Blood Vessels - drtracey.net
advertisement

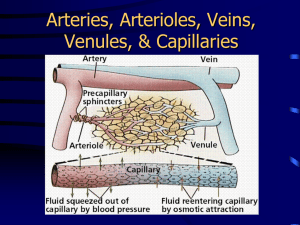
The Circulatory System Blood Vessels Anatomy & Physiology II Chapter 15 The Vascular System Closed system Blood vessels Four heart chambers Blood Vessels Delivery system of dynamic structures that begins and ends at the heart ◦ Arteries: carry blood away from the heart; oxygenated except for pulmonary circulation and umbilical vessels of a fetus ◦ Capillaries: contact tissue cells and directly serve cellular needs ◦ Veins: carry blood toward the heart Blood Vessels Five types of blood vessels Arteries Arterioles Capillaries Venules Veins Blood Circuits Two groups of blood vessels The pulmonary circuit ◦ Pulmonary artery and its branches ◦ Capillaries in lungs ◦ Pulmonary veins The systemic circuit ◦ Aorta ◦ Systemic capillaries ◦ Systemic veins Blood flow in a closed system of vessels Oxygen content changes as blood flows through the capillaries. Zooming In • Judging from color coding, which vessels pick up oxygen? Which vessels release oxygen? Vessel Structure Three tunics (coats) of arteries and veins Inner (endothelium) Middle (smooth [voluntary] muscle) ◦ Controlled by autonomic nervous system ◦ Thinner in veins Outer (supporting connective tissue) Sections of small blood vessels Drawings show the thick wall of an artery, the thin wall of a vein, and the single-layered wall of a capillary. A venous valve also is shown.The arrow indicates the direction of blood flow. Zooming In: Which vessels have valves that control blood flow? Systemic Arteries The aorta Largest artery Receives blood from left ventricle Branches to all organs The Aorta and Its Parts Ascending aorta Aortic arch Thoracic aorta Abdominal aorta The aorta and its branches Zooming In: How many brachiocephalic arteries are there? Principal systemic arteries Zooming In: How many brachiocephalic arteries are there? Branches of the Ascending Aorta and Aortic Arch Ascending aorta ◦ Left and right coronary arteries Aortic arch ◦ Brachiocephalic artery Right subclavian artery Right common carotid artery ◦ Left common carotid artery ◦ Left subclavian artery Branches of the Thoracic Aorta Branches to chest wall, esophagus, and bronchi Intercostal arteries Branches of the Abdominal Aorta Celiac trunk ◦ Left gastric artery ◦ Splenic artery ◦ Hepatic artery Superior mesenteric artery Inferior mesenteric artery Paired lateral branches ◦ ◦ ◦ ◦ ◦ Phrenic arteries Suprarenal arteries Renal arteries Ovarian and testicular arteries Lumbar arteries The Iliac Arteries and Their Subdivisions Internal iliac arteries External iliac arteries ◦ Femoral artery Popliteal artery Tibial arteries Dorsalis pedis Arteries That Branch to the Arm and Head External carotid artery Internal carotid artery Subclavian artery ◦ Vertebral artery ◦ Axillary artery Brachial artery Radial artery Ulnar artery Anastomoses Communication between two vessels Circle of Willis Superficial palmar arch Mesenteric arches Arterial arches Arteries that supply the brain The bracket at right groups the arteries that make up the circle of Willis. Arterioles Smallest arteries Lead to capillary beds Control flow into capillary beds via vasodilation and vasoconstriction Systemic Veins Superficial veins ◦ Cephalic, basilic, median cubital veins ◦ Saphenous veins Deep veins ◦ Femoral and iliac vessels ◦ Brachial, axillary, subclavian vessels ◦ Jugular veins ◦ Brachiocephalic vein The Venae Cavae and Their Tributaries Superior vena cava ◦ Head, neck, upper extremities Azygos vein ◦ Chest wall Inferior vena cava ◦ Right, left veins from paired parts, organs ◦ Unpaired veins from spleen, digestive tract Principal systemic veins Zooming In: How many brachiocephalic veins are there? Venous Sinuses Coronary sinus Cranial venous sinuses ◦ Cavernous sinuses Petrosal sinuses ◦ Superior sagittal sinus Confluence of sinuses ◦ Transverse sinuses (lateral sinuses) Cranial venous sinuses The inset shows the paired transverse sinuses, which carry blood from the brain to the jugular veins. The Hepatic Portal System Carries blood from abdominal organs to liver Superior mesenteric vein Splenic vein Gastric, pancreatic, inferior mesenteric veins Sinusoids Hepatic portal system Veins from the abdominal organs carry blood to the hepatic portal vein leading to the liver. Arrows show the direction of blood flow. Zooming In: What vessel do the hepatic veins drain into? Circulation Physiology Blood exchanges