Thrombotic microangiopathy in HCV (+) renal allograft recipient
advertisement

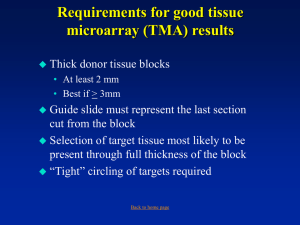
Thrombotic microangiopathy in HCV (+) renal allograft recipient Agnieszka Perkowska-Ptasinska Transplantation Institute, Warsaw Medical University, Poland HCV (+) male renal allograft recipient • native kidneys’ function loss due to nephroangiosclerosis at the age of 50, • KTX at the age of 55, • donor: cadaveric, female, age 45, cause of death: multiple injuries due to a car accident, • post-TX basic immunosuppression: Pred + MMF + tac • immediate graft function after KTX 4 weeks after KTX • serum creatinine concentration elevation, • platelet count, LDL, and haptoglobin levels: within normal limits → kidney transplant biopsy: - an acute vascular rejection (Banff IIA) - mild thrombotic microangiopathy - no C4d deposition. First graft biopsy (4 weeks after Tx) The 1st graft biopsy (4 weeks after Tx) Further course • good response to antirejection treatment (steroid pulse therapy) with the decrease in the serum creatinine concentration to the pre-rejection value of 1,0 mg/dl, • due to the biopsy findings: a change in the IS regimen: ↓tac MMF exposure A year after Tx • proteinuria of 2,0 g/day, • a rise in serum creatinine concentration to 1,3 mg/dl. A year after Tx • Clinically: signs of intravascular coagulation (mildly decreased platelet count, slightly elevated LDL and decreased haptoglobin levels), • no anti-HLA antibodies against class I and class II antigens in the serum, • further serological testing: anticardiolipin antibodies in IgG class, • HCV-PCR: high number of viral copies in patient’s blood, but the liver function tests normal. → 2nd graft biopsy The 2nd biopsy (a year after Tx) • LM: - acute lesions: thrombi in some of the glomerular capillaries and arterioles, - chronic lesions: double contouring of some of glomerular capillaries, IFTA I, moderate arteriolar hyalinisation, arterial intimal sclerotisation with mild reduction in vascular lumen, - no C4d deposition in PTCs, • the immunofluorescence: negative for Ig and complement components. • EM: electron-lucent expansion of the subendothelial zone with the deposition of basement membrane/lamina densa-like material. The 2nd graft biopsy (a year after Tx) The 2nd graft biopsy (a year after Tx) FINAL DIAGNOSIS Chronic active thrombotic microangiopathy, most probably due to HCV-related presence of anticardiolipin antibodies Further course • treatment: intravenous immunoglobulins and plasmapheresis, • response: - decrease in the anticardiolipin antibodies level - stabilization of renal function, and the level of proteinuria, • liver biopsy: mild chronic hepatitis with portal to portal (Ishak’s stage 3 ) fibrosis The patient is currently receiving antiviral therapy. Thrombotic microangiopathy after kidney transplantation • relatively common lesion (affects about 20% of kidney grafts recipients), may occur any time after TX, although the risk seems to be higher in the first 6 months after Tx, • may be clinically silent or overt, limited to the graft or widespread Thrombotic microangiopathy after kidney transplantation Prognosis: • depends on the etiopathogenesis of this process, • is better in TMA localized to the graft, • is better in cases limited to glomeruli • depends on the intensity of lesions (both acute and chronic): TMA may affect single arterioles and/or glomeruli, it may be also widespread and complicated by the focal infarcts of kidney tissue, Thrombotic microangiopathy after kidney transplantation Morphology of acute TMA: • edematous widening of the subendothelium in capillaries and arterioles, • mucoid thickening of the arterial intima, • the presence of fibrin and/or platelet thrombi within the wall or in the vascular lumen, • red cell fragmentation and entrapment within edematous vascular walls, • focal fibrinoid necrosis of the vascular wall (capillaries, arterioles, arteries), • in glomeruli: thrombi, mesangiolysis, collapse and wrinkling of GBM (acute ischemia) Thrombotic microangiopathy after kidney transplantation Morphology of chronic TMA: • glomeruli – double contours of capillary walls, - chronic ischemia of the tuft, - secondary FSGS without immunological complexes in IF, - in EM: thickening and reduplication of the glomerular capillary basement membrane with cellular interposition, • arteries – sclerotisation of the intima, in the early phase without the multiplication of the elastica, • arterioles – sclerotisation of the subendothelial region, - hyalinisation. Thrombotic microangiopathy after kidney transplantation Pathogenesis: Two broad categories: • the recurrence of TMA after Tx, • TMA that evolves de novo after Tx. The differentiation between the recurrent vs de novo TMA is not possible on morphological grounds. Thrombotic microangiopathy after kidney transplantation Recurrent TMA • usually within the first year (sometimes first days) after Tx, • in majority of cases the recurrence of TMA leads to the graft loss (70%) (3-years graft survival ± 50%) TMA recurrence after Tx – risk factors Types of common recurrences: • the deficiency of factors I, B, H, ADAMTS13 (vWF cleaving protease), • the presence of Ab against complement components, • antiphospholipid syndrome, • idiopathic HUS, • TMA in scleroderma, Very rare recurrences: • familial TMA caused by the deficiency of MCP and thrombomodulin (both are transmembrane proteins), • HUS associated with E.coli or S.dysenteriae infection TMA recurrence after Tx – risk factors The risk of TMA recurrence: • rises with older age of the disease presentation in native kidneys, • is higher in cases characterized by more dynamic evolution of TMA-dependant ESKD in native kidneys, • is higher in living-related donation, • is higher in patients treated with CNI TMA evolving de novo after KTX – risk factors • ischemia-reperfusion injury: - stimulates endothelial apoptosis, and the release of prothrombotic substances, • CNI toxicity, mTOR inhibitors toxicity: - direct injury to the endothelium, - suppression of antithrombotic factor C activity, - increased tissue thromboplastin and vWF multimers production, • OKT3 toxicity (currently very rare complication): - production of procoagulants by stimulated by OKT3 inflammatory cells, • acute graft rejection, especially ABMR: - T-cell, DSA toxicity to the endothelium, • viral infections: - direct injurious effect of the influenza virus A, CMV, HCV, HHV6, parvovirus), - indirect effect of CMV, HIV, HBV and HCV through the stimulation of anticardiolipin Ab production Conclusions • TMA is a relatively common complication after KTX, • it may have diverse clinical manifestation, it may be clinically silent, • it may be a recurrent phenomenon, or it may evolve de novo after Tx, • it’s pathogenesis is complex, and rarely definable solely upon the morphology of kidney graft biopsy, • the differentiation of TMA etiology requires additional diagnostic tools including serological (DSA, antiphospholipid antibodies, complement components) and virological testing