eprint_3_14241_1419
advertisement
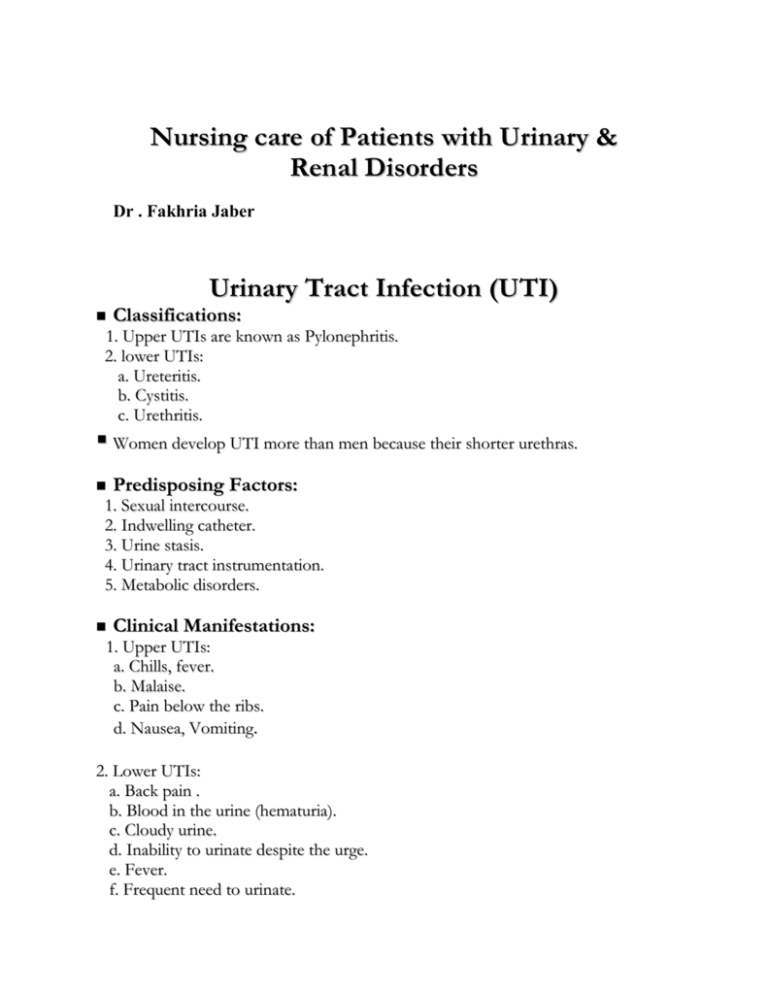
Nursing care of Patients with Urinary & Renal Disorders Dr . Fakhria Jaber Urinary Tract Infection (UTI) Classifications: 1. Upper UTIs are known as Pylonephritis. 2. lower UTIs: a. Ureteritis. b. Cystitis. c. Urethritis. Women develop UTI more than men because their shorter urethras. Predisposing Factors: 1. Sexual intercourse. 2. Indwelling catheter. 3. Urine stasis. 4. Urinary tract instrumentation. 5. Metabolic disorders. Clinical Manifestations: 1. Upper UTIs: a. Chills, fever. b. Malaise. c. Pain below the ribs. d. Nausea, Vomiting. 2. Lower UTIs: a. Back pain . b. Blood in the urine (hematuria). c. Cloudy urine. d. Inability to urinate despite the urge. e. Fever. f. Frequent need to urinate. g. General discomfort (malaise). h. Painful urination (dysuria). Diagnostic tests: 1. Urine analysis. 2. Urine culture. 3. WBCs. Prevention: 1. Avoid products that may irritate the urethra (e.g., bubble bath, scented feminine products). 2. Cleanse the genital area before sexual intercourse. 3. Change soiled diapers in infants and toddlers promptly. 4. Drink plenty of water to remove bacteria from the urinary tract. 5. Do not routinely resist the urge to urinate 6. Take showers instead of baths. 7. Urinate after sexual intercourse. 8. Women and girls should wipe from front to back after voiding to prevent contaminating the urethra with bacteria from the anal area. Urolithiasis Urolithiasis: The process of forming stones in the kidney, bladder, and/or urethra (urinary tract). Etiology: 1. Immobility. 2. Hypercalcemia. 3. UTIs. 4. Urine stasis. 5. Fractures. Clinical Manifestations: 1. Renal colic. 2. Nausea and vomiting accompanying severe pain. 3. Fever and chills. 4. Hematuria. 5. Rarely, oliguria or anuria. 6. Bladder distension (urine retention) Diagnostic tests: 1. KUB radiograph reveals visible calculi. 2. IVP (Intravenous Pyelogram) determines size and location of calculi. 3. Renal Ultrasonography reveals obstructive changes. Nursing Management: 1. Monitor intake of fluid amount and urinary output. 2. Medicate for pain as prescribed. 3. Continue antibiotic therapy as prescribed. 4. Correct diet to include reduced protein and calcium content. 5. Encourage plenty clear fluid intake. Acute Renal Failure Acute renal failure is a sudden, usually reversible deterioration in normal renal function. It can be classified according to underlying cause as: 1. Prerenal: a. Hypovolemia. b. Impaired cardiac efficiency. c. Vasodilatation. 2. Postrenal obstruction: a. Urinary tract obstruction. b. Tumors. 3. Intrarenal: a. Acute nephritis. b. Antibiotics. c. NSAIDs. Clinical Manifestations 1. Nausea and vomiting 2. Diarrhea 3. Decreased tissue turgor 4. Dry mucous membranes 5. Lethargy 6. Difficulty in voiding; changes in urine flow 7. Steady rise in serum creatinine 8. Fever 9. Edema Diagnostic Evaluation: 1. Serum creatinine level—the most reliable measure of the GFR, found to be rising 2. Radionuclide studies to evaluate GFR and renal blood flow and distribution 3. Urinalysis—reveals proteinuria, hematuria, casts 4. Ultrasonography to determine anatomic abnormalities Treatment: 1. Correction of any reversible cause of acute renal failure (ie, surgical relief of obstruction) 2. Correction and control of fluid and electrolyte imbalances 3. Restoration and maintenance of stable vital signs 4. Maintenance of nutrition with low-sodium, lowpotassium, low-phosphate, moderate-protein diet 5. Initiation of dialysis for patients with life-threatening complications Chronic Renal Failure Chronic renal failure is irreversible destruction of nephrons so that they are no longer capable of maintaining normal fluid and electrolyte balance. Causes: 1. Recurrent UTIs. 2. Toxic agents. 