Urinary Tract Infection
advertisement

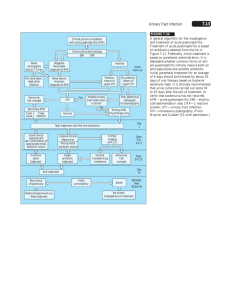
Urinary Tract Infection 2nd Affiliated Hospital ZJ University Yu Gong Epidemiology of UTI by Age Group and Sex Balance Host Pathogen Host defenses: miscellaneous • Multi-layer transitional cells • Urinary immunoglobulins : Tamm-Horsfall protein • Spontaneous exfoliation of uroepithelial cells with bacterial detachment • Mechanical flushing of micturition Come with a rush, go with a flush! Pathogens Bacteria of UTI • • • • • • • • • • Bacterial Species Outpatients (%) Escherichia coli 89.2 Proteus mirabilis 3.2 Klebsiella pneumoniae 2.4 Enterococci 2.0 Enterobacter aerogenes 0.8 Pseudomonas aeruginosa 0.4 Proteus species 0.4 Serratia marcescens 0.0 Staphylococcus epidermidis 1.6 Staphylococcus aureus 0.0 Inpatients (%) 52.7 12.7 9.3 7.3 4.0 6.0 3.3 3.3 0.7 0.7 Opportunistic pathogens Fungal Pathogens Most such infection occurs in patients : • with long indwelling Foley catheters • receiving broad-spectrum antibacterial therapy • diabetes mellitus • on corticosteroids Other Pathogens • C. Trachomatis • U. Urealyticum Chronic Urethritis Chronic Prostatitis Urinary Tract Infection (UTI) • Upper UTI-pyelonephritis (renal abscess, perinephric abscess, Surgical kidney) • Lower UTI -cystitis (urethritis) Surgical kidney Pyelonephritis Pyelonephritis —— inflammation of the kidney and its pelvis PATHOGENESIS How bacteria reach the urinary tract in general and the kidney in particular? Pathogenesis Two potential routes : (1) hematogenous infection bacteremia → kidney (Descending) (2) retrograde infection urethra→bladder→ ureter →kidney (ascending) Hematogenous Infection Because the kidneys receive 20% to 25% of the cardiac output, any microorganism that reaches the bloodstream can be delivered to the kidneys. Hematogenous Infection Existing infection (skin, respiratory tract) blood circulation small abscess renal papillary kidney(cortex) renal tubular renal pelvis PATHOGENESIS Factors predisposing to pyelonephritis • Urinary Tract Obstruction • Vesicoureteral Reflux • Instrumentation of the Urinary Tract • Pregnancy • Diabetes Mellitus How long will there be possibility of UTI after urethral catheterization? Diabetes Mellitus • 3-4 times UTIs in DM than in non-diabetes • Diabetic neuropathy and vascular injury affects bladder emptying(paralytic bladder) • hyperglycemia impact host immuno system Clinical Presentation • • • • • fever back pain colicky abdominal pain nausea and vomiting Sepsis, septic shock Clinical Presentation Cystitis • Suprapubic region pain • frequency, urgent urination, odynuria and dysuria Complications • Sepsis • Peri-renal abscess • Renal papillary necrosis/Acute renal failure Laboratory findings • Urine dipstick pyuria on microscopic examination urine WBC > 3 WBC/high-power field • Middle stream urine culture bacterial account > 105cfu/ml (cfu:clony-forming units) • blood culture Treatment • Rest • Drinking large amount of water • Antibiotics: 2 weeks / until symptom free • Treat related diseases: diabetes, renal stones, etc Antibiotic therapy • Objective - prevention of sepsis - eradication of organism - prevention if recurrences • Medications - trimethoprim-sulfamethoxazole(SMZ) - fluoroquinolones - ampicillin Catheter-associated UTI • Over 1 million catheter-associated UTIs occur in the US each year • Risk factors: duration of catheterization: mostly at 72 hours after catheterization (Bacteria film) Remove catheter as early as possible Change catheter Any abnormalities of structural, or functional causes should be excluded when UTI was diagnosed and treated. Take radical measures, insted of providing temporary solutions 治标,更要治本 Genitourinary Tuberculosis Epidemiology • 8~10 million new active cases of TB each year(WHO) • TB is the most common opportunistic infection in AIDS patients(WHO) Transmission and Development • Genitourinary TB is caused by metastatic spread of the organism through bloodstream during initial infection (hematogenous). • Kidney is usually the primary organ infected in urinary disease • Primary site for infection of genital system is often the epididymis in men and the fallopian tubes in women Pathological renal TB Parenchyma to Collecting system Clinical renal TB Clinical Features • • • • Most patients are aged 20~40 years Some cases with Pulmonary tuberculosis Bladder is always the spokesman for renal TB Urologist should always consider the diagnosis of genitourinary TB in a patient presenting with vague, long-standing urinary symptoms for which there is no obvious cause Diagnosis • Urine examination (Sterile pyuria, pH<7, WBC, RBC, Pro) • Urine : Acid-fast bacilli (AFB) • Blood: TB-Antibody • Imageology (Ultrasonography, Plain film, IVU, RGP, CU, CTU, ) • Cystoscopy and Biopsy Acutely inflamed ureteric orifice Tuberculosis bullous granulations Hyperemia and tuberculosis ulcer 1. Severe calyceal and parenchymal destruction Multiple stricture of ureter Moth-eaten sign 2. Contracted bladder RGP Autonephrectomy Lateral renal tuberculosis, Contralateral hydronephrosis Calcification, parenchymal scarring, hydrocalycosis, thickening of the walls of renal pelvis Painting petal Extensive tuberculosis of kidney Antituberculous drugs Isoniazid(INH), Rifampicin(RFP), Streptomycin(SM), Pyrazinamide(PZA), Ethambutol(EMB), PAS Surgery 1. Excision of diseased tissue (Partial )Nephrectomy, Abscess Drainage, Epididymectomy 2. Reconstructive Surgery Ureteral stricture, Augmentation cystoplasty, Urinary conduit diversion(Bricker’s procedure, ileum conduit), orthotopic Neobladder Thank You