Integumentary System: Skin Structure & Function
advertisement

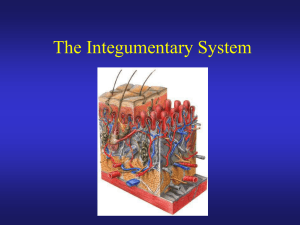
Week 6 Lecture 1 Chapter 5 The Integumentary System • Skin and its accessory structures – – – – – – structure function growth and repair development aging disorders General Anatomy • A large organ composed of all 4 tissue types • 22 square feet • 1-2 mm thick • Weight 10 lbs. • The skin protects us against environmental hazards. It’s the FIRST LINE OF DEFENSE • The skin helps regulate body temperature. • The skin is always being attacked by microorganisms • Skin makes up about 16% of the total body weight. • Tanning – ancient Rome women lightened their skin with lead based cosmetics. At the time of Shakespeare before industrial revolution un-tanned skin = high status • Europe 18/19th century fair skin with freckles was attractive while tan skin = manual labor like a farmer • 20th century- indoor work increased. Tan skin = leisure class. 1920 Coco Channel accidentally got tan on French Riviera. She ignited a fad. Introduction to the Integumentary System • Connections – Cardiovascular system • Blood vessels in the dermis – Nervous system • Sensory receptors for pain, touch, and temperature Skin Functions • Protection of underlying tissues and organs against impact, abrasion, fluid loss and chemical attacks. • Excretion of salts, water, wastes. 500 ml a day=1 pint • Temperature- via adipocytes which insulate to keep warmer, or evaporative ( sweating ) for cooling. • Synthesis of D3 ( cholcalciferol )Sunlight hits the skin, and the subcutaneous cholesterol stimulates D3 which will go to the liver where it will make some intermediary products which will go to the kidney which in turn will make Calcitriol. This will increase the absorption of calcium and phosphorous from the GI tract and increase the deposition to he bones. • Stores lipids in adipocytes • Detects touch, pressure, pain, temperature, and relays to the neural system. Overview • 2 Major layers of skin – epidermis is epithelial tissue only – dermis is layer of connective tissue, nerve & muscle • Subcutaneous tissue (subQ or hypodermis) is layer of adipose & areolar tissue – subQ = subcutaneous injection – intradermal = within the skin layer Overview of Epidermis • Stratified squamous epithelium • Mechanical protection • Keeps micro-organisms outside • Contains no blood vessels • 4 types of cells • 5 distinct strata (layers) of cells Cell types of the Epidermis • Keratinocytes--90% – produce keratin • Melanocytes-----8 % – produces melanin pigment – melanin transferred to other cells with long cell processes • Langerhan cells – from bone marrow – provide immunity • Merkel cells – in deepest layer – form touch receptor with sensory neuron Epidermis • Thin Skin – Covers most of the body – Has four layers of keratinocytes • Thick Skin – Covers the palms of the hands and soles of the feet – Has five layers of keratinocytes Layers (Strata) of the Epidermis • Strata means LAYER • Stratum corneum • Stratum lucidum • Stratum granulosum • Stratum spinosum • Stratum basale Epidermis • Stratum Germinativum-basale ( basal cell carcinoma ) – The “germinative layer” • Has many germinative (stem) cells or basal cells • Is attached to basal lamina by hemidesmosomes • Forms a strong bond between epidermis and dermis – Forms epidermal ridges (e.g., fingerprints) – Dermal papillae (tiny mounds) • Increase the area of basal lamina • Strengthen attachment between epidermis and dermis Epidermis Figure 5–4 The Epidermal Ridges of Thick Skin. Epidermis • Specialized Cells of Stratum Germinativum – Merkel cells • Found in hairless skin • Respond to touch (trigger nervous system) – Melanocytes • Contain the pigment melanin – or not with albinism • Scattered throughout stratum germinativum Epidermis • Stratum Spinosum – The “spiny layer” • Produced by division of stratum germinativum • Eight to ten layers of keratinocytes bound by desmosomes • Cells shrink until cytoskeletons stick out (spiny) – Continue to divide, increasing thickness of epithelium – Contain dendritic (Langerhans) cells, active in immune response Stratum Granulosum • 3 - 5 layers