Therapeutic Drug Monitoring of Cyclosporine
advertisement

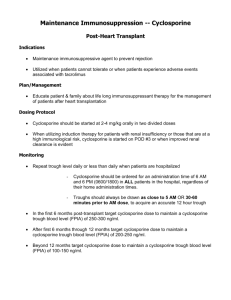
Therapeutic Drug Monitoring of Cyclosporine Therapeutic Drug Monitoring Quantification of drug concentration in a biological fluid to assess therapeutic compliance, efficacy, and/or to prevent drug-induced toxicity. Cyclosporine 11-amino acid cyclic peptide, discovered in soil fungus in 1970. It has tremendously improved graft survival in all areas of transplantation, through inhibition of T lymphocytes activity. Tolypocladium inflatum Why cyclosporine needs to be monitored? 1. Narrow therapeutic index. Desirable pharmacological effect only within narrow ranges of concentration in the blood. Too much nephrotoxicity; Too little graft rejection. 2. Poor dose response relationship. Soluble only in organic solvents or lipids, it is insoluble in water. Highly variable absorption between and within patients. 3. The clinical effect is difficult to measure. Graft rejection may be the first indication of therapeutic ineffectiveness. The major adverse effect of the drug is hard to distinguish from a lack of therapeutic effects. Measuring cyclosporine blood concentration Whole blood Cyclosporine is 90% protein bound and concentrated in erythrocytes. The degree of concentration in erythrocytes is temperature dependent in vitro. Immunoassay cross-reactivity to the metabolites HPLC HPLC-MS/MS When cyclosporine should be monitored? 1. Trough, C0 monitoring Trough level is the lowest level that a medicine is present in the body. In a medicine that is administered periodically, the trough level should be measured just before the administration. Titrate the dose of cyclosporine to get the predose blood concentration of the drug into a range that is considered both nontoxic and effective. 2. Average concentration (CAV) and area under the concentration-time curve (AUCt) monitoring Mutiple blood samples are taken over a dosing interval and the conentrationtime curve is drawn. CAV= AUCt/T AUC0-4: Area under the concentration-time curve in the first 4 hours. 3. C2 monitoring The concentration 2 hours after dosing Trough, C0 monitoring Benefits: simple, practical Challenges: inaccurate indicator of total drug exposure not a sensitive predictor of clinical outcomes The method of choice for most transplant units until recently. Overlap in the predose concentrations seen in patients with rejection and those exhibiting nephrotoxicity Relationship between C0 level and either rejection or nephrotoxicity could not be always established in different studies. AUC monitoring AUC monitoring Benefits: Challenges: more precise indicator of total drug exposure more sensitive predictor of clinical outcomes able to characterize abnormal absorption patterns impractical, extra blood sampling required higher cost AUC was better correlated with dose and was a better predictor of acute and chronic rejection, graft survival rate, nephrotoxicity, and efficacy of treatment in psoriatic patients. AUC monitoring Sparse sample algorithms Keown et al.Transplant Proc 1998;30:1645–9. AUC monitoring Sparse sample algorithms AUC = Constant + M1 × Ct1 + M2 × Ct2 + M3 × Ct3 . . .+ Mi × Cti AUC monitoring Sparse sample algorithms AUC monitoring Sparse sample algorithms AUC monitoring Sparse sample algorithms Ther Drug Monit 2001; 23(2):100-114. AUC monitoring Sparse sample algorithms Benefits: more practical, 2-3 point-sampling is adequate accurate estimators of Neoral® AUC value Challenges: be careful when choose which algorithm to follow. AUC(0-4) monitoring The study population comprised 98 consecutive primary kidney transplant recipients transplanted between August 1998 and December 1999 at the Queen Elizabeth II Health Sciences Centre in Halifax. All patients were followed for a minimum of 6months. The diagnosis of AR was confirmed by percutaneous core needle biopsy, and classified according to the Banff criteria. American Journal of Transplantation 2002; 2: 789–795. C2 monitoring Benefits: more practical accurate estimators of Neoral® AUC value Challenges: under validation in various graft transplantation C2 monitoring Transplantation 2001; 72(6):1024-1032. C2 monitoring American Journal of Transplantation 2002;2:148-156. Patients receiving transplants between February 2002 and September 2003 (n89) were prospectively managed by daily C2 monitoring of CsA-MEF. CsA-MEF was administered orally, mostly in capsule formulation, at 5 AM and 5 PM under the supervision of a nurse. Blood was collected daily by a study nurse at 2 hours after the morning dose, and C2 concentrations of CsA were determined by fluorescence-polarization immunoassay (FPIA). Target C2 levels were1,500±200 ng/mL. Patients managed by C2 monitoring (C2 group) were retrospectively compared with the kidneytransplant recipients receiving transplants throughout 2001 (n88) who fulfilled the same criteria for inclusion in the study but who had been managed by trough level monitoring of CsA-MEF (C0group). In the C0 group, target levels for CsA were 250 ± 50 ng/mL (FPIA). The study was conducted in 21 centers in eight countries using a prospective, multicenter, randomized, parallel cohort open-label design which was approved by the ethics committee at each participating center. All patients received immunoprophylaxis with basiliximab 20mg i.v. on the day of transplant and 20mg i.v. on day 4, and maintenance double-drug immunosuppression consisting of cyclosporine emulsion and prednisone. Treatment with cyclosporine emulsion was commenced at a dose of 4±6mg/kg given orally twice daily, starting within the first 12h following transplantation. CsA levels were measured at each site by a monoclonal antibody assay specific for the parent molecule, and the daily dose was adjusted to maintain the selected target ranges within each Daily Dose American Journal of Transplantation 2002;2:157-166. American Journal of Transplantation 2002;2:157-166. Thirty-one patients (27 men and 4 women, 52±10 years, 74% Caucasian) who underwent routine surveillance endomyocardial biopsy following OHT at the Hospital of the University of Pennsylvania were enrolled. Ther Drug Monit 2005; 27(4):417-421. Ther Drug Monit 2005; 27(4):417-421. N should be 83(C0) and 21(C2) in each group to get a power of 80% to detect if P<0.05 Ther Drug Monit 2005; 27(4):417-421. Opposite to expected Ther Drug Monit 2005; 27(4):417-421.