Rheumatic Diseases and the Eye
advertisement
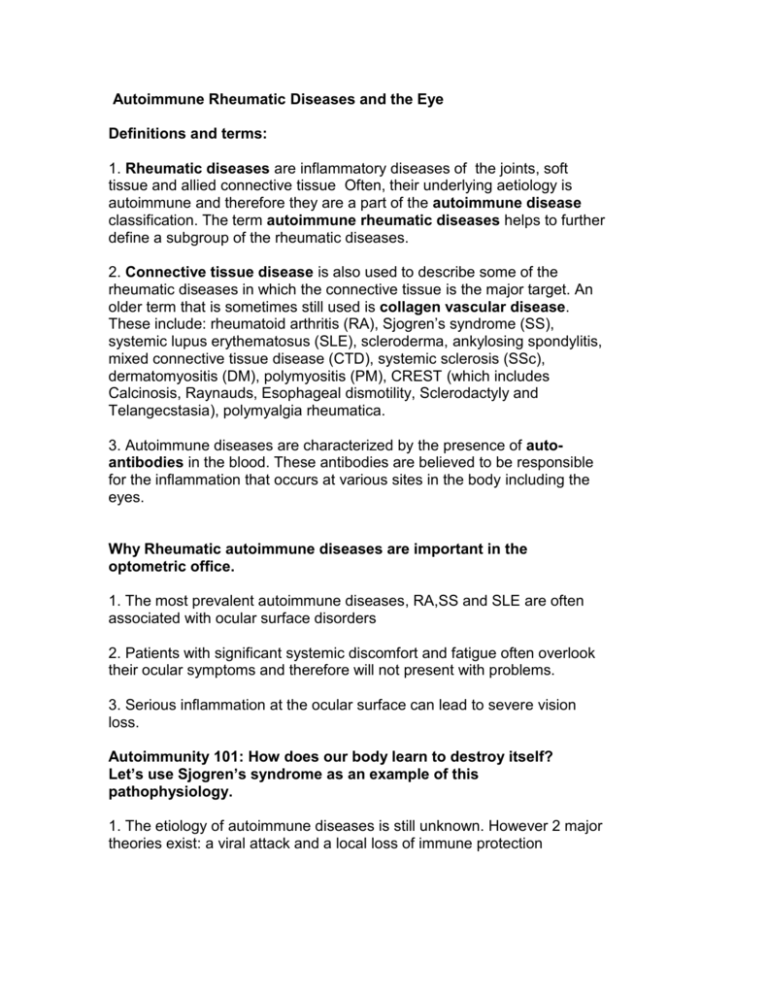
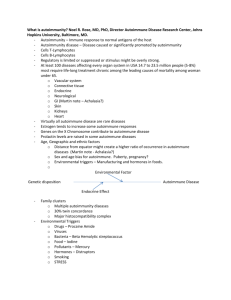
Autoimmune Rheumatic Diseases and the Eye Definitions and terms: 1. Rheumatic diseases are inflammatory diseases of the joints, soft tissue and allied connective tissue Often, their underlying aetiology is autoimmune and therefore they are a part of the autoimmune disease classification. The term autoimmune rheumatic diseases helps to further define a subgroup of the rheumatic diseases. 2. Connective tissue disease is also used to describe some of the rheumatic diseases in which the connective tissue is the major target. An older term that is sometimes still used is collagen vascular disease. These include: rheumatoid arthritis (RA), Sjogren’s syndrome (SS), systemic lupus erythematosus (SLE), scleroderma, ankylosing spondylitis, mixed connective tissue disease (CTD), systemic sclerosis (SSc), dermatomyositis (DM), polymyositis (PM), CREST (which includes Calcinosis, Raynauds, Esophageal dismotility, Sclerodactyly and Telangecstasia), polymyalgia rheumatica. 3. Autoimmune diseases are characterized by the presence of autoantibodies in the blood. These antibodies are believed to be responsible for the inflammation that occurs at various sites in the body including the eyes. Why Rheumatic autoimmune diseases are important in the optometric office. 1. The most prevalent autoimmune diseases, RA,SS and SLE are often associated with ocular surface disorders 2. Patients with significant systemic discomfort and fatigue often overlook their ocular symptoms and therefore will not present with problems. 3. Serious inflammation at the ocular surface can lead to severe vision loss. Autoimmunity 101: How does our body learn to destroy itself? Let’s use Sjogren’s syndrome as an example of this pathophysiology. 1. The etiology of autoimmune diseases is still unknown. However 2 major theories exist: a viral attack and a local loss of immune protection 2. Viral etiology: The ocular mucosal tissues are exposed to all forms of viral species. Viruses can travel from the surface to invade the lacrimal gland could certainly cause an autoimmune response. Changes in cytokine expression of lacrimal acinar cells would activate both T and B immune cells that are present in the healthy lacrimal gland. 3. Failed local immunity: Inflammation in and around the lacrimal gland from any cause could create a breakdown in immune protection. Sjogren’s syndrome, then, becomes a disease of failed local immunity as stimulated acinar cells become antigen presenting cells. MHC class II positive epithelial cells initiate an autoimmune response by presenting their own internal proteins on their surfaces to reactive T lymphocytes and thus activate these cells at the local level. This form of inflammation has been noted in several ocular conditions including corneal transplant rejection, uveitus and proliferative vitreoretinopathy. Dendritic, T and B cells also play a role in this process. 4. This same sort of pathophysiology applies to our understanding of RA and SLE with different organs being affected. Epidemiology of rheumatic autoimmune diseases 1. It is generally believed that rheumatic autoimmune diseases affect 5% of the population. The most prevalent of these diseases are RA, SS and SLE . There is a predominance of women affected by these diseases. 