keratinocytes • Show nuclear degeneration • Contain dark-staining keratohyalin granules • Contain lamellar granules that release lipid that repels water • Highest level where living cells are found. Epidermis • Cells of Stratum Granulosum – Produce protein fibers – Dehydrate and die – Create tightly interlocked layer of keratin surrounded by keratohyalin Stratum Lucidum • Seen in thick skin on palms & soles of feet • Three to five layers of clear, flat, dead cells • Contains keratin Stratum Corneum • Exposed layer • 25 to 30 layers of flat dead cells filled with keratin and surrounded by lipids • Continuously shed – takes about 15-30 days for cells to go from the basal layer to corneum • Barrier to light, heat, water, chemicals & bacteria • Coats surface with lipid secretions form sebaceous glands • Friction stimulates callus formation • The skin is water resistant not water proof. So we lose about 500 ml or 1 pint of water a day. This is called insensible perspiration. • Ocean water is hypertonic. Water leaves the body which results in dehydration. In pool water (hypotonic) the water crosses the epithelium and can increase the size of cells 4 x the size. This is seen in the soles and palms. Keratinization & Epidermal Growth • Stem cells divide to produce keratinocytes • As keratinocytes are pushed up towards the surface, they fill with keratin • 4 week journey unless outer layers removed in abrasion. Dead cells can remain an additional 2 weeks before shedding. • Hormone EGF (epidermal growth factor) can speed up process • Psoriasis = chronic skin disorder – cells shed in 7 to 10 days as flaky silvery scales – abnormal keratin produced Skin Grafts • New skin can not regenerate if stratum basale and its stem cells are destroyed • Skin graft is covering of wound with piece of healthy skin – autograft from self – isograft from twin – autologous skin • transplantation of patients skin grown in culture Dermis • Connective tissue layer composed of collagen & elastic fibers, fibroblasts, macrophages & fat cells • Contains hair follicles, glands, nerves & blood vessels • Major regions of dermis – papillary region -superficial – reticular region –deeper – Tattoo ink is held here – Phagocytes digest the ink Papillary Region • • • • Top 20% of dermis- Superficial layer Composed of loose CT & elastic fibers Finger like projections called dermal papillae Functions – anchors epidermis to dermis – contains capillaries that feed epidermis – contains Meissner’s corpuscles (touch) & free nerve endings (pain and temperature) – It’s where dermatitis takes place. Reticular Region • Dense irregular connective tissue • Contains interlacing collagen and elastic fibers • Packed with oil glands, sweat gland ducts, fat & hair follicles • Provides strength, extensibility & elasticity to skin –stretch marks are dermal tears from extreme stretching Skin Color Pigments (1) • Melanin produced in epidermis by melanocytes – same number of melanocytes in everyone, but differing amounts of pigment produced – results vary from yellow to tan to black color – melanocytes convert tyrosine to melanin • UV in sunlight increases melanin production • Clinical observations – freckles or liver spots = melanocytes in a patch – albinism = inherited lack of tyrosinase; no pigment – vitiligo = autoimmune loss of melanocytes in areas of the skin produces white patches Skin Color Pigments (2) • Carotene in dermis – yellow-orange pigment (precursor of vitamin A) – Found in carrots and squash – Found in stratum corneum & dermis • Hemoglobin – red, oxygen-carrying pigment in blood cells – if other pigments are not present, epidermis is translucent so pinkness will be evident – When scared someone looks white as a ghost b/c blood went from skin > muscles – Skin gets flushed and red when body temp increases b/c superficial blood vessels dilate so skin acts as a radiator to lose heat. – Scarlet fever – Strep attacks RBC- the hemoglobin leaks into the interstitial cells. Skin Color as Diagnostic Clue • Jaundice – yellowish color to skin and whites of eyes – buildup of yellow bilirubin in blood from liver disease • Cyanotic – bluish