Hypothermia / Hyperthermia / Exposure
advertisement

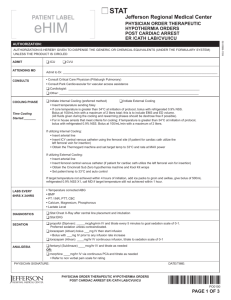
JP SMILES Core temp < 35 °C Research limited to either mild hypothermia in healthy subjects or case reports Heat loss occurs through ◦ ◦ ◦ ◦ Radiation Conduction Convection Evaporation Hypothermia results in derangement of multiple organ systems Shivering – increases metabolic rate but only while glycogen stores last and down to temps of 30 °C Initial tachycardia and peripheral vasoconstriction Subsequent bradycardia (refractory to atropine), hypotension and fall in cardiac output Osborn J waves appear < 32 °C Anti-arrythmic drugs and inotropes/vasopressors are generally ineffective at temperatures < 30 °C Loss of fine motors skills and co-ordination then loss of gross motor skills Progressive decrease in GCS Cerebrovascular auto regulation is lost at 24 °C 20 °C EEG is flat and patient appears dead as cerebral metabolism falls Temperatures at which shivering is lost varies widely 24 °C - 35 °C Temp < 28 °C = rigidity, mydriasis, and areflexia Initially rise in resp rate followed by depression and basal metabolic rate slows CO2 retention and resp acidosis can occur Significant fall in O2 consumption and CO2 production (50% at 30 °C) Apnoea can develop Initial left shift of the oxygen dissociation curve ◦ Impaired O2 delivery and tissue hypoxia ◦ Lactic acidosis If acidosis becomes severe the curve shifts back R again Cold induced diuresis GFR falls as CO and renal blood flow fall ARF in 40% of patients who require ICU Initial hypokalaemia due to shift of extracellular potassium into cells Hyperkalaemia can occur with acidosis secondary to cell death Intestinal motility decreases below 34 °C Ileus < 28 °C Oral medication is not appropriate Hepatic impairment can occur due to reduced CO (Raised lactate and therefore Hartmans is a bad idea) Pancreatitis and Mesenteric Venous Thrombosis are both common Increased blood viscosity fibrinogen and haematocrit Coagulopathy may develop Mild (35 °C - 32 °C) Moderate (32 °C - 28 °C) Severe (<28 °C) Temperature measurement Accurate low reading digital of mercury thermometer Placed 15 cm rectally of oesophageally (better as cold faeces can effect rectal temperatures) UEC Glucose CK FBC COAG LFT LIPASE VBG ◦ Hypo or hyperkalaemia/ARF/low HCO3◦ Hypo/Hyperglycaemia ◦ May be elevated ◦ Increased haematocrit due to cold induced diuresis and hypovolaemia ◦ Thrombocytopaenia ◦ Coagulopathy and DIC is common ◦ Transaminitis ◦ Pancreatitis ◦ Initial respiratory alkalosis ◦ Secondary respiratory and metabolic acidosis ECG ◦ ◦ ◦ ◦ ◦ Bradycardia PR/QRS/QT prolongation Variable ST and T wave changes Osborn J waves Arrythmias AF/VT/VF/1st, 2nd, 3rd Degree HB These waves were definitively described in 1953 by JJ Osborn Also called J waves Delayed depolarisation Represented as ST elevation at the QRS – ST junction < 32 °C Proportional to the degree of hypothermia Not pathognomonic ◦ SAH/Cerebral injuries/Myocardial ischaemia ABC Remove wet clothing and insulate Gentle handling – rough handling and invasive procedures have historically been thought to increase risk of cardiac arrythmias Now thought these risks have been overemphasised Consider co-existent pathology Intubation as necessary IV Access (drugs IV only. IM SC poor absorption) Urinary catheter NGT Temperature and cardiac monitoring Fluid resuscitation ◦ Dehydration is often present ◦ Warmed fluids ◦ Dextrose is good Avoid drugs until core temp 30 °C – ineffective and may accumulate until released Rewarming – mild hypothermia Endogenous rewarming ◦ Exercise if possible Passive external warming ◦ Warm dry environment ◦ Cover with warm blankets Rewarming – moderate hypothermia Active external rewarming Warm blankets Radiant heat source Bair hugger 2°C per hour Rewarming – severe hypothermia Includes cardiopulmonary arrest Warmed humidified inhaled oxygen Warmed IV fluids Warmed left pleural lavage Warmed Peritoneal lavage Cardiopulmonary bypass Most other methods are ineffective Arrythmias VF may occur spontaneously in < 29 °C Sinus brady and AF with slow ventricular response are common and can be considered physiological with hypothermia AF usually reverts spontaneously on rewarming Drugs and electricity are unlikely to work until temp is > 30 °C ETT – Warmed humidified air 42 °C - 46 °C Aggressive active core warming ◦ Warmed saline/peritoneal lavage/pleural lavage/bypass VF/VT – Single defibrillation appropriate and initial drug therapy. If no response defer further attempts or drug doses until core rises above 30 °C PEA/Asystole – Again wait till core temp above 30°C (atropine not likely to be effective) Many anecdotal reports of unexpected survival Not dead