oxygen, carbon dioxide, other substances generated by cells Tissue fluid (interstitial fluid) is exchange medium Connection between small blood vessels through capillaries The blood delivers oxygen (O2) to the tissues and picks up carbon dioxide (CO2) for transport to the lungs. Note the lymphatic capillaries, which aid in tissue drainage. Capillaries Microscopic blood vessels Walls of thin tunica intima, one cell thick Pericytes help stabilize their walls and control permeability Size allows only a single RBC to pass at a time Capillaries In all tissues except for cartilage, epithelia, cornea and lens of eye Functions: exchange of gases, nutrients, wastes, hormones, etc. Capillaries Three structural types 1. Continuous capillaries 2. Fenestrated capillaries 3. Sinusoidal capillaries (sinusoids) Continuous Capillaries Abundant in the skin and muscles ◦ Tight junctions connect endothelial cells ◦ Intercellular clefts allow the passage of fluids and small solutes Continuous capillaries of the brain ◦ Tight junctions are complete, forming the blood-brain barrier Pericyte Red blood cell in lumen Intercellular cleft Endothelial cell Basement membrane Tight junction Endothelial nucleus Pinocytotic vesicles Continuous capillary: Least permeable, and most common (e.g., skin, muscle). Fenestrated Capillaries Some endothelial cells contain pores (fenestrations) More permeable than continuous capillaries Function in absorption or filtrate formation (small intestines, endocrine glands, and kidneys) Pinocytotic vesicles Red blood cell in lumen Fenestrations (pores) Endothelial nucleus Basement membrane Tight junction Intercellular cleft Endothelial cell Fenestrated capillary: Large fenestrations (pores) increase permeability. Occurs in special locations (e.g., kidney, small intestine). Sinusoidal Capillaries Fewer tight junctions, larger intercellular clefts, large lumens Usually fenestrated Allow large molecules and blood cells to pass between the blood and surrounding tissues Found in the liver, bone marrow, spleen Endothelial cell Red blood cell in lumen Large intercellular cleft Tight junction Incomplete basement membrane Nucleus of endothelial cell Sinusoidal capillary: Most permeable. Occurs in special locations (e.g., liver, bone marrow, spleen). Blood Flow Through Capillary Beds Precapillary sphincters regulate blood flow into true capillaries Regulated by local chemical conditions and vasomotor nerves Vascular shunt Precapillary sphincters Terminal arteriole Metarteriole Thoroughfare channel True capillaries Postcapillary venule (a) Sphincters open—blood flows through true capillaries. Terminal arteriole Postcapillary venule (b) Sphincters closed—blood flows through metarteriole thoroughfare channel and bypasses true capillaries. Capillary Exchange How substances move between cells and capillary blood Diffusion ◦ Main process Blood pressure ◦ Moves material into tissue fluid Osmotic pressure ◦ Moves material into capillaries Factors Aiding Venous Return 1. Respiratory “pump”: pressure changes created during breathing move blood toward the heart by squeezing abdominal veins as thoracic veins expand 2. Muscular “pump”: contraction of skeletal muscles “milk” blood toward the heart and valves prevent backflow 3. Vasoconstriction of veins under sympathetic control The Dynamics of Blood Flow Vasomotor center in medulla regulates vasomotor activities Vasodilation Vasoconstriction Precapillary sphincter Return of Blood to the Heart Mechanisms that promote blood’s return to heart Contraction of skeletal muscles Valves Breathing Role of skeletal muscles and valves in blood return. Role of skeletal muscles and valves in blood return. (A) Contracting skeletal muscle compresses the vein and drives blood forward, opening the proximal valve, while the distal valve closes to prevent backflow of blood. (B) When the muscle relaxes again, the distal valve opens, and the proximal valve closes until blood moving in the vein forces it open again. The Pulse Ventricular contraction Wave of increased pressure Begins at heart and travels to arteries Influenced by various factors ◦ ◦ ◦ ◦ ◦ ◦ ◦ Body size Gender Age Muscular activity Emotion Body temperature Thyroid secretion Blood Pressure Force exerted by blood against vessel walls Determined by heart’s output and resistance to blood flow Systemic Blood Pressure The pumping action of the heart generates blood flow Pressure results when flow is opposed by