dr. antoine hage`s lecture from 4/10/13
advertisement
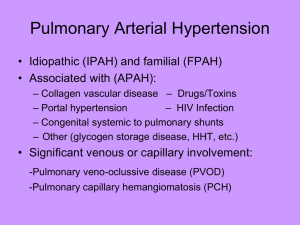
Role of the Echocardiogram in the Assessment of Pulmonary Hypertension and the Right Ventricle Antoine Hage, M.D Director, Solid Organ Transplant Cardiology Co-Director, Pulmonary Hypertension Program Cedars Sinai Heart Institute Clinical Professor of Medicine/ Cardiology David Geffen School of Medicine at UCLA Role of Echocardiography in Pulmonary Hypertension: Overview • Definition and classification • Role of ECHO in – Diagnosis (allows identification of patients for whom RHC is required) – Screening high risk patient populations – Evaluation of Structure/ Morphology/ Function/ Hemodynamics of RV and PA (CHD) – Determining etiology / PH group (PAH vs PVH) and secondary causes – Risk stratification (Evaluation of functional and hemodynamic impairment) – Formulating therapeutic options, monitoring disease stability and response to therapy (longitutudinal F/U) – Prognostic evaluation 2 Hemodynamic Definition of PH/PAH PH PAH Mean PAP ≥25 mm Hg Mean PAP ≥25 mm Hg plus PCWP/LVEDP ≤15 mm Hg ACCF/AHA CECD includes PVR >3 Wood Units Badesch D et al. J Am Coll Cardiol. 2009;54:S55-S66. McLaughlin VV et al. J Am Coll Cardiol. 2009;53:1573-1619. 1. PAH •Idiopathic PAH •Heritable (BMPR2, ALK1, Endoglin) •Drug- and toxin-induced •Persistent PH of newborn •Associated with: −CTD −HIV infection −portal hypertension −CHD −schistosomiasis −chronic hemolytic anemia 3. PH Owing to Lung Diseases and/or Hypoxia •COPD •ILD •Other pulmonary diseases with mixed restrictive and obstructive pattern •Sleep-disordered breathing •Alveolar hypoventilation disorders •Chronic exposure to high altitude •Developmental abnormalities 4. CTEPH 1’. PVOD and/or PCH 5. PH With Unclear Multifactorial Mechanisms 2. PH Owing to Left Heart Diseases •Systolic dysfunction •Diastolic dysfunction •Valvular disease Simonneau G et al. J Am Coll Cardiol. 2009;54;S43-S54. •Hematologic disorders (MPD, splenectomy,..) •Systemic disorders (sarcoidosis, LAM,..) •Metabolic disorders (e.g Thyroid disorders,.. ) •Others (e.g Renal failure/ dialysis, fibrosingmediastinitis,..) When to Suspect and Screen for PAH • • • • • • • • Family history – 6% - 12% prevalence of positive family history. If BMPR2 present, 20% chance of developing PAH. – Autosomal dominant, incomplete penetrance, genetic anticipation Connective tissue disease – Limited and diffuse scleroderma: 8%- 30% – CREST: up to 20% - 25% – Systemic lupus erythematosus: 4% - 14% – Rheumatoid arthritis up to 21% Congenital Heart Disease – Reversal of left-to-right shunt – Ventricular septal defect, patent ductusarteriosus, atrialseptal defect Portal hypertension – Nearly 10% have elevated right ventricular systolic pressure by echo and RHC. – 4% have severe PAH to contraindicate liver transplantation Deep venous thrombosis/history of pulmonary embolism – Up to 3-4% of survivors Appetite suppressant or stimulant use – 1/20000 of Fen Phen users more than 3 months – Methamphetamine use HIV – 0.5% (1/200) patients. Sickle cell disease, hemodialysis patients, etc Echocardiography in Pulmonary HTN Echocardiography is an integral part of the assessment of a patient with PH, Often the first test to detect PH Evaluates cardiac structure, function and hemodynamics Rules out congenital heart diseases and shunts* Provides a reasonably