Plastic surgery
Plastic surgery
definition, the Greek word plastikos means “ to form or mold ” ). Not limited to the skin and its adnexa, plastic surgery may encompass any area of the body.
While the details of various procedures are important, basic principles allow the plastic surgeon to solve unusual problems, to apply known procedures to other body parts, and to be innovative and change with the times and with developing technology. These broad principles can be applied to simple skin excisions or to complex free tissue transfers.
The first objective in analyzing a reconstructive problem is a correct diagnosis. The extent and type of missing tissue are assessed in order to formulate a plan for correction or reconstruction (Fig.
1). Planning the reconstruction by using a
“ reconstructive ladder ” illustrates a basic principle.
Innovations of plastic surgery
“ It is now Monday and we are in the second week of creation ” Peter Sloterdijk
Many promising new findings will not survive forever or be rejected after a while or even innovated by the original authors or others.
Many old techniques on the other hand have never been neglected: the ever-cited Indian Flap e.g. The coexistence of both: old and new – is the secret of good science.
Obtaining A Fine-Line Scar
The final appearance of a scar is dependent on many factors:
(1) the type of skin and location on the body.
(2) the tension on the closure.
(3) the direction of the wound.
(4) co-morbid conditions.
(5) the technique used for closure. Minimizing damage to the skin edges with atraumatic technique, debridement of necrotic or foreign material, ample irrigation of traumatic or contaminated wounds.
Intrinsic Factors
1.Age. Loss of elasticity combined with changes in the subcutaneous tissue, produce wrinkling, which makes scars in older individuals less obvious and less prone to stretching.
2.Type of skin should also be taken into account. Skin that is oily or pigmented, or both, produces more unsightly scars. Patients with fibroelastic diatheses are also prone to unpredictable healing and scarring.
3.Certain anatomic areas produce unfavorable scars that tend to become hypertrophic or widened. The shoulder and sternal area are notable examples. On the other hand, eyelid scars almost always heal with a fine-line scar.
4.Nutritional status can affect wound healing. Wounds gain strength less rapidly in the face of protein depletion. Vitamin A reverses the healing retardation caused by steroids. Vitamin C deficiency has long been known to cause scurvy, characterized by a failure of collagen synthesis. Zinc is required for epithelialization and fibroblast proliferation. Ferrous iron and copper are necessary for normal collagen metabolism.
5.Co-morbid conditions such as anemia can retard wound healing. .
Skin lines
The lines of tension in the skin were first noted by Dupuytren(1832).
Langer(1861) also described the normal tension lines of the skin, called “ Langer ’ s lines ” . Borges has written extensively on the subject and lists 36 descriptive terms for skin lines. He refers to the skin lines as “ relaxed skin tension lines ” (Fig. 2).
Excision of lesions is planned when possible so that the final scar will be parallel to the relaxed skin tension lines. Maximal contraction occurs when a scar crosses the lines of minimal tension at a right angle. Wrinkle lines are generally the same as the relaxed skin tension lines and lie perpendicular to the long axis of the underlying muscles. Scars can also be hidden in contour lines (i.e., lines of division) between body planes.
Factors determine the severity of suture markers
1.Time of removal of stitches .
2.diameter of the suture .
3. Relation to wound edges.
4. Region of the body.
5.Absence of infection.
6. Propensity for keloid.
Features of good scar
1- Fine line scar
2- absence of contour irregularities
3absence of pigmentary irregularities
4- no contracture or distortion
Methods of Excision
1.Simple Elliptical Excision
Lesions of the skin can be excised with elliptical, wedge, or circular excision. Simple elliptical excision is most commonly used . Dog ears may be corrected by extending the ellipse or removing excess tissue to close the incision in an L or Y shape.
2.Wedge Excision
Lesions located at or adjacent to free margins can be excised by wedge excisions. Onethird of the lower lip and one-fourth of the upper lip and eyelid can be excised with primary closure.
