ATHEROSCLEROSIS
BY
Dr Ola Omran
Pathology Department
objectives
1. Define & classify Arteriosclerosis
2. Emphasize the clinical importance of the arteriosclerosis
3. List the risk factors & explain the pathogenesis of Atherosclerosis
4. Describe the Morphology of complicated & uncomplicated atheromatous lesions
5. Explain the pathological consequences, prognosis & common complications of
Atherosclerosis
Arteriosclerosis ( literally, hardening of arteries )
• Classification of Arteriosclerosis
1. Atherosclerosis
2. Monckeberg medial calcific sclerosis
3. Arteriolosclerosis
Arteriosclerosis
Arteriosclerosis
Hardening
Atherosclerosis
Large BV
Intima
Medial Calcific
Sclerosis
Media
Arteriolosclerosis
Small vessel
Full thickness
Hyaline Hyperplastic
This is Monckeberg's medial calcific sclerosis , which is the most insignificant form of arteriosclerosis.
Note the purplish blue calcifications in the media; note that the lumen is unaffected by this process.
Thus, there are usually no real clinical consequences.
Atherosclerosis
DEFINITION
“ Chronic inflammatory disorder of intima of large arteries characterised by formation of fibrofatty plaques called atheroma, which protrudes into and obstructs the vascular lumen & weakens the underlying media & may be associated with serious complications ”.
ATHEROMA
Risk Factors for Atherosclerosis
Non modifiable
• Age
• Male Sex,
• Genetic - Hyperchol.
• Family history
Potentially Modifiable
• Hyperlipidemia –
HDL/LDL ratio.
• Hypertension.
• Smoking.
• Diabetes.
• Lesser, or Non quantitated risk factors
– Obesity
– Physical inactivity
– Stress
– Postmenopausal estrogen deficiency
– High carbohydrate intake
– Alcohol
– Lipoprotein a
– Hardened unsaturated fat intake
– Chlamydia pneumoniae
PATHOGENESIS
Response to injury hypothesis
,
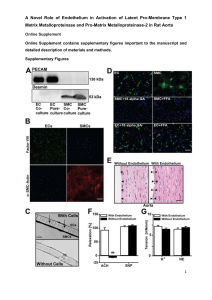
Atherosclerosis is considered to be a chronic inflammatory response of the arterial wall initiated by the injury to the endothelium .
Main features of the injury hypothesis :
1.
Chronic endothelial injury
2.
Insudation of lipoproteins into the vessel wall mainly LDL with high cholestrol content…….then o xidation of lesional lipoprotein
3.
Adhesion of blood monocytes & other leukocytes to the endothelium ,
& their migration into the intima & their transformation into macrophages & foam cells
4.
Adhesion of platelets
5.
Release of factors from activated platelets , macrophages or vascular endothelial cells that cause migration of SMCs from media into the intima.
6.
Proliferation of SMCs in the intima , elaboration of extracellular matrix , leading to accumulation of collagen & proteoglycans .
7.
Enhanced accumulation of lipids within macrophages & SMCs & extracellularly
Evolution of arterial wall changes in response to injury hypothesis
Pathogenesis in short:
1. intimal injury
2. Inflammation, Necrosis
3. Lipid – Cholesterol accumulation (soft.atheroma)
4. Fibrosis, smooth muscle proliferation
(hard.atheroma)
5. Extension of lesion and destruction of vessel
6. Complications - Thrombosis, embolism, aneurism, dissection & rupture.
Morphology of atheroma
(GP)
Athermo plaque consists of:
• a raised focal lesion , soft , yellow core of lipids( mainly cholestrol & cholestrol esters), covered by a firm, white fibrous cap .
• 0.3-1.5 cms . In diameter, sometimes coalesce to form larger lesions.
• Involve partial circumference of arterial wall (
( eccentric ), patchy & variable along the length of vessel.
• First the patches are focal & sparse then gradually increase in size & become diffuse
GP
1. Fatty dots
• not raised , so do not cause obstruction to the flow
• Multiple, yellow , flat spots < than 1mm in diameter
• composed of lipid laden foam cells
2. Fatty streaks = coalesce of multiple fatty dots
• Elongated, 1 cms longer or more
• contain T- lymphocytes & extracellular lipid < than plaques
• Appear in aorta in some children younger than 1 year & all children older than 10years ,
3.