accurate estimate of pulmonary artery pressures Guides diagnosis and therapy Helps determine prognosis: Many Echo parameters are prognostic indicators: •RV size and function (eg,TAPSE, S’, FAC, MPI/TEI index) • Pericardial effusion • Estimate of CO/CI and RA pressure (hemodynamics) * May need TEE 6 Role of Echocardiography in the Screening of Patients at Risk of Developing PH/ PAH When to Suspect and Screen for PAH • Family history/ Heritable PAH • Connective tissue disease • Congenital Heart Disease • Portal hypertension • Deep venous thrombosis/ history of pulmonary embolism • HIV patients • Appetite suppressant or stimulant use (Methamphetamine) • Sickle cell disease, hemodialysis patients/fistula, sarcoidosis, post-splenectomy etc. Echocardiographic Criteria Corresponding to Various Levels of Likelihood of Presence of Pulmonary Hypertension Peak tricuspid jet velocity m/sec Estimated sPAP mm Hg Other echo signs of PH present* PH ( grade of evidence) < 2.8 <36 No Unlikely (I-B) < 2.8 <36 Yes* Possible (IIa- C) 2.9 - 3.4 37 - 50 No Possible (IIa-C)# > 3.4 > 50 Yes/No Likely (I-B) * Eg, if RV morphology and function and/or systolic time intervals such as PAAT, or mid systolic deceleration of right ventricular ejection (notching) are suggestive of PH, such diagnosis should be considered “possible” even if Doppler estimate of sPAP is within normal range . # TRV > 2.8 m/Sec corresponds to TIPG > 31 mm Hg, suggest PH except in elderly or very obese patients Galie N, et al: EurRespir J. 2009; 34; 1219-1263 Screening Patient Groups at Risk of Developing PAH • Yearly echocardiography is recommended in patients – At risk for heritable PAH – With CTD, especially patients with scleroderma • Some recommend echo Q 2 years if normal BNP and : – DLCO > 70% and – FVC% /DLCO% < 1.6 – • With sickle cell disease Echocardiography should be considered, in patients with PHsuggestive symptoms – – – – – – After pulmonary embolism With HIV infection With portal hypertension With prior appetite suppressant use With sarcoidosis After splenectomy 10 Limitations of Echocardiography in PAH • • • • • • • 1,2 Experienced technicians and interpreting physicians are essential Consistency of skilled technicians/readers – Applies to all imaging modalities Images can be limited in some patient populations The RV, the chamber of highest concern in PAH, is the least emphasized on the “standard” echocardiography exam TR jet may be absent in some patients, thus precluding PASP assessment May overestimate or underestimate actual pulmonary arterial pressure Can estimate LVEDP (PCWP) or CO/CI, but may prove impractical CI, cardiac index; CO, cardiac output; LVEDP, left ventricular end diastolic pressure; PASP, pulmonary arterial systolic pressure; PCWP, pulmonary capillary wedge pressure; RV, right ventricle; TR, tricuspid regurgitation. 1. Cheitlin et al. Circulation. 1997;95:1686-1744. 2. McGoon et al. Chest. 