible; - more dermis = less contraction - ? Due to myofibroblasts shrinkage; – FTSG Skin Graft Healing • Reinnervation: – from margins to bed; – 4/52 to 2 years; – Depends on graft thickness and bed; – Uneventful healing leads to near normal 2PD; – Cold sensitivity can be a problem. Skin Graft Expansion • Based on principle that wounds reepithelialized from the periphery • Expansion provides larger areas from which epithelium can grow • Larger areas can be covered with less skin Skin Graft Expansion • Meshing - covers large area - easier to contour - fluid can drain through holes - cosmetic results less than ideal - various mesh ratio Skin Graft Survival • • • • • • Meticulous technique Atraumatic graft handling Well vascularized bed Haemostasis Immobilization No proximal constricting bandages Skin Graft Failure • • • • • • • • • • Haematoma Infection Seroma Mobility Inappropriate bed Dependency Arterial insufficiency Venous congestion Lymphatic stasis Technical – upside-down