Fatty streaks may be precursor of plaque but not all fatty streaks are converted into fibrous plaque or more advanced lesions
The white arrow denotes the most prominent fatty streak in the photo, but there are other fatty streaks scattered over the aortic surface. Fatty streaks are the earliest lesions seen with atherosclerosis in arteries.
Common sites:
1. Abdominal aorta compared to thorasic aorta & lesions are more common around the ostia of major branches
2. Other common arteries in descending order after aorta is coronaries, popliteal, internal carotid
& cicle of Willis
3. Vessels of the upper extremities are usually spared
4. Mesenteric & renal arteries are also spared but ostias can be involve
COMPONENTS OF ATHEROMATOUS PLAQUE (MP)
1.
*Superficial fibrous cap is composed of SMCs & relatively dense collagen
2.
*cellular zone containing, SMCs , macrophages,
Lymphocytes (T cells)
*Foam cells : are monocytes derived from blood & SMCs can also become foam cells
3.
* Deep to the fibrous cap is central necrotic core , containing a disorganized mass of lipids( cholestrol& cholestrol esters) cholestrol clefts, debris from dead cells , foam cells, fibrin
4.
*Below & to the sides of cap ( shoulder) is a cellular area cosisting of macrophages, SMCs, T lymphocytes
5.
At the periphery area of neovascularization is present
Generally plaque undergo remodelling ( degeneration , synthesis of ECM & organization of thrombus.
Atheroma Aorta:
Atheroma Aorta:
Atheroma Coronary Artery:
Calcification
COMPLICATIONS & clinical significance
A) Advanced lesions of atheromas are vulnerable to following pathological changes:
1. Thrombosis & calcification
2. Emboli formation , cholestrol emboli or atheroemboli which are discharged into blood stream.
3. Rupture, ulceration, erosions.
4. Hemorrhage: due to rupture of fibrin cap or thin walled capillaries that vascularize the plaque & contained hematoma expand & rupture the plaque
5. Aneurysmal dilatation: Fusiform, dissecting, or berry etc., due to pressure or ischemic atrophy of media with loss of elastic tissue causing weakness & rupture .
This is severe atherosclerosis of the aorta in which the atheromatous plaques have undergone ulceration along with formation of overlying mural thrombus.
A coronary thrombosis is seen microscopically occluding the remaining small lumen of this coronary artery.
Such an acute coronary thrombosis is often the antecedent to acute myocardial infarction.
The aorta shows a large atheroma . Cholesterol clefts are numerous in this atheroma. The surface shows ulceration and hemorrhage .
COMPLICATIONS & clinical significance
B) ATH mostly involves arteries supplying the heart , brain. Kidneys & lower extremities
1. Myocardial infarction ( heart attack)
2. Cerebral infarction ( stroke)
3. Chronic IHD
4. ischemic encephalopathy
5. Aortic aneurysms
6. Peripheral vascular disease ( gangrene of the legs)
7. mesenteric occlusion
8. Sudden cardiac death
Coronary
Thrombosis
With Infarction
Thrombo-embolism
Aorta Dissecting Aneurisms:
Subarachnoid
Haemorrhage:
American heart association classified
ATH into six types or stages
• Type I – Fatty dots - Foam cells
• Type II – Fatty streak
• Type III – Intermediate stage (Extracellular lipid pool)
• Type IV – Atheroma – Core of lipid
• Type V – Fibroatheroma – Fibrotic layer
• Type VI – Complicated lesion ( Ulcer, Ca+
Hemorrhage, thrombus, embolism, aneurysm).
Prevention
• Three factors need improvement
1. life style, cigarette smoking
2.Reduced consumption of cholestrol & saturated animal fat & control of hypertension
3. Prevention of recurrences in those who have previously suffered from serious
ATH related clinical events
Summary:
• Disease of elastic & medium sized muscular arteries.
• Fatty dots, streaks, plaques & complications.
• Risk factors – Males, age, Hypertension, smoking, DM, life style.
• High LDL & low HDL.
• Major cause of ischemic organ damage & death. Stroke, MI, Aneurysms, Gangrene