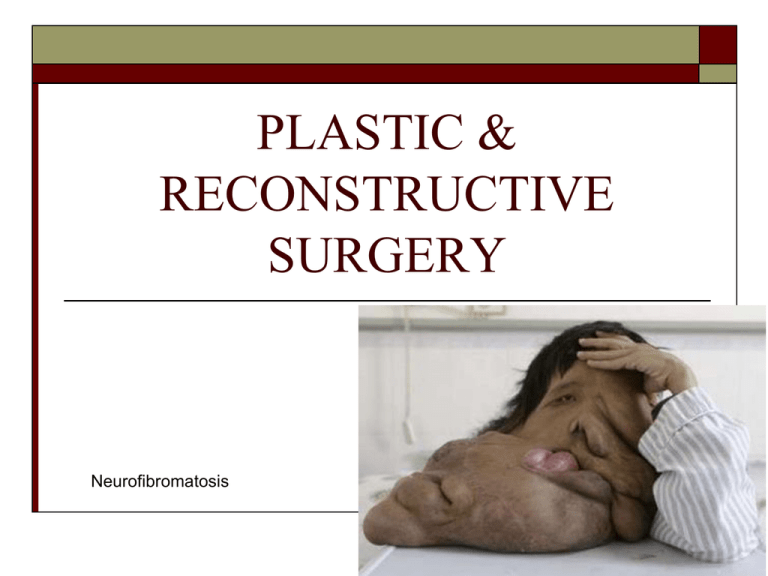
PLASTIC &
RECONSTRUCTIVE
SURGERY
Neurofibromatosis
Outline
Terminology
Anatomy of Skin and Hand
Pathology
Medications
Anesthesia
Supplies, Instrumentation, and Equipment
Considerations and Post-op Care
Procedures: Skin and Hand
Terminology
Dermatome-instrument used to incise skin, for thin skin transplants/can be
a tool for debridement
Dermis-inner sensitive (nerve rich), vascular (capillaries) layer of skin
Donor site-area of body used as source of a graft
Epidermis-outer, non-sensitive, non-vascular layer of skin
Erythema-small spot or reddened area of skin
Graft-tissue transplanted or implanted in a part of the body to repair a
defect
Plastic-”(plastikos) to mold or shape with one’s hands” (Caruthers & Price, 2001)
Plastic surgery-surgery performed to repair, restore, or reconstruct a body
structure
Recipient site-area of body that receives grafts
Terminology & Procedures
-plasty-restorative or
Fibrous Dysplasia
reconstructive
Abdominoplasty-abdominal wall
Blepharoplasty-eyelid
Cheiloplasty/Palatoplasty-cleft palate
Mammoplasty-breasts
Mentoplasty-chin
Rhinoplasty-nose
Rhytidectomy-face lift
W, X, Y or Z-plasty-skin (burns/scars)
Excision of Cancerous Neoplasms (basal cell, squamous cell, malignant
melanoma)
Lipectomies-liposuction
Microlipo-extraction
Collagen injection
Dermabrasion-removal of scars, tatoos, acne scars
Scar Revision
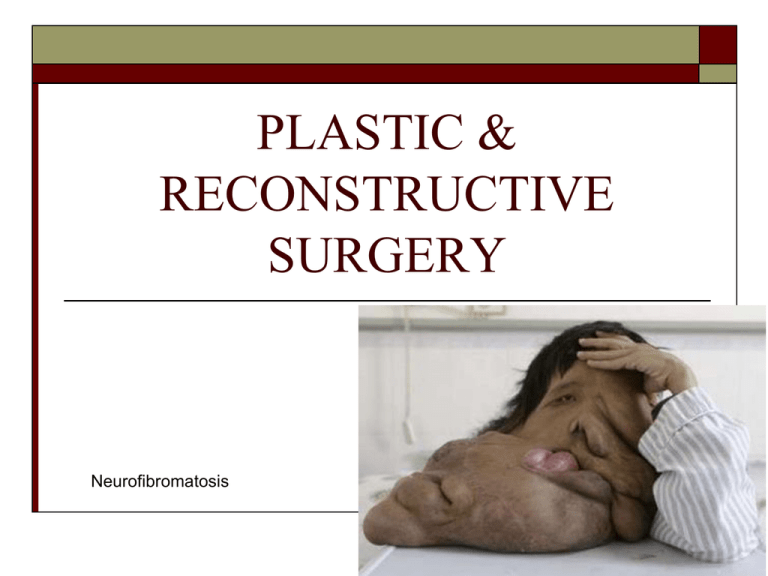
Purposes of Plastic & Reconstructive
Surgery
Dede Koswara
Correct congenital
anomalies or defects
Correct traumatic or
pathologic (disease)
deformities or
disfigurements
Improve appearance
(cosmetic)
Restore appearance
and function
Anatomy & Physiology
Multi-system/structure involvement
Non-specific anatomically unlike peripheral
vascular or orthopedics
Anatomy & Physiology
Integumentary System
Skin (cutaneous membrane)-outer covering of the
body
Function of:
Protection from external forces (sunrays)
Defense against disease
Fluid balance preservation
Maintenance of body temperature
Waste excretion (sweat)
Sensory input (temp/pain/touch/pressure)
Vitamin D synthesis
Integumentary System
Layers
2 main:
Epidermis (outer)
Composed of 4-5 layers called strata
Constantly proliferating (newly forming) and shedding (thousands a day)
Five week process
Dermis (inner)
Connective tissue
Composed of nerves, capillaries, hair follicles, nails, and glands
Two divisions:
Reticular layer-thick layer of collagen for strength, protection, and
pliability
Papillary layer-”named for papilla or projections the groundwork for
fingerprints” (Caruthers & Price, 2001)
Integumentary System
•Subcutaneous
Layer/Hypodermis
•Not
really a layer but
serves as an anchor for
the skin to the
underlying structures
•Composition:
adipose
(fat) & loose connective
tissue
•Purpose: insulation &
internal organ protection