resistance Systemic pressure ◦ Is highest in the aorta ◦ Declines throughout the pathway ◦ Is 0 mm Hg in the right atrium The steepest drop occurs in arterioles Arterial Blood Pressure Systolic pressure: pressure exerted during ventricular contraction Diastolic pressure: lowest level of arterial pressure Pulse pressure = difference between systolic and diastolic pressure Systemic Blood Pressure Systolic pressure Mean pressure Diastolic pressure Arterial Blood Pressure Reflects two factors of the arteries close to the heart ◦ Elasticity (compliance or distensibility) ◦ Volume of blood forced into them at any time Blood pressure near the heart is pulsatile Capillary Blood Pressure Ranges from 15 to 35 mm Hg Low capillary pressure is desirable ◦ High BP would rupture fragile, thin-walled capillaries ◦ Most are very permeable, so low pressure forces filtrate into interstitial spaces Maintaining Blood Pressure Requires ◦ Cooperation of the heart, blood vessels, and kidneys ◦ Supervision by the brain Maintaining Blood Pressure The main factors influencing blood pressure: ◦ Cardiac output (CO) ◦ Peripheral resistance (PR) ◦ Blood volume Maintaining Blood Pressure F = P/PR and CO = P/PR Blood pressure = CO x PR (and CO depends on blood volume) Blood pressure varies directly with CO, PR, and blood volume Changes in one variable are quickly compensated for by changes in the other variables Cardiac Output (CO) Determined by venous return and neural and hormonal controls Resting heart rate is maintained by the cardioinhibitory center via the parasympathetic vagus nerves Stroke volume is controlled by venous return (EDV) Cardiac Output (CO) During stress, the cardioacceleratory center increases heart rate and stroke volume via sympathetic stimulation ◦ ESV decreases and MAP increases Exercise BP activates cardiac centers in medulla Activity of respiratory pump (ventral body cavity pressure) Activity of muscular pump (skeletal muscles) Parasympathetic activity Sympathetic activity Epinephrine in blood Sympathetic venoconstriction Venous return Contractility of cardiac muscle EDV ESV Stroke volume (SV) Heart rate (HR) Initial stimulus Physiological response Result Cardiac output (CO = SV x HR Figure 19.8 Control of Blood Pressure Short-term neural and hormonal controls ◦ Counteract fluctuations in blood pressure by altering peripheral resistance Long-term renal regulation ◦ Counteracts fluctuations in blood pressure by altering blood volume Cardiac Output Volume of blood pumped out of each ventricle in one minute Heart rate ◦ Beats per minute Stroke volume ◦ Controlled by force of contractions Resistance to Blood Flow Peripheral resistance is affected by Vasomotor changes Baroreceptors in large arteries Elasticity of blood vessels Viscosity Total blood volume Blood Pressure Measurement Pressure is measured in the brachial arm artery using a sphygmomanometer Systolic pressure ◦ Occurs during heart contraction ◦ Normal systolic: 120 mmHg Diastolic pressure ◦ Occurs during heart relaxation ◦ Normal diastolic: 80 mmHg Abnormal Blood Pressure Hypotension ◦ Lower than normal blood pressure Hypertension ◦ High blood pressure Essential hypertension ◦ No apparent medical cause Treatment of Hypertension Stage 1 ◦ 140/90 mm Hg ◦ Diet, exercise, weight loss Stage 2 ◦ 160/100 mm Hg ◦ Drugs added to treatment Arterial Degeneration and Other Blood Vessel Disorders Arteriosclerosis ◦ Atherosclerosis Clot formation Leg cramps, pain, lameness Cerebral artery sclerosis Hypertension Coronary artery arteriosclerosis Renal artery damage Ischemia, gangrene Treatment for Arterial Degeneration Balloon catheterization Bypass grafts Stents Endarterectomy Aneurysm Bulging sac in blood vessel wall Swelling deranges other structures Can burst, causing death Surgery can replace damaged segment Hemorrhage Profuse escape of blood from vessels Internal or external Can be life-threatening ◦ Apply pressure to wound ◦ Elevate extremity above heart ◦ Apply pressure to pressure point Shock Inadequate blood flow to tissues Classified by type ◦ Cardiogenic ◦ Septic ◦ Hypovolemic ◦ Anaphylactic Classified by severity (cause unknown) ◦ Mild ◦ Severe Thrombosis Formation of blood clot in a vessel Deep venous thrombosis (DVT) Embolus Pulmonary embolism Phlebitis Thrombophlebitis Varicose Veins Superficial veins that are swollen, distorted, and ineffective Saphenous veins of lower extremities Rectal veins (hemorrhoids) End of Presentation