Sickle Cell and Transfusions
advertisement

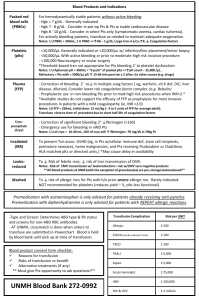
Sickle Cell and Transfusions Ashley Duckett, MD MUSC June 21, 2012 Transfusion • • • • Risks of transfusions Indications for transfusion Exchange transfusion Standardize care at MUSC • Largest users of US rare donor registry • Different antigens than on donor RBCs Transfusions • The good – Increase O2 carrying capacity & organ perfusion – Decrease percentage of HbS – Prevent organ damage • The bad – – – – – – Infection Volume overload Transfusion reactions Alloimmunization Iron overload Hyperviscosity Transfusion • If pt is new to MUSC, notify blood bank that pt has SCD – – leuko-reduced and phenotypically matched RBCs • Pts seen here from birth had a phenotype sent at 1 year old or before 1st transfusion Transfusion • If pt stable, high retic and simple pain crisis DO NOT need to transfuse • There is NO DATA that transfusion shortens the duration of a pain crisis • Expert opinion: NIH guidelines, Red Cross guidelines… Transfusion Reactions • Febrile nonhemolytic transfusion reactions – IF h/o febrile transfusion reactions should be premedicated (Benadryl, Tylenol) - ask the pt • Acute hemolytic transfusion reactions • Delayed hemolytic transfusion reactions • TRALI (transfusion associated lung injury) Alloantibodies • Almost 30% have alloantibodies – Need to give phenotypically matched RBCs (matched for C, E, Kell) – Ask pts if they have abs or if it takes a long time to find compatible blood • Anamnestic response delayed hemolytic transfusion reaction (life threatening!) – 5-20 days after a transfusion Iron Overload • Each unit of blood adds 200-250 mg Fe – Can’t phlebotomize anemic patients • • • • • • End organ damage – heart, liver, endocrine; Contributes to early death Serum ferritin, MRI (heart, liver, panc, spleen) Chelation therapy Desferal – req IV or SQ infusion Exjade (desferasirox)-only oral iron chelator – Side effects: N/V/D/abdominal pain, inc cr – Rare hepatic failure – need LFT monitoring Hyperviscosity • Blood from SS pt has higher viscosity than normal blood at same Hb • Deoxygenated sickle blood has 10x higher viscosity than oxygenated sickle blood at the same Hb • Increased viscosity means slow flow (esp in small vessels) and promotes sickling • DO NOT transfuse a sickle cell pt to a Hb of >10 Reasons to transfuse acutely • Symptomatic anemia – Severe fatigue, dyspnea, heart failure – Usually not until Hb <5 (NIH guidelines, 2002) • • • • • • Acute Chest Syndrome Acute CVA Aplastic crisis (remember short RBC life span) Preop Hepatic or Splenic sequestration Priapism (second line because of ASPEN) – Exchange transfusion- (Erythrocytapharesis) • VERY SICK pts – multiorgan failure, impending respiratory failure, hepatic sequestration • Pts with Hb too high for simple transfusion or need to rapidly decrease HbS fraction Exchange transfusion • Need to know pts HbS fraction – Understand HbS fraction – Indicated when HbS>80%, goal <30% • Maybe with lower fraction if Hb is >8-9 – STAT Hb electrophoresis, call path and let them know • Call pheresis team and determine access – Dialysis cath, now new ports? Preoperative Transfusions • Multicenter study of 604 surgical patients • Randomized to aggressive (Hb S<%30) vs conservative (Hb 10) transfusion regimen • Serious complications were the same (acute chest in 10%) except more transfusion rxns in aggressive group • ?SC or B+ thal pts with high baseline Hb Vichinsky et al; NEJM 1995;333 206-13 Preop transfusions • Cochrane review Jan 2012 – 2 studies (NEJM and study from Bahrain) and observational data from 3rd world countries – Is no tx = to simple transfusion? “Conservative therapy appears to be as effective as aggressive therapy in preparation for surgery in people with sickle cell disease, further research is needed to examine the optimal regimen for different surgical types, and to address whether preoperative transfusion is needed in all surgical situations”. 14 Chronic transfusions • Benefits must outweigh known risks • Primary and secondary prevention of CVA (STOPI and STOPII trials) • Recurrent acute chest, debilitating pain • Symptomatic anemia with renal failure unresponsive to epo • Pulmonary hypertension • Heart failure • ?Priapism, Leg ulcers • Sickle cell progress note • Transfusion criteria on OACIS • Dr Greenberg, Dr Sherron Jackson 16 References • Inati, Adlette. Recent advances in improving the management of sickle cell disease. Blood Reviews, 2009 Dec; 23 Suppl 1:S9-13. • Yazdanbakhsh, K et al. Red blood cell alloimmunization in sickle cell disease: pathophysiology, risk factors, and transfusion management. Blood, 2012. May 4. [Epub ahead of print] • Smith-Whitely, K and Thompson, AA. Indications and complications of transfusions in sickle cell disease. Pediatr Blood Cancer. 2012 Aug;59(2):358-64. [Epub 2012 May 4.] • American Red Cross. Practice Guidelines for Blood Transfusion, Second Edition, April 2007 The Management of Sickle Cell Disease, 4th ed. NIH Publication No. 02-2117. Revised May 28, 2002 (Forth Edition) National Institutes of Health, National Heart, Lung, and Blood Institute Hirst C, Williamson L. Preoperative blood transfusions for sickle cell disease. Cochrane Database of Systematic Reviews 2012, Issue 1. Art. No.: CD003149. DOI: 10.1002/14651858.CD003149.pub2 • •