2 months
FMT in Pediatric IBD
Michael Docktor, MD
Boston Children’s Hospital
August 16, 2014
Disclosures
• I have no relevant disclosures or financial obligations
2
Outline
I. Brief background
II. Anecdotal experience at Boston
Children’s
III. Oh and by the way, they have IBD
IV. Pediatric FMT in ulcerative colitis
V. Pediatric FMT in Crohn’s disease
VI. Future directions
3
Kostic, et al. Gastro. 2014; 146(5): 1489-1499
Our experience: FMT for IBD
“Innovative Therapy”
• 7 patients with recalcitrant IBD
– Ages 12-17 yrs. (average 15 yrs.), 3 M / 4 F
– 4 UC, 2 CD, 1 IC
– Related donor FMT via colonoscopy and f/u home enemas
• All seven were recommended escalation of therapy
– 85% (6/7) recommended Tacrolimus +/- surgical colectomy
• All 6 were steroid dependent at time of FMT
Our experience: FMT for IBD
“Innovative Therapy”
• 85% (6/7) stabilized and were weaned from steroids
– 57% (4/7) improved but remained stable on previous therapy
– 28% (2/7) discontinued steroids, biologic and 6-MP
• 1 in deep clinical remission on 5-ASA & Vancomycin 2+ years
• 1 with mild activity, de-escalated to 5-ASA
– 15% (1/7) continued to slowly worsen, Tac surgical colectomy 9 months later
• No adverse events reported, all procedures and f/u well tolerated up to 2.5 years out.
Docktor M, et al. Unpublished data 2011-2013
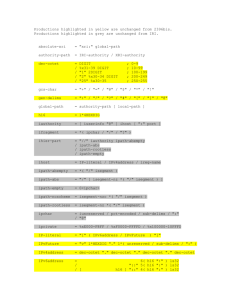
Microbial analysis of FMT
Firmicutes
Post-FMT
(48 Days)
Post-FMT
(3 Days)
Donor
Pre-FMT
OTU Log Abundance
(Fraction of all reads)
0 1 2 3 4
Shannon Diversity
(Log-Scale)
5
Docktor M, et al. Unpublished data 2011-2013
• 10 children with RCDI (1-19 years)
• Open label single, related FMT via NG tube (2) or colonoscope (8)
• 3/10 patients had concomitant IBD
• Overall success rate 90% for curing RCDI
– 7/7 (100%) among non-IBD patients
– 2/3 (66%) among IBD patients
Russell GH, et al. JPGN. 2014; 58(5): 588-592.
8
Russell GH, et al. JPGN. 2014; 58(5): 588-592.
• 11 y/o M with CD
• Counted as failure
• Redeveloped CDI after readmission 2 months
Russell GH, et al. JPGN. 2014; 58(5): 588-592.
10
• 19 y/o F with UC
• Admitted for severe, acute colitis
• 100% better for 5 days then severe bloody diarrhea
• Never redeveloped CDI
• Potential fulminant UC flare secondary to
FMT?
Russell GH, et al. JPGN. 2014; 58(5): 588-592.
11
Fecal Microbiota Transplantation in Children with
Recurrent Clostridium difficile Infection
Anne Pierog, MD, Ali Mencin, MD, and Norelle Rizkalla Reilly, MD
Columbia University Medical Center,
Division of Pediatric Gastroenterology, Hepatology and Nutrition
• 6 patients with RCDI
– Ages 4-21 yrs., 4 M / 2 F
– 1 CD, 1 IC
– Related donor FMT via colonoscopy
• 100% cure rate for C. diff
• 12 y/o M with CD
– Initial clinical improvement @ 1 week
– Acute appendicitis @ 2 weeks post FMT
– Clinical “remission” with optimized therapy @ 12 weeks
• Follow up: both IBD patients cured of CDI, required escalation of IBD therapy
Pierog A, et al. Peds Infec Dis Journ . Accepted for publication.
12
FMT FOR PEDIATRIC
ULCERATIVE COLITIS
• Safety and tolerability of FMT via enema in 9 children w/
UC
• 7 – 21 years, mild-moderate disease (PUCAI 15-65)
• Daily enemas x 5 days
– 78% (7/9) showed clinical response within 1 week
– 67% (6/9) maintained clinical response at 1 month
– 33% (3/9) achieved clinical remission at 1 week
• FMT via enema was feasible and tolerable in children with limited side effects.
Kunde S, et al. JPGN 2013 Jun;56(6):597-
601
Kunde S, et al. JPGN 2013 Jun;56(6):597-
601
Fecal Microbial Transplant via Nasogastric tube for active
Pediatric Ulcerative Colitis
David L. Suskind 1 M.D., Namita Singh 2 M.D., Heather Nielson, Ghassan
Wahbeh 1 M.D.,
• Open label single FMT via NG tube
• Four male patients, 14.5 ± 1.7 years
• Pretreatment with Rifaximin TID x 3 days
• Follow up @ 2, 6, 12 weeks
– Mild symptoms including vomiting and bloating
– 2/4 developed C.diff
within 4 months (1 recurrence)
– No change in PUCAI, CRP, albumin, HCT
• Overall safe but not efficacious
Suskind D, et al. JPGN. Accepted for publication.