Lesions near the rim of the ear can be excised in a simple V shape and directly approximated. If excisions are large, stepping the limbs of the V at the helix will prevent notching.
3.Circular Excision
When preservation of the skin is required in areas such as the nose or the anterior surface of the auricle, the lesion can be excised in a circular manner and the defect closed with a skin graft or skin flap .
4.Multiple Excision Technique
Serial excision is frequently employed for large lesions such as congenital nevi. The inherent viscoelastic properties of skin are utilized, allowing the skin to “ stretch ” over time. These techniques allow wound closure to be accomplished with a shorter scar than if the original lesion was elliptically excised in a single stage.
Methods of suturing
A. interrupted.
B. Vertical mattress.
C. Transvers mattress.
D. Subcuticular .
E. Half – buried.
F. Continous.
skin graft skin graft consists of epidermis and some portion of dermis that is removed from its blood supply and transferred to another location.
history
• Reverdin 1 st skin transfere
Pollock autograft
Theish thin graft
Wolf full thichness
USES
Close any wound with good blood supply temporary closure control infection aesthetic replacement close donor site mucosal replacement
•
TYPES
Autograft
Xenograft(heterograft)
•
Allograft(homograft)
Skin Graft Types according to thickness skin graft may either be full or split thickness, depending on how much dermis is included. Split-thickness skin grafts contain varying thicknesses of dermis while a full-thickness skin graft contains the entire dermis. All such grafts contain adnexal structures such as sweat glands, sebaceous glands, hair follicles, and capillaries.
Skin Graft Donor Sites
Skin grafts can be taken from anywhere on the body, although the color, texture, thickness of the dermis, vascularity, and donor site morbidity vary considerably. Skin grafts taken from above the clavicles provide a superior color match for defects of the face. The upper eyelid skin can also be used, as it provides a small amount of very thin skin. Full-thickness skin graft harvest sites can be closed primarily. The abdominal wall, buttocks, and thigh are common donor sites for split-thickness skin grafts.
Choice of the type
STSG doubtful area contracture FTSG full thickness defects no contracture
Survival of a Skin Graft
The success of skin grafting, or “ take, ” depends on the ability of the graft to receive nutrients and, subsequently, vascular ingrowth from the recipient bed.
Skin graft revascularization or “ take ” occurs in three phases.
1 . serum imbibition and lasts for 24 to 48 hours. Initially, a fibrin layer forms when the graft is placed on the recipient bed binding the graft to the bed. Absorption of nutrients into the graft occurs by capillary action from the recipient bed.
2 . inosculatory phase in which recipient and donor end capillaries are aligned.
3 . the graft is revascularized through these “ kissing ” capillaries. Because the full-thickness skin graft is thicker, survival of the graft is more precarious, demanding a well-vascularized bed.
Four theories have been proposed for graft revascularization:
(1) There is neovascularization of the graft in which new vessels from the recipient bed invade the graft to form the definitive vascular structure of the graft
(2) communication occurs between existing graft vessels and those in the recipient site.
(3) there is a combination of ingrowth of new vessels and reestablishment of flow into existing vessels.
(4) the vasculature of the skin graft is made up, primarily, from its original vessels before transfer.
To optimize take of a skin graft, the recipient site must be prepared.
Skin grafts require a vascular bed and will seldom take in exposed bone, cartilage, or tendon devoid of its periosteum, perichondrium, or paratenon. There are exceptions, however, as skin grafts are frequently successful inside the orbit or on the temporal bone, despite removal of the periosteum. Close contact between the skin graft and its recipient bed is essential. Hematomas and seromas under the skin graft will compromise its survival and immobilization of the graft is essential.