Accessory Structures of the
Integumentary System
1.
2.
3.
Hair
Nails
Glands:
Sebaceous Glands
Sweat Glands/Sudoferous Glands
Merocrine Glands
Apocrine Glands
Ceruminous Glands
Sebaceous Glands
Oil (sebum) producing glands
Travels through ducts emptying in the hair follicle
Fluid regulation
Softens hair and skin
Makes skin and hair pliable
Activity stimulated by sex hormones
Activity begins in adolescence, continues throughout
adulthood, decreasing with aging
Sweat (Sudoriferous) Glands
Merocrine
Cover most of the body
Openings are pores
Secretion 1° water and
some salt
Stimulated by heat or
stress
Sweat (Sudoriferous) Glands
Apocrine
Larger than Merocrine glands
Located in external genitalia
and axillae
Ducts in hair follicles
Secrete water, salt, proteins,
fatty acids
Activated at puberty
Stimulated by pain, stress,
sexual arousal
Sweat (Sudoriferous) Glands
Ceruminous
External auditory canal
Secrete cerumen
(earwax)
No sweat glands
located in following
areas:
Some regions of
external genitalia,
nipples, lips
Palate
Roof of the mouth
Anterior portion = hard
palate
Composed of maxilla,
palatine bones, mucous
membrane
Posterior portion = soft
palate
Composed of muscle, fat,
mucous membrane
Terminates or ends at uvula
(opening of oropharynx)
Function of palate to separate
nose from mouth
Function swallowing and
speech
The Hand
Wrist
Palm
Fingers
Wrist (Carpus)
8 carpal bones
Arranged in 2 rows 4
each: distal and
proximal
Proximally articulate
with distal ulna and
radius
An easy way to remember the 8 carpal
bones
Some Lovers Try Positions
That They Can’t Handle
Scaphoid (Skay-foid)
Lunate
Triquetrum
Pisiform
Trapezium
Trapezoid
Capitate
Hamate
Palm (Metacarpus)
Metacarpals
5 per hand
Long, cylindrical
shaped
Fingers (digits)
Phalanges
14 per hand
3 phalanges
per finger or
digit
Numbered 1-5
beginning with
the thumb
Hand Joints
Metacarpals articulate with the phalanges
Diarthroses or freely-moveable joints
Synovial hinge joints
Metacarpophalangeal joints or MPJ referred
to as the (knuckles)
Nerves in the Hand
Branches of brachial
plexus supply
innervation to the
forearm and hand
Radial
Median
Ulnar
Radial Nerve (purple)
Runs with the radius
Sensation to forearm and small
section hand
Extensor muscles of
the forearm
Median Nerve (Blue)
2 branches
Innervates:
Skin of lateral 2/3 of
hand
Flexor muscles of the
forearm
Intrinsic muscles of the
hand
Ulnar Nerve (Yellow)
Innervates
Skin of
medial 1/3 of
hand
Some flexor
muscles of
hand and
wrist
Muscles and Tendons
of the Hand
40 muscles are
responsible for
movement of the hand,
wrist, and fingers
Most are on anterior
aspect of the hand
Anterior muscles are
for flexion
Fewer posterior
muscles are for
extension
Compartments or Tunnels
of the Hand
One main anterior
(palm)
Posterior or dorsally
there are 5
6 total compartments
Tendon Sheaths of the Hand