color to nail beds and skin – hemoglobin depleted of oxygen looks purpleblue • Erythema – redness of skin due to enlargement of capillaries in dermis – during inflammation, infection, allergy or burns Skin Color Figure 5–5b Melanocytes. Skin Color • Function of Melanocytes – Melanin protects skin from sun damage – Ultraviolet (UV) radiation • Causes DNA mutations and burns that lead to cancer and wrinkles – Skin color depends on melanin production, not number of melanocytes Skin Color • Capillaries and Skin Color – Oxygenated red blood contributes to skin color • Blood vessels dilate from heat, skin reddens • Blood flow decreases, skin pales – Cyanosis • Bluish skin tint • Caused by severe reduction in blood flow or oxygenation Skin Color • Illness and Skin Color – Jaundice • Buildup of bile produced by liver • Yellow color – Addison disease • A disease of the pituitary gland • Skin darkening – Vitiligo • Loss of melanocytes • Loss of color Vitamin D3 • Vitamin D3 – Epidermal cells produce cholecalciferol (vitamin D3) • In the presence of UV radiation – Liver and kidneys convert vitamin D3 into calcitriol • To aid absorption of calcium and phosphorus – Insufficient vitamin D3 • Can cause rickets Vitamin D3 Figure 5–7 Rickets. Skin Color Figure 5–6 Skin Cancers. Hair • The human body is covered with hair, except – Palms – Soles – Lips – Portions of external genitalia • Functions of Hair – Protects and insulates – Guards openings against particles and insects – Is sensitive to very light touch Accessory Structures of Skin • Epidermal derivatives • Cells sink inward during development to form: – – – – hair oil glands sweat glands nails Structure of Hair • Shaft -- visible • Root -- below the surface • Follicle surrounds root – base of follicle is bulb • blood vessels • germinal cell layer Hair Related Structures • Arrector pili – smooth muscle in dermis contracts with cold or fear. – forms goosebumps as hair is pulled vertically • Hair root plexus – detect hair movement Hair A Single Hair Follicle Figure 5–10 Hair Follicles and Hairs. Functions of Hair • Prevents heat loss • Decreases sunburn • Eyelashes help protect eyes • Touch receptors (hair root plexus) senses light touch • Healthy loss is 50 a day. Glands of the Skin • Specialized exocrine glands found in dermis • Sebaceous (oil) glands • Sudiferous (sweat) glands • Ceruminous (wax) glands • Mammary (milk) glands Sebaceous (oil) glands- Holocrine gland • Secretory portion in the dermis • Most open onto hair shafts • Sebum – combination of cholesterol, proteins, fats & salts – keeps hair and skin soft & pliable – inhibits growth of bacteria & fungi(ringworm). The sebaceous glands forces lipids into the hair follicle and onto the skin creating a seal. • Acne- ( can be a sign of EPA deficiency ) – Bacterial inflammation of glands – secretions stimulated by hormones at puberty Sudoriferous (sweat) glands • Merocrine (sweat) glands – most areas of skin – secretory portion in dermis with duct to surface – regulate body temperature with perspiration • Apocrine old name. it’s now called Merocrine (sweat) glands – armpit and pubic region – secretory portion in dermis with duct that opens onto hair follicle – secretions more viscous – the sweat produced is a nutrient for bacteria which intensifies the odor. Ceruminous glands • Modified sweat glands produce waxy secretion in ear canal • Cerumin contains secretions of oil and wax glands • Helps form barrier for entrance of foreign bodies • Impacted cerumen may reduce hearing • Mammary Glands produce milk – found in both sexes, but rudimentary until puberty. With estrogen they develop, with testosterone they are inhibited. Nails • Nails protect fingers and toes – Made of dead cells packed with keratin – Metabolic disorders can change nail structure • Nail production – Occurs in a deep epidermal fold near the bone called the nail root Structure of Nails • Tightly packed keratinized cells • Nail body – visible portion pink due to underlying capillaries – free edge appears white • Nail root – buried under skin layers – lunula is white due to thickened stratum basale • Eponychium (cuticle) – stratum corneum layer – Nail matrix deep to the nail root is the region from which the nail growth occurs Nail Growth • Nail matrix below nail root produces growth • Cells transformed into tightly packed keratinized cells • 1 mm per week Clubbing of the Finger Nails: Symptom of Advanced Lung Cancer • It takes about 8 months for a nail to grow out. • White spots are called Leukonychia.