INSTRUMENT
Knife Humby
Watson
Reese Drume type
Electrical dermatome
•
Causes of failure
1 . Haematoma
2 . Inadequate immolization
3 . Misevaluation of the wound
4 . Epidermal upside down
5 . Dependent position
character of skin graft
Primary contraction is the immediate recoil of freshly harvested grafts as a result of the elastin in the dermis. The more dermis the graft has, the more primary the contraction that will be experienced. Secondary contracture, the real nemesis, involves contraction of a healed graft and is probably due to myofibroblast activity. A full-thickness graft will contract more on initial harvest (primary contraction) but less upon healing (secondary contracture) than a split-thickness skin graft. The thinner the split-thickness graft, the greater the secondary contracture. Granulating wounds left to heal secondarily demonstrate the greatest degree of contracture and are most prone to hypertrophic scarring.
character of skin graft
The number of epithelial appendages transferred with a skin graft depends on the thickness of the dermis present. The ability of grafted skin to sweat depends on the number of glands transferred and the sympathetic reinnervation of these glands from the recipient site.
Skin grafts are reinnervated by ingrowth of nerve fibers from the recipient bed and from the periphery. Fullthickness grafts will have the greatest sensory return because of a greater availability of neurilemmal sheaths.
Hair follicles can also be transferred with the graft. Fullthickness skin grafts will contain more hair follicles than split-thickness skin grafts.
Unwanted squeals
Scaling
Milia
•
Special Techniques
Mesh graft Indication
Contraindication Dermal graft
Application Mucosal graft
Composite graft
SKIN FLAPS
Unlike a graft, a flap has its own blood supply. Although the skin graft is often simpler, there are cases in which a flap is required or may be more desirable. Flaps are usually needed for
1 .covering recipient beds that have poor vascularity;
2 .reconstructing the full thickness of the eyelids, lips, ears, nose, and cheeks
3.padding body prominences (i.e., for bulk and contour).
4 .Flaps are also used when it is necessary to operate through the wound at a later date to repair underlying structures.
5. muscle flaps may provide a functional motor unit or a means of controlling infection in the recipient area.
6. controlling of infection.
•
Disadvantages
1.Bulky.
2.Carry hair.
3.Multiple operations
4.Masked facial expression.
TYPES
1.Skin
2.Muscle
3.Omental
4.Fascial
5.Chondral
6.Periostial
7.Mixed
A skin flap consists of skin and • subcutaneous tissue that are transferred from one part of the body to another with a vascular pedicle or attachment to the body being maintained for nourishment.
Proper planning of a flap is essential to the success of the operation. All possible sites and orientations for the flap must be considered to be certain that the most suitable one is selected.
Blood Supply of the skin
1.Segmental
2.Anastimosing axial vessels
3.cutaneous vessels
A.Musculocutaneous perforators
B.Direct cutaneous vessels
Classification of skin flaps
A. According to vascular anatomy
1.Random flaps
2.Axial flaps a. peninsular b. island c. free
B. According to mobilization
1. Local a. Moved around fixed point
1.rotation
2.Transposition Rhomboid,dufourmental
3.Z plasty
4. Interpolated b.
Advancement
1. single pedicle
2. bipedicle
3. V-Y plasty
Advancement Flaps
All advancement flaps are moved directly forward into a defect without any rotation or lateral movement. Modifications are the single-pedicle advancement, the V-Y advancement, and the bipedicle advancement flaps.
The V-Y advancement technique has numerous applications. It is
•
The single-pedicle advancement flap is a rectangular or square flap of skin and subcutaneous tissue that is stretched forward.
Advancement is accomplished by taking advantage of the elasticity of the skin (Fig. 20A) and by excising Burow ’ s triangles lateral to the flap (Fig. 20B). These triangular excisions help to equalize the length between the sides of the flap and adjacent wound margins.
• not an advancement in the same sense as the forward movement of a skin flap just described. Rather, a V-shaped incision is made in the skin, after which the skin on each side of the V is advanced and the incision is closed as a Y (Fig. 21). This V-Y technique can be used to lengthen such structures as the nasal columella, eliminate minor notches of the lip, and, in certain instances, close the donor site of a skin flap.