Finger and thumb tendons
are contained in a tendon
sheath
Serves to protect
Lined with synovium
Pulleys are attached to the
bones along the tendon
sheath
Serve to hold the tendon to
the bones they pass over
Hand Circulation
2 primary arteries
Brachial splits below the
elbow >radial and ulnar
arteries
Radial supplies lateral
aspect of arm
Ulnar supplies medial aspect
of arm
Join to form palmar and
superficial palmar arches
Names of hand veins
correlate with their arteries
Pathology
I. Burns
Injury resulting from heat,
cold, chemicals, radiation,
gases, or electricity that
causes tissue damage
Female patient who suffers with severe
burns on 70% of her body
Burn Classification
Depth
1st degree - involvement just epidermis
2nd degree - involvement to dermis
3rd degree - penetrates full thickness of skin
Can affect underlying structures
4th degree - char burns
5th degree - most of the hypodermis is lost, charring and
exposing the muscle (and some bone) underneath.
6th degree - the most severe form. Almost all the muscle tissue
in the area is destroyed, leaving almost nothing but charred
bone.
Damage to blood vessels, nerves, muscles, tendons, and
possibly bone density in 3rd thru 6th degree.
Burns Video - http://video.about.com/firstaid/Burns.htm this
video only covers 1st thru 3rd degree)
First Degree Burn
Superficial
Epidermis involvement
Redness or erythema
Healing rapid
Second Degree Burn
Partial Thickness Burn
Epidermis and Dermis
If Deepest Epithelial
layer undamaged will
heal
Infection can result in
damage same as third
degree burn
Blistering, pain,
moist/red/pink in
appearance
Third Degree Burn
Full-Thickness Burn
Epidermis and Dermis destroyed
Extends to subcutaneous layer
and structures
Requires skin grafts to heal
Dry, pearly white, charred
surface (eschar)
No sensation
Fourth Degree Burn
Damage to bones,
tendons, muscles, blood
vessels, and nerves
Charring
Electrical burns most
common
Extensive skin grafting
required
Patient might survive
and/or limb might be
saved.
5th and 6th Degree Burns
Fifth and sixth degree burns are most often
diagnosed during an autopsy. The damage
goes all the way to the bone and everything
between the skin and the bone is destroyed. It
is unlikely that a person (or limb) would
survive this type of injury.
Healing
Remember that first-degree burns require
three to five days to heal, second-degree burns
take two to six weeks to heal, and third- and
fourth-degree burns take many weeks to
months to heal.
Lund-Browder Method (perdriatrics) vs.
Rule of Nines (everybody)
Lund-Browder Method used in the evaluation of all
pediatric patients.
The Lund-Browder system
uses fixed percentages for
the feet, arms, torso, neck,
and genitals, but the values
assigned to the legs and
head vary with a child's
age.
Is more accurate but also
more difficult to use.