2. A recent CDC analysis demonstrated that the prevalence of RA has lessened and that the prevalence of SS may be higher than previously thought in the US. This review of surveys suggests that up to 3.1 million adult Americans (approximately 1%) suffer from Sjogren’s syndrome. It is also believed that 9 out of 10 of them are women. What we need to do in our eye examinations 1. A thorough history that identifies autoimmune disease if it exists. 2. A series of questions of those patients presenting with prolonged and significant dry eye or acute red eyes that might identify autoimmune disease. 3. If suspicious, a look at the hands of patients with suspected or confirmed autoimmune disease to assess joint inflammation. 4. An observation of the tongue of those patient in whom you suspect Sjogren’s syndrome. 5. Extra attention to the ocular surface and anterior chamber to assess: corneal staining with fluorescein, conjunctival staining with lissamine green or rose bengal, Schirmer testing, close observation of episclera and sclera, anterior chamber observation to rule out cell and flare. 6. Findings of Schirmer scores <= 5mm in 5 min in 1 eye and/or total staining scores of <= 4/9 in at least 1 eye suggests the possibility of primary or secondary Sjogren’s syndrome. Assess the dry mouth status and refer where appropriate 7. Significant peripheral corneal staining with inflammation and/or cell and flare requires immediate attention with topical and/or oral steroids. Hospitalization may be required. The mechanism of ocular involvement in rheumatic autoimmune diseases. 1. The cornea: alterations in epithelial phenotype as dry eye features such as reduced tear flow, increased osmolarity and inflammation cause disease. This is seen as staining of the ocular surface 2. The cornea: peripheral corneal melting caused by acute autoimmune inflammation near the limbus. This is likely a vasculitis which is a serious sign of increased and acute complications of autoimmune disease 3. The conjunctiva: changes is cell phenotype as dry eye factors cause trauma. MUC1 and MUC16 show increased expression in SS. 4. Scleritis and episcleritis: local autoimmune inflammation 5. Uvea: the systemic aspects of chronic autoimmune disease is classically displayed in the anterior chamber where cells and proteins from the uveal blood vessels are seen in the anterior chamber. More serious are the posterior uveitis cases. Treatment and Management 1. If autoimmune disease is suspected refer to rheumatology or ask the family practitioner for specific antibody testing RA, Ro and La. 2. treat the dry eye. Explain the problem and that it will not affect long term visual function, prescribe lubricants, gels, anti-inflammatories, nutritional and supplement counselling, eye protection, humidification and general health. 3. Treat corneal melts immediately with referral when necessary. Hospitalization with IV steroids may be needed. 4. Treat the episcleritis and scleritis topically with steroids and frequent followups 5. Treat iritis with your usual protocol: cycloplegia, steroids. Uveitis requires a referral and possible invasive treatment. Chronic rheumatic autoimmune diseases are a large part of optometric care. All patients with RA, SLE, SS etc should be queried for possible anterior segment involvement. All red, sore and dry eyes should be analyzed with the possibility of systemic autoimmune conditions in mind.