201109 Critical care conference
advertisement

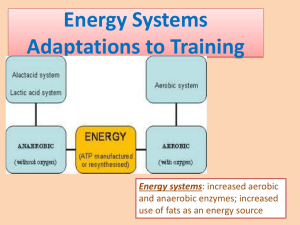
Intensive care conference: management of acid-base disorders with CRRT --2011 International Society of Nephrology 主講人: R2 顏介立 Introduction 1. acid-base homeostasis challenge in ICU 2. Focus on CRRT (Continuous renal replacement therapies ) in critical patient with AKI 3. hypercapnic acidosis and lactic acidosis for example CRRT (Continuous renal replacement therapies ) - called "go slow dialysis” - The major advantage of continuous therapy is the slower rate of solute or fluid removal per unit of time - CVVHD (Continuous veno-venous hemodialysis ) - CVVHF (Continuous veno-venous hemofiltration ) - CVVHDF CRRT (Continuous renal replacement therapies ) Hypercapnic acidosis 1. Cause - Increase CO2 production or decrease CO2 elimination 2. Physiological compensatory: lung: hypercapnia stimulate cental and paripheral chemoreceptors=>increase ventilation Hypercapnic acidosis 2. Physiological compensatory: kidney: 3-5 days (in animal model) ** but this mechanism is limited in AKI patient Hypercapnic acidosis 3. Management - - ALI/ARDS treatment: CO2 retention permission =>low tidal volume(4-6ml/kg) and low pressure(<30) =>maintain adequate oxygenation =>PaCO2=66.5mmhg/ PH decrease to 7.2 Acidosis would “well tolerated” if fair tissue perfusion and oxygen Hypercapnic acidosis 3. Management - Hypercapnic acidosis controversies: Advantage: improve arterial and tissue oxygenation, reduce oxidative stress, anti-inflammatory effect Disadvantage: vasodilating effect, increase capillary permeability (may worsen brain edema) =>ICH may cause myocardial depression, pulmonary hypertension Conclusion: patient with advanced age and multiple comorbidities, lung-protective stragegies may disadvantage Hypercapnic acidosis 3. Management sodium bicarbonate : - - Worsen exisiting hypercapnia Worsen heart failure due to volume expansion, hyperosmolality, decrease ionized calcium plasma concentration Hypercapnic acidosis treat by sodium bicarbonate is not recommended unless metabolic acidosis coexist Hypercapnic acidosis 3. Management -Intermittent hemodialysis: rapid flux of bicarbonate => excess CO2=> required hyperventilation -CRRT: much slower buffer delivery=> correct combined respiratory and metabolic acidosis by CRRT in case reports. Hypercapnic acidosis 3. Management - - Convective hemofiltration: use hemofiltration with replacement fluid contain NaOH can remove half of CO2 production =>50% reduction in minute ventilation and keep PaCO2 level 35-38 with stable blood PH CVVHF may an effective adjunctive treatment for acidosis in respiratory failure patient => avoid intubation and ventilator induced ALI or infection Lactic acidosis 1. pathophysiology: - Pyruvate: precursor of lactate PDH Lactic acidosis 2. Classification of lactic acidosis: - Type A: inadequate oxygen supply Type B: dysregulation of metabolism rather than hypoxia B1: liver disease, malignancy B2: drug induced: metformin, aspirin, propofol…… B3: congenital - Sepsis induced lactic acidosis - Lactic acidosis 3. Clinical application of lactate: - Lactate acidosis is related to high mortality - Lactate is a prognosis indicator surviving sepsis campaign regard lactate level>4mmol/L need aggressive treatment protocols - Treat underlying disease Lactic acidosis 4. Treatment of lactic acidosis: - Treatment underlying disease - Sodium bicarbonate: - may worsen oxygen delivery, increase lactate production (especially when hypoxia=>induce glycolysis), decrease portal vein flow The surviving sepsis campaign recommended hold sodium bicarbonate unless ph<7.15 -two randonmized trials Lactic acidosis 4. Treatment of lactic acidosis - CRRT Type A lactic acidosis: small observational studies showed efficient management of severe type A lactic acidosis=> CRRT vs sodium bicarbonate infusion Lactic acidosis 4. Treatment of lactic acidosis - CRRT Drug-induced lactic acidosis: metformin - shock and overdose @ increase intestinal lactic acid production, impaired gluconeogensis, glycogenolysis, mitocondrial respiration and phophorylation=>mortality rate>30% @metformin is sliminated by kidney and highly water soluble Lactic acidosis 4. Treatment of lactic acidosis - CRRT -Drug induced lactic acidosis Hemodialysis and CRRT=> Correct acidosis and remove metformin from plasma -NRTI-induced lactic acidosis -Summary: CRRT are useful in uncontrollable acidemia with multiple organ failure, and removal causative toxin Anticoagulation - heparin: Heparin is the most commonly utilized anticoagulant @ risk of systemic bleeding and heparin-induced thrombocytopenia Anticoagulation Citrate: - - - chelating ionized calcium=> anticoagulation @decrease risk of systemic bleeding @systemic calcium infusion Citrate=>bicarbonate (carbonic anhydrase) @liver, skeletal muscle, kidney (high mitochondria) Citrate toxicity=> in liver failure patient @ metabolic acidosis=> because bicarbonate loss and citrate can’t metabolize bicarbonate @ ca2+ decrease but total plasma calcium increase Conclusion Hypercapnic acidosis and lactic acidosis - Bicarbonate infusion vs addition bicarbonate during CRRT - Need further prospective controlled study - Thanks for your attention ~~ Any question?