till they are warm and dead!!!! Heat stroke Heat exhaustion Heat cramps These may occur as a continuum Bhut Jolokia pepper Core body temp > 40 °C Hot dry skin CNS abnormalities (delirium/coma) Classical – Occurs due to exposure to a high environmental temperature Exertional – Occurs in the setting of strenuous exercise Oxidative phosphorylation stops at temperatures > 42 °C Cell damage Loss of thermoregulatory compensatory mechanisms Hypoxia, increased metabolic demands, circulatory failure, coagulopathies and inflammatory response Tachyarrythmias and hypotension Two types exist with exertional heat stroke ◦ Hyperdynamic group – high cardiac output and tachycardia ◦ Hypodynamic group – Low cardiac output, increase peripheral vascular resistance Cardinal features of heat stroke Delirium, lethargy, coma and seizures Can be permanent (up to 33%) Injured cells leak phosphate and calcium Hypercalcaemia and Hyperphosphataemia Hypokalaemia is seen early ◦ Secondary to heat induce hyperventilation leading to respiratory alkalosis ◦ Sweat and renal losses Hyperkalaemia is seen later ◦ Potassium losses from damaged cells and renal failure Hyperuricaemia develops secondary to the release of purines from injured muscle ARF in approx 30% ◦ Direct thermal injury to kidneys ◦ Pre-renal insult of volume depletion and renal hypoperfusion ◦ Rhabdomyolysis Exertional heat stroke is associated with haemorrhagic complications Petechial haemorrhages or eccyhmosis secondary to direct thermal injury or DIC Similar to sepsis The actions of inflammatory mediators account for the multi organ dysfunction Consider in patients with altered mental state and exposure to heat Classic triad of hyperthermia, neurological abnormalities and dry skin Measure temp with rectal/oesophageal probe Sweating can still be present Hypotension and shock 25% ◦ Hypovolaemia, peripheral vasodilatation and cardiac dysfunction Sinus tachy Hyperventilation – a universal finding in heat stroke UEC ◦ Hypokalaemia ◦ Hyperphosphataemia and hypercalcaemia ◦ Hyperkalaemia and hypocalcaemia may be present if rhabdomyolysis has occurred ◦ Renal impairment Urate – is frequently high and may play a role in the development of acute renal failure Glucose – elevated in up to 70% LFT Almost always seen in exertional heat stroke (AST and LDH most commonly elevated) CK – 10000 to 1000000 in rhabdomyolysis FBC – WCC as high as 30 -40,000 Coag – routinely abnormal and DIC may occur Acid Base: ◦ Lactic acidosis ◦ Compensatory respiratory alkalosis Myoglobin – serum or urine myoglobin may be elevated ECG ◦ Rhythm disturbances (sinus tachy, SVT + AF) ◦ Conduction defects (RBBB and intraventricular conduction defects) ◦ QT prolongation (most common secondary to low K+ , Ca 2+ and Mg 2+) ◦ ST changes (secondary to myocardial ischaemia) CXR: ◦ ARDS ◦ Aspiration If prompt effective treatment not undertaken mortality approaches 80% A – ETT if needed ◦ Consider early ◦ Avoid suxamaethonium B C ◦ Monitor Resp Rate and O2 sats ◦ Look for evidence of aspiration if GCS decreased ◦ Check for ARDS and ventilate as per lung injury protocol ◦ May be a large fluid deficit ◦ N saline is probably best (CSL – lactate and avoid K+ containing fluids) ◦ Monitor heart rate, BP, CVP and urine output ◦ Picco/Swan-Ganz pulmonary artery catheter may be indicated ◦ Pressors may be needed but avoid adrenergic agents as they can impair heat dissipation by causing peripheral vasoconstriction (dopamine) D – Intubate if needed E – Temperature should be measured by oesophageal or rectal probe Mainstay of therapy and must be initiated from the onset Use prehospital may be lifesaving Initially remove patient from heat source and remove all clothing Evaporative cooling – tepid water on the skin with fans Ice water immersion – most effective method but practically difficult and cant use monitors/equipment and uncomfortable for the patient Ice packs to axilla, groin and neck Cooling blankets and wet towels Peritoneal lavage and cardiopulmonary bypass can be considered in severe resistant cases Shivering may occur in rapid cooling – this will increase oxygen consumption and heat production ◦ Sedate ◦ paralyse Paracetamol and aspirin are ineffective and should not be used Mortality should be less than 10% with prompt treatment Most recover without sequalae Residual neurological defects are reported Heat exhaustion – mild heat stroke Same physiological process Patients can still have the capacity to dissipate heat and the CNS is not impaired Volume depletion is still a problem Painful involuntary spasms of major muscles Usually in heavily exercised muscle groups Dehydration and salt loss also thought to plat a role Rest rehydrate and replace salts