•
2. Distant Flaps
A. Direct
B. Indirect carried either by
1. carrier
2. migration eg.caterpillar
Delay Phenomenon
It is a method of augmenting the surviving length of a flap by:
1. increase tolerance to ischemia
2. increase vessel no. &size
Requirement for survival
1. Size &location
2. presence of large bl. Vessel
3. delay method
4. absence of arteriosclerosing changes
5. absence of smoking absence
6. absence of trauma ,infection
&radiation.
Causes of failure
A. Intrinsic factors 1.inadequate bl.
2.AV shunts B. Extrinsic factors
1.infection
2.hypotention
3.compression
4.hematoma
5.smoking
Monitoring Viability
A. Clinical test 1.color &temp
2. capillary refilling
3.dermal bleeding
4.atropin absorption
5.histamin test B. Chemical
Flourescin dye injection C.
Instrumental 1.doppler
2.photoplethysmography
3.tissue PH,PO2,PCO2.
Measures to improve circulation
1. Postural assistance
2. Cooling 0-20`C
3. Leeches Hirudo Medicinalis
4.Dextran
5.Hyperbarric O2
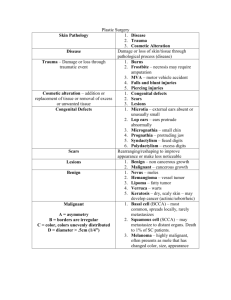
SKIN CANCERS
Skin cancer is the most common ca. in USA. it account for 1% of all ca. death.
Etiology:
1. Radiation
2.Chemical
3.Inherited
Premalignant Lesions
1. Actinic keratosis:20-25%
2. Bowen disease :intraepidermal SCC
3. Erythroplesia of Querate
4. Leakoplakia:15-20%
5. Keratoacanthoma :self-limiting SCC
6. Radiation Dermatitis
7. Xeroderma Pigmentosum
Basal Cell Ca.
. Consist of 65-80% of all Ca.
. 85% of them found on head& neck
. It is slowly growing but with massive silent penetration .
It arise from basal layer of epithelium
TYPES
1. Nodular ulcerative
2. Superficial
3. sclerosing(morphea )
Fire Feild 4.
Pigmented (fibroma like)
Rodent ulcer
Syndroms with multiple BCC
1. Xeroderma Pigmentosum
2. Basal cell nevus syndrome(Gorlin
Syndrome) palmar pits, sensetivity to light&bone cyst.
3. Bazex Syndrome
(atrophoderma,anhidrosis)
Treatment
1. Surgical depend on many factors
2. curettage& desiccation
3. cryosurgery
4. radiation
5. dermabrasion & chemical peel.
6. interferon alpha & 5 flurouracil
7. laser
Recurrent Basal Cell Carcinoma
Definite clinical signs that alert the physician to the possible presence of a recurrent skin cancer are as follows.
•
Scarring with intermittent or nonhealing ulceration 1 scar that becomes red, scaled, or crusted
An enlarging scar with increased telangiectasia in .
the adjacent area
3
Development of papule or nodule formation within the scar itself
.
4
Tissue destruction .
5
•
•
•
•
Squamous Cell Ca.
. Originate from atypical keratinocytes
. Predisposing factors
1.sun exposure UVB&UVA
2.radiation
3.arsenic
4.immunosupresion
5.HPV
6.tars&polycyclic hydrocarbons
TYPES
1. Slowly growing (Verrocous
,Exophytic)
2. Rapidly growing (more nodular
&indurated )