Burn Assessment -Rule of Nines
Rule of Nines
Increments of 9% BSA (body surface area)
Head and Neck (front and back)= 9%
Anterior Trunk = 18%
Posterior Trunk = 18%
Upper Extremity (front & back)= 9%
Lower Extremity x 1(front & back)= 18%
Perineum = 1%
Burn Surgical Intervention
Debridement - medical term referring to the removal
of dead, damaged, or infected tissue to improve the
healing potential of the remaining healthy tissue.
Skin Grafting
The Story - Milwaukee Journal Sentinel - The
Phoenix Man - George Bennett – 70% burn underground tank
Skin Grafts
Autograft - taken from part of the patient’s body
Homograft or Allograft– graft taken from same
species as recipient (cadaver)
Stored in a tissue bank
Heterograft or Xenograft – Taken from one
species and used on another species (pigskin/porcine
skin or cowskin/bovine)
Synthetic Skin
These means reduce fluid loss and protect the wound
Autografts
Classified by the source of their vascular supply and
tissue involved
Factors for determining choice of grafting method:
Location of defect
Amount of area to be covered
Depth of defect
Underlying tissue involvement at defect
Cause of defect (trauma, disease, or heredity)
Autografts
(FTSG) Full Thickness Skin Graft
Consists of epidermis and all of the dermis
May include greater than 1 mm of the subcutaneous layer
Because is a deep excision at the donor site, limited to smaller areas of
grafting (face, neck, hands, axillae, elbow, knees, feet)
Especially used for covering squamous cell or basal cell carcinomas
Donor site must be closed
Cannot reuse donor site
Excised by a skin graft knife
Prevent contraction of a wound better than a split-thickness graft
Autografts
(STSG) Split-Thickness Skin Graft
Involves removal of epidermis and dermis to a depth
of up to 1mm
Can be used over large body surfaces (back, trunk,
legs)
Donor site regenerates quickly and can reuse in
about 2 weeks if it has been properly cared for
Graft excised with a dermatome
Graft can be stretched or enlarged by a skin graft
mesher
Dermatomes
Used to remove STSG
Brown - oscillating blade
Padgett-Hood-rotating
blade housed in drum
Powered by nitrogen or
electricity
Hall
Reese
Can be hand held
Dermatome
Connect blade to dermatome before passing off the power cord
Test in a safe place
Blades are disposable
Take care with blades
Surface of blade protected with a guard (are 4 sizes)
Secure blade and guard with screwdriver
Guard should not cover the cutting edge of blade
Dermatome
Graft thickness (depth) determined by small lever on side of dermatome
(in tenth of a millimeter increments)
Set at 0 before procedure and after changing blades
Adjust per surgeon directions or surgeon may adjust
Width of graft determined by gaps in edges of plate that are one to four
inches
Donor Site
Covered with a mesh-like medicated dressing
Graft Care
Do not allow to dry out
Place in a basin with small amount of warm
saline until ready to use
Mesh Graft Device
Manually operated/roller like device
Used with a split thickness skin graft to expand (meshing)
the size of the skin graft
Skin graft is placed on a plastic derma-carrier, which holds
the graft flat prior to placing in the mesh graft device
If more than one graft used, each is placed on its own dermacarrier
Derma-carriers come in various sizes (sized in ratios)
If ratio on derma-carrier says 3:1, means graft will cover
three times the area it would have if not meshed
Meshing creates netted effect
When skin graft placed on site being grafted, epithelial tissue
will grow in between the slits
Mesh Graft Device
Graft Care Post Placement
Will likely be secured as it needs to stay in place until healing can ensue
May use a pressure type dressing
Anything wrong here?
II. Acne
Inflammatory disease of skin
Formation of pustules or pimples
Face, neck, upper body affected
Related to stress, diet, and hormonal activity
Bacteria can invade and cause pits and scars
Surgical intervention requires removal of pits
and scars via dermabrasion
III. Aging
Elastic fiber number decrease
Lost adipose tissue
Collagen fiber loss, slows healing
Wrinkling and sagging result
Surgical intervention = Conservative
nonsurgical intervention to invasive surgical
intervention
Rhytidectomy = “face-lift”
IV. Sun Exposure
Sunlight exposure thickens epidermis and
damages elastin
Damaged elastin allows for formation of premalignant and malignant cells
Prevention best (sunscreen)
Can resurface skin pharmaceutically or
surgically
No sunscreen can lead to Melanoma.