- Caused by trauma, fungus, decreased zinc, decreased protein, alcoholism, allergy to nail products. • Brittle nails- Decreased Iron and Biotin, thyroid and/or kidney disease • Clubbed nails- hypoxia, lung cancer, heart or liver disease • Spooning- Iron deficiency anemia, systemic fungal infections, B12 deficiency • Beaus Lines – Transverse depression- Acute sever illness, diabetes, chemotherapy, decreased calcium • Splinter hemorrhages – Red/brown linear streaks, bacterial endocarditis, trichinosis( parasite-raw food ) • Paronchyia – inflammation of nail root, manicuring, biting, bacteria, yeast, fungi Excretion and Absorption • 500 mL of water evaporates from it daily • Small amounts salt, CO2, ammonia and urea are excreted • Lipid soluble substances can be absorbed through the skin – vitamins A, D, E and K, Oxygen and CO2 – acetone and dry-cleaning fluid, lead, mercury, arsenic, poisons in poison ivy and oak Transdermal Drug Administration • Method by which drugs in a patch enter the body • Drug absorption most rapid in areas where skin is thin (scrotum, face and scalp) • Examples – nitroglycerin (prevention of chest pain from coronary artery disease) – scopolamine ( motion sickness) – estradiol (estrogen replacement therapy) – nicotine (stop smoking alternative) • In 2002 23,800 pre-mature deaths in U.S form cancer due to decreased UVB exposure which decreases the VIT D. • Other research says 50-63,000 die a year from decreased Vit. D. this is higher than 8800 deaths from Melanoma or squamous cell carcinoma. • 1 in 5 kids ( 80 % hispanics 90 % afroamericans) Burns • 1st Degree – Sunburn – Skin redness erythema = inflammation of the epidermis. • 2nd Degree – Entire Epidermis and some dermisBlister, pain, swelling. The accessory structures usually not effected. • 3rd Degree – Destroys BOTH epidermis and dermis. Swelling but less pain b/c sensory nerves are destroyed with blood vessels. • If burns cover more than 20 % of the body then it’s life threatening b/c Increased :fluid loss, evaporating cooling, bacteria on moist skin. This will lead to wide spread infection called SEPSIS. This is leading cause of death in burn victims. • If burns are on 80 % of the body 50/50 % of living. • Rules of 9 for body parts and % of burn Arms 9/9 = 18% Legs 18/18 = 36% Trunk 18/18 = 36% Head 9 = 9% Genitals = 1% ______________________ 100 % UVA UVB Rays • UVAPenetrate the dermis Produces oxygen free radicals that disrupt collagen and elastic fibers. This is reason for severe wrinkling. Permeate blood vessels and destroys Folic Acid. UVB These rays reach the keratinocytes and convert cholesterol into pre-vit D, which the kidney will later make into vit D. The melanin produced protects against DNA damage and folate breakdown. Repair of the Integument • Bleeding occurs • Mast cells trigger inflammatory response • A scab stabilizes and protects the area • Germinative cells migrate around the wound • Macrophages clean the area • Fibroblasts and endothelial cells move in, producing granulation tissue Repair of the Integument Figure 5–14 Repair of Injury to the Integument. Repair of the Integument Figure 5–14 Repair of Injury to the Integument. Repair of the Integument • Fibroblasts produce scar tissue – Inflammation decreases, clot disintegrates – Fibroblasts strengthen scar tissue – A raised keloid may form Repair of the Integument Figure 5–15 A Keloid. Importance of the Integumentary System Figure 5–16 The Integumentary System in Perspective. Importance of the Integumentary System Figure 5–16 The Integumentary System in Perspective. Importance of the Integumentary System Figure 5–16 The Integumentary System in Perspective. Importance of the Integumentary System Figure 5–16 The Integumentary System in Perspective.