16
FMT FOR PEDIATRIC
CROHN’S DISEASE
Fecal Microbial Transplant Effect on Clinical Outcomes and Fecal Microbiome in Active Crohn’s disease
David L. Suskind MD 1 , Mitchell J. Brittnacher PhD 2 , Ghassan Wahbeh MD 1 , Michele L. Shaffer PhD 1 ,
Hillary S. Hayden 2 , Namita Singh MD 3 , Christopher J. Damman MD 4 , Kyle R. Hager, Heather Nielson,
Samuel I. Miller MD 2,4,5,6
• Nine pediatric patients
– Mild to moderate Crohn’s (PCDAI of 10-29)
– 12-19 years
– Open label NGT delivery of related donor FMT
• Studied
– Clinical response (PCDAI, CRP, calprotectin)
– Engraftment & % similarity to donor
– Microbial changes
Suskind DL, et al. Seattle Children’s Hospital. Data in submission for print.
18
Fecal Microbial Transplant Effect on Clinical Outcomes and Fecal Microbiome in Active Crohn’s disease
David L. Suskind MD 1 , Mitchell J. Brittnacher PhD 2 , Ghassan Wahbeh MD 1 , Michele L. Shaffer PhD 1 ,
Hillary S. Hayden 2 , Namita Singh MD 3 , Christopher J. Damman MD 4 , Kyle R. Hager, Heather Nielson,
Samuel I. Miller MD 2,4,5,6
Suskind DL, et al. Seattle Children’s Hospital. Data in submission for print.
Fecal Microbial Transplant Effect on Clinical Outcomes and Fecal Microbiome in Active Crohn’s disease
David L. Suskind MD 1 , Mitchell J. Brittnacher PhD 2 , Ghassan Wahbeh MD 1 , Michele L. Shaffer PhD 1 ,
Hillary S. Hayden 2 , Namita Singh MD 3 , Christopher J. Damman MD 4 , Kyle R. Hager, Heather Nielson,
Samuel I. Miller MD 2,4,5,6
• 7/9 (78%) Had PCDAI fall < 10 @ 2 weeks
– 2 required escalation of Rx
• 5/7 (71%) Remained < 10 @ 12 weeks
• No or modest improvement in patients without engraftment
• More divergent = better engraftment and response
Suskind DL, et al. Seattle Children’s Hospital. Data in submission for print.
Fecal Microbial Transplant Effect on Clinical Outcomes and Fecal Microbiome in Active Crohn’s disease
David L. Suskind MD 1 , Mitchell J. Brittnacher PhD 2 , Ghassan Wahbeh MD 1 , Michele L. Shaffer PhD 1 ,
Hillary S. Hayden 2 , Namita Singh MD 3 , Christopher J. Damman MD 4 , Kyle R. Hager, Heather Nielson,
Samuel I. Miller MD 2,4,5,6
Time relative to FMT (days)
Suskind DL, et al. Seattle Children’s Hospital. Data in submission for print.
21
Fecal Microbial Transplant Effect on Clinical Outcomes and Fecal Microbiome in Active Crohn’s disease
David L. Suskind MD 1 , Mitchell J. Brittnacher PhD 2 , Ghassan Wahbeh MD 1 , Michele L. Shaffer PhD 1 ,
Hillary S. Hayden 2 , Namita Singh MD 3 , Christopher J. Damman MD 4 , Kyle R. Hager, Heather Nielson,
Samuel I. Miller MD 2,4,5,6
Time relative to FMT (days)
Suskind DL, et al. Seattle Children’s Hospital. Data in submission for print.
22
Fecal microbial transplantation in a one-yearold girl with early onset colitis - caution advised
Vandenplas Y, Veereman G, van der Werff ten Bosch J, A. Goossens, Pierard
D, Samsom JN, Escher JC
Vandenplas Y, et al. JPGN. 10.1097/MPG.0000000000000281.
Vandenplas Y, et al. JPGN. 10.1097/MPG.0000000000000281.
From healthy age matched niece
7- 14 days of remission
Vandenplas Y, et al. JPGN. 10.1097/MPG.0000000000000281.
From older brother
Vandenplas Y, et al. JPGN. 10.1097/MPG.0000000000000281.
FMT
From older brother
FMT
FMT
Vandenplas Y, et al. JPGN. 10.1097/MPG.0000000000000281.
FMT
Remission 1 month
From older brother
FMT
FMT
Vandenplas Y, et al. JPGN. 10.1097/MPG.0000000000000281.
FMT
Remission 1 month
From older brother
FMT
Remission 2 month
FMT
Vandenplas Y, et al. JPGN. 10.1097/MPG.0000000000000281.
FMT
From older brother
FMT
FMT
Remission 1 month
Remission 2 month
Remission 6 month
Clinical Trials
• NCT01096635 – DBPCT using FMT to treat chronic active UC
(Padaramothy, New South Wales)
• NCT02049502 – FMT to treat active UC associated post-IPAA pouchitis
(Shaffer, Emory)
• NCT0184717- FMT effect on the IBD microbiome
(Moss, Beth Israel)
• NCT01947101 – FMT as a transition off immunosuppression with stable UC
(Kellermeyer, Baylor)
Summary
• FMT appears safe and well tolerated in children independent of route
• Efficacious for RCDI
• Mixed response in IBD
– Best route ?
– Pre-FMT antibiotics ?
– Donor matching ?
– Durability / maintenance ?
32
The road ahead
33