Melanoma
A form of skin cancer that begins in melanocytes (the cells that
make the pigment melanin). Melanoma usually begins in a mole.
The most dangerous type of skin cancer.
It begins as a dark skin lesion and may spread rapidly to other areas
on the skin and within the body.
HOW DO I KNOW IF I HAVE MELANOMA?
The ABCD’s
A- Asymmetry. If the mole is asymmetrical, it is potentially
cancerous.
B- Border. If the mole has an irregular border, it could be
cancerous.
HOW DO I KNOW IF I HAVE
MELANOMA?
C- Color. If the mole has more than one color
or is blue, pink, or white, it could be
cancerous.
D- Diameter. If the mole has a diameter of
larger than 6 mm, it could be cancerous.
V. Eyelids
Blepharochalasis = loss of muscle tone or relaxation
of the eyelids
Causes wrinkling and thinning
Poor results surgically
Dermachalasis = relaxation and hypertrophy of
eyelid skin
Bags under the eyes
Easily corrected surgically
Ptosis = eyelid drooping
Muscle shortening repairs this
VI. Neoplasms
Any new or abnormal growth
May be benign, pre-malignant, or malignant
Caused by exposure direct or indirect to
chemicals or the sun
Removal surgically can be chemical, laser, or
minor surgical
Neoplasm Example
VII. Nose and Chin
Rhinoplasty - reshaping the nose
Can be done with other nasal procedures to
restore upper respiratory function post-trauma
Mentoplasty – reshaping the chin
VIII. Cleft Lip & Palate
Cleft = split or gap between
two structures that normally
are joined
Cheiloschisis = cleft lip (hair
lip) -Say cheiloschisis
Palatoschisis = cleft palate
- Say palatoschisis
May see alone or in
conjunction
May be unilateral or bilateral
Surgical intervention =
cheiloplasty and palatoplasty
IX. Breasts
Gynecomastia
Liposuction
Cancer
Congenital deformity
Aesthetic reasons
Medical reasons
Mammoplasty
X. Abdomen
Abdominoplasty or tummy tuck
Thinning of abdominal fat and tightening of
abdominal muscles
Removing fat and excess skin from mid to lower
abdomen
Can do in addition to liposuction
Panniculectomy = removal of fat apron in obese
patients
Hand Pathology
1. DeQuervain’s Disease
Stenosis/inflammation
of tendons in first
dorsal wrist
compartment
Treatment
conservative with antiinflammatories or
surgical (rare
recurrence after
surgery)
Hand Pathology
2.
Trigger Finger
Stenosis of digital
tendons
Surgical intervention
needed if digit
becomes “locked”
Hand Pathology
3.
DuPuytren’s
Disease
Related to traumatic
injury
Contracture of palmar
fascia
May be seen as a
nodule in the palm,
dimpling or pit in the
palm, or fibrous cord
from palm to fingers
Surgical intervention
warranted if movement
and function are
impaired
Hand Pathology
4.
Ganglion Cyst
Benign lesion in
hand or wrist
Filled with
synovial fluid
coming from a
tendon sheath or
joint
Results from
trauma or tissue
degeneration
May aspirate
Surgical removal
Recurrence 50%
Hand Surgery
5.
Rheumatoid Arthritis
(RA)
Disease that attacks the
synovial tissues
Most common connective
tissue disease
Loss of joint function
Anti-inflammatory meds
treat
Surgical intervention
required to stabilize a
weakened joint or replace
a damaged structure
Hand Surgery
6.