3. Diabetic nephropathy. 4. Uncontrolled hypertension. Complications: 1. Azotemia/uremia—nitrogen waste products accumulating in blood. Toxic levels manifest themselves in many ways such as coma, headache, gastrointestinal disturbances, neuromuscular disturbances. 2. Metabolic acidosis—as a result of decreasing GFR 3. Electrolyte imbalance 4. Severe anemia—kidneys unable to stimulate erythropoietin; uremic toxins deplete erythrocytes; nutritional deficiencies. 5. Hypertension—renal ischemia stimulates renin–angiotensin system. 6. Congestive heart failure Clinical Manifestations: 1. Decreased appetite and energy level 2. Increased urinary output and fluid intake 3. Bone or joint pain 4. Delayed or absent sexual maturation 5. Growth retardation 6. Dryness and itching of skin 7. Anemia 8. Markedly elevated BUN and creatinine Diagnostic Evaluation: Determine extent of disease; monitor progression. 1. Serum studies a. Decreased hematocrit, hemoglobin, Na+, Ca++; increased K+, phosphorous b. As renal function declines, BUN, uric acid, and creatinine values continue to climb. 2. Urine studies: a. Specific gravity—increased or decreased b. 24-hour urine for creatinine clearance is decreased (increased creatinine in urine) reflecting decreased GFR. c. Changes in total output 3. Many other tests may be ordered to evaluate othersystems and extent of disease (ie, chest x-ray, electrocardiogram) Treatment: 1. Correction of calcium phosphorous imbalance. Administer activated vitamin D to increase calcium absorption and calcium phosphate binders with meals to bind phosphate in the gastrointestinal tract. 2. Correction of acidosis with buffers such as Bicitra 3. Diets should meet caloric needs of the child containing adequate protein for development (1.0–1.5 g/kg per day). 4. Correction of anemia through the use of erythropoietin (Epogen) administered subcutaneously at home 5. Growth retardation should be evaluated for possible use of growth hormone. 6. Treatment options for end-stage renal disease are hemodialysis, peritoneal dialysis, or transplantation. 7. Institute dialysis therapy while transplant work-up is in progress. Nursing Management: A. Ensuring Safety 1. Protect the patient from the effects of decreased level of consciousness and involuntary movements by maintaining crib or bed side rails up and padded, as necessary. 2. Monitor for any seizure activity and have airway or tongue blade and suction equipment on hand. B. Educating About Chronic Renal Failure 1. Because numerous issues may interfere with the patient's psychological and social development and education, help the patient and family to cope with: a. Uncertainty regarding the course of the disease and ultimate prognosis. b. Abnormal lifestyle necessitated by dialysis. c. Burden of dialysis and continuous administration of medications. d. Fear of death, present in most children, adolescents, and family members