Atherosclerosis
advertisement

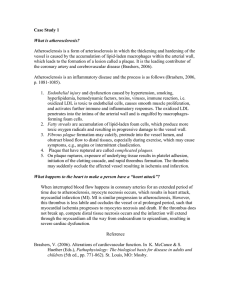
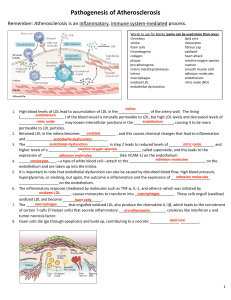
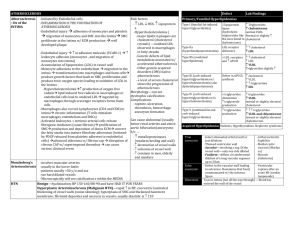
Atherosclerosis Mike Clark, M.D. Terms • • • • Arteriosclerosis – hardening of the arteries Atherosclerosis – a form of arteriosclerosis Venosclerosis Arteriolosclerosis Step One of Atherosclerosis Endothelium injured The tunica interna is injured in some way by bloodborne chemicals, hypertension, components of cigarette smoke or viral or bacterial infections. Almost any type of chronic infection – including periodontal disease can cause the damage. Step Two of Atherosclerosis Lipids accumulate and oxidize in the tunica intima Injured endothelial cells release chemotactic agents and growth factors (VEGF) and begin to modify lipids picked up from blood, in particular LDL, that delivers cholesterol to tissues. The accumulated LDL is oxidized as a result of the endothelial inflammation. This damages neighboring endothelial and tunica interna cells – and acts as a chemotactic agent, attracting macrophages. Some of these macrophages become so engorged with LDL that they are transformed into lipid-laden cells termed “foam cells.” The accumulation of these foam cells in the local area forms a fatty streak – the first sign of the of atheroma development. Step Three of Atherosclerosis Smooth muscle cells migrate and proliferate and a fibrous cap forms Smooth muscle cells migrate from the tunica media and deposit collagen and elastic fibers in the tunica intima – thus producing fibrous lesions with a cord of dead and dying foam cells – termed a fibrous or atherosclerotic plague. At first the growing plaque causes expansion of the vessel wall – but eventually the plague causes narrowing of the vessel lumen. Step Four of Atherosclerosis The Plague becomes unstable As the plaque continues to enlarge, the cells at its center die. Calcium is deposited, and collagen fiber production by smooth muscle cells declines. Now called a complicated plaque – it constricts the vessel wall and caused the arterial walls to fray and ulcerate, conditions that encourage blood sludging and backup, platelet adhesion, and thrombus formation. The vessels increased rigidity leads to hypertension. Together these events increase the risk of myocardial infarction, strokes, and aneurysms, that are responsible for pain (angina) that occurs when heart muscle becomes ischemic. Damaged Endothelial Cells • 1. Produce less Nitric Oxide – a local vasodilator and inhibitor of platelet aggregation • 2. Produce less Prostacyclin (PGI2) – an inhibitor of platelet aggregation • 3. Produce less thrombomodulin – inhibits coagulation • 4. Produces less heparin-like molecules • 5. Produce more von Willebrand factor and tissue thromboplastin – which promote coagulation. Figure UN 19.1