Hand Trauma
Cuts
Sprains
Fractures
Burns
Crush injury
Amputation
Reimplantation of digits is
a microvascular procedure
Goal:
Restoration of
appearance
Restoration of function
KEY GOAL =
FUNCTION
Medications
Local anesthetics
Hemostatics
Mineral oil (for skin with dermatome use)
Antibiotic irrigants and ointments
All solutions must be warmed especially on
burn patients
Supplies
Basin pack
Beaver blades
Knife blades of surgeons choice
Medicine cups
Mineral oil
Sterile tongue blade used in conjunction with dermatome to stretch skin as
graft being removed
Derma-carrier
Drains of surgeon’s choice
Needle tip cautery electrode
Marking pen
Ruler or calipers
Luer lock control syringes
25 and 27ga needles
Instrumentation
Basic Plastics Tray
Basic Plastics Tray:
Towel clips
Micro mosquitoes
Hemostats
Allises
Littler, Iris, tenotomy scissors
Small metz fine and blunt tipped
Small mayo straight and curved
Bandage scissors
NH fine and crile-wood
Adsons smooth and with teeth
Adson-brown, bishop-harmon, debakey
Skin hooks single and double pronged
Senn retractors, Army-Navy, Spring Retractors
#3, #7,knife handles, beaver handle
Freer, small key elevators
Frazier suction tip 8F angled with “finger cut-off” valve
Nasal Instruments
Rhinoplasty/Nasal tray
Vienna Nasal speculums
Single skin hooks
Cottle or Joseph double prong skin hooks
Cottle knife
Cottle or Fomon Retractor
Cottle osteotomes (4, 7, 9, 12mm)
Ballenger chisel
Ballenger swivel knife
Joseph nasal bayonets, right and left
Freer septal chisels curved and straight
Joseph rasp or Double ended Maltz rasp
Cushing Bayonet forceps with teeth
Jansen Bayonet dressing forceps
Takahashi Forceps
Cottle cartilage crusher
Abdominoplasty Instruments/Supplies
Basic Plastic Set
Fiberoptic Retractor Set
Abdominal retractor tray (deavers,
richardsons, etc.)
Lap sponges
Umbilical template
Abdominal drapes (universal) or Laparotomy
Extension blade for the cautery
Cheiloplasty & Palatoplasty
Instruments/Supplies
Basic plastic tray
#15 blade
Oral instruments
Mouth Gag (Jennings/Davis/McIvor)
+ assorted blades
2x2 gauze for dressing
Mammoplasty Instruments & Supplies
Basic Plastic Tray
Minor Tray
#15 blades
Local with Epinephrine
Control syringes and local needles
Fiberoptic retractor set
Extension tip available for cautery
Laparotomy sponges
Chest drapes (universal or laparotomy)
Suture of surgeon preference
Dressing
Hand Supplies
Basin pack
Basic pack
Extremity sheet or hand/arm drape
Split sheet
Half sheet for lower part of body
#15 blades
Stockinettes
Esmark
Tourniquet and padding for (cast type)
Suture of preference
Anesthetics of choice (local)
Control syringes and 25/27ga. hypo needles
Dressing of surgeon choice
Elastic bandage
Hand Instruments
Minor orthopedic tray
Minor plastic tray
Small vascular instruments (re-implantations)
Metacarpal retractors
Pediatric deavers
Hand Equipment
Sitting stools
ECU
Suction
Hand table
Tourniquet
Tower Equipment including insufflator
Positioning
Depends on area being operated on
Care to padding depending on which position
used
Extreme care with a burned patient with
moving
Guard all IV lines, trach tubes, ET tubes
Do not delay transport to the OR
Prepping
Colorless solution preferred if using skin graft
so skin color can be seen
Donor and graft sites prepped separately
Solutions used should be warmed
Prep gentle and about 3 minutes (less time
than normal skin)
Keep patient covered with warm blankets
until ready to prep, keep blankets on as much
area as possible
Special Considerations
Strict aseptic technique
Death related to septicemia and pneumonia in severely
burned patients
Environmental temperature should be geared to prevent
hypothermia, prevent microbial invasion, and aid in the
healing process
Body temp will be monitored throughout on burn patients
with a rectal, esophageal, or tympanic probe
Patient will be in isolation post-op
May go to hyperbaric unit to promote healing
I & O carefully monitored (urine and blood loss)
Post-Operative Care
Maintain asepsis until all dressings are
secured prior to removal of drapes