Differential Diagnosis
1. Actinic keratosis
2. Keratoacanthoma
3. Seborrhic keratosis
4. Wart or horn
5. BCC
Syndromes with SCC
1. Xeroderma Pigmentosum
2. Epidermodysplasia verrusiformis
3. Muirr-Torre syndrome.
Moh Micrographic Surgery
. By fixing the skin with ZnCl
. Advantage 1. preservation of normal tissue . 2. precise delineation of tumer
Malignant Melanoma (MM)
. 2 nd killer Ca. in male
. Arise from neural crest derived cells
Types
1. Superficial spreading (50-70%)
2. Nodular melanoma (10-20%)
3. Amelanotic melanoma .
4. Lentigo Maligna (Hutchison freckles) .
Indication of biopsy
A. Asymmetry
B. Border
C. Color
D. Diameter
Prognostic Factors
1. Depth (Clark Level).
2. Thickness (Breslow level).
3. Ulceration.
4. Type of primary lesion.
5. Satellistosis
6. Site a. Grave AGE b. Poor Border.
Differential Diagnosis
1. Dysplastic nevi
2. Pigmented BCC
3. Seborrhic keratosis
4. Blue nevi
5. Dermatofibroma
6. pyogenic granuloma
7. Kaposi sarcoma
Premalignant pigmented lesions
1. Large no. of nevi >100.
2. Gaint congenital nevus >10cm.
3. Dysplastic nevus
STAGES
Stage 1 :localize to skin
Stage 2 :spread to regional LN
Stage 3 :2& metastasis to distant skin
Management
1. Surgery
2. ERND elective regional LN dissection
3. Regional perfusion
4. chemotherapy
5. Interferon alpha 2b
Embryology
.CL :failure of mesenchymal fusion of nasofrontal &lateral processes at 4-7 weeks
. CP : failure of mesenchymal fusion of 2 palatine processes at 7-12 weeks
Classification (Stark-Kernahan)
A. Cleft of primary palate .unilateral
.bilateral
.median for each. complete
.incomplete
.microform B. cleft of secondary palate .complete
.incomplete
.submucous C. Cleft of primary & secondary palate
Etiology
1. Family history
2. reduction of facial mesenchyme
3. increase facial width
4. high position of tongue
5. oligohydramnion
6. drugs
7. infection, radiation ,alcohol
Early consideration
1. Feeding
2. airway Peirre-Robin syndrome
3. middle-ear disease
4.speech consideration
5.teeth problem
6. psychological
7. associated anomaly
Time of repair
CL Rule of 10 10 weeks
10g Hb
10 pounds(4.5Kg)
10,000 WBC CP 12-14 months
Aim of Rx
1. Normal appearance
2. Aligned teeth
3. swallowing
4.speech
5. hearing
Pressure sores
The terms pressure sore, decubitus ulcer, and bedsore have been used synonymously to refer to the tissue ulceration commonly seen in debilitated patients. The term decubitus comes from the Latin word decumbere, which means to
“ to lie down.
” Although this term may be appropriate for patients who are bedridden, it does not correctly describe the ulcers in patients who are mobile (i.e., ischial ulcers in wheelchairbound patients).
TABLE 1. Pressure sore staging
Stage Description
Stage I Skin intact but reddened for more than1 hour after relief of pressure
Stage II Blister or other break in dermis ± infection
Stage IIISubcutaneous destruction into muscle ± infection
Stage IV Involvement of bone or joint ± infection
Epidemiology
In general, approximately 9% of all hospitalized patients develop pressure sores. The occurrence seen in the acute care setting is as high as 11%. Commonly cited in all studies was their association with other medical problems, including cardiovascular disease (41%), acute neurologic disease (27%), and orthopedic injury (15%).
Pathophysiology
1. Pressure
2. infection
3. edema
Preoperative care
1. Nutrition.
2. Infection.
3. Releive of pressure mattress systems are designed to relieve pressure, including foam, static flotation, alternating air, low-air-loss, and air fluidized beds. The purpose of these beds is to more evenly distribute the patient ’ s weight to minimize pressure in any one area.
The Clinitron bed is designed with medical-grade optical beads fluidized with a constant flow of warm air.
4. spasm valium baclofen dantrolene rhizotomy
5. Contacture
Surgical Rx
1. Debridment
2. ostectomy
3. closure
complications
1. Recurrence
2. Carcinoma. Marjolin ulcer