2004;126:14S-34S. 11 ECHO FEATURES OF PULMONARY ARTERIAL HYPERTENSION ECHO FEATURES OF PULMONARY ARTERIAL HYPERTENSION Right atrial enlargement Right ventricular enlargement/dilatation - D-shaped LV on short axis Right ventricular hypertrophy Significant tricuspid regurgitation – (TR jet estimated RVSP is 4V2 + RAP) Right ventricular dysfunction Pulmonary regurgitation - PR jet estimated mPA and PAEDP Reduced RV outflow tract velocity, short acceleration time Dilated IVC not collapsing with respiration (if patient not ventilated) Patent foramen ovale (bubble contrast used) Pericardial effusion Dilated pulmonary arteries 12 Echocardiographic Findings that Increase Clinical Suspicion of PVH •Absence of right heart chamber enlargement or pericardial effusion • Evidence of left atrial enlargement • Presence of left ventricular hypertrophy • Impaired diastolic relaxation indices • Elevated left ventricular filling pressures as determined by E/e’ ratio >15 (most reliable predictor of LA pressure >15 mmHg) • Extent of functional MR and size of mitral valve regurgitant orifice at rest or during exercise (predictor of increased PA and pulmonary edema in ischemic heart disease and probably in HFpEF) • Modest elevation of pulmonary pressures (i.e., 60’s rather than > 80’s) 13 Findings that Increase the Clinical Suspicion of PVH • Age (elderly) • Female gender • Obesity • Systemic Htn (particularly if not optimally controlled) and LVH • Diabetes mellitus • Coronary artery disease • Obstructive sleep apnea • Atrial fibrillation Lack of right axis deviation Lack of right atrial enlargement or RVH Evidence of left atrial enlargement Evidence of left ventricular hypertrophy Pulmonary vascular congestion/ Kerley B lines Pulmonary edema Pleural effusion 14 Progression of RV Dysfunction in PAH Champion H C et al. Circulation 2009;120:992-1007 15 Role of Echo in Diagnosis of PH and Assessment of PA / RV Hemodynamics Estimating Pulmonary Artery Pressures by Echo TR Mean PR TR TR Diast 2* SPAP = 4TR Vmax2 + RAP Diast PA = 4PRend Vmax2 + RAP Mean PA = TR Vmean+ RAP Or = 4PR Vmax2 + RAP TR Vmax= Peak TR velocity PRend Vmax= End PR velocity PR Vmax= Peak PR velocity TR Vmean=from VTI Modified from Garvan Kane Mean Pulmonary Artery pressure • The most reproducible method to estimate mean PA pressure is based on the mean Doppler gradient of the tricuspid regurgitant (TR) signal Mean PA Pressure Mean systolic = RV-RA gradient Aduen JF, et al. J Am Soc Echocardiogr. 2009: 22; 814-819 Estimated RA+pressure Pulmonary Artery Mean and Diastolic Pressures mPAP = 79 – 0.45x (PAAT) = 79 - 0.45x (130) =79-59 = 20 mm Hg PA Diastolic Pressure • [PADP = 4 x (end-diastolic pulmonary regurgitant velocity)² + RA pressure] Mean PA Pressure •mPAP = 1/3(SPAP) + 2/3(PADP) • Or 4 x (early PR velocity)² + estimated RA pressure •Or: 0.61 xsPAP + 2 mm Hg ( Chemla’s Equation) •Or: 79 - 0.45 x (PAAT) • Or: 90 – (0.62 x PAAT) • Or mPAP= 80 – 0.5 x (PAAT) •Or: RAP + VTI of TR jet mPAP =79 – 0.45x (PAAT) =79- 0.45x (70) = 79 – 32 = 47 mm Hg CHEST. 2011;139(5):973-975. Pulmonary Acceleration Time PV AccT 72 ms mPA = 47 mm Hg Mean PA pressure = 79 - (0.45 x AT) PA in Pulmonary vascular disease CTEPH- Before PTE Same pt After PTE Right Atrial Pressure Estimate: IVC and Hepatic Vein Right atrial (RA) pressure estimate should not not be based on an arbitrary value, but rather based on 2D and Doppler imaging of the IVC and hepatic veins* Modified from Garvan Kane *Hepatic veins > 11 mm is abnormal Right Atrial Pressure Estimate: IVC and Hepatic Vein American Society of Echocardiography Recommends: • 3mmHg, IVC diameter <21mm w/ >50% collapse • 8mmHg, IVC normal in diameter w/ <50% collapse • 15mmHg, IVC diameter >21mm w/ >50% collapse • 20mmHg, IVC dilatation with <50% collapse 23 Right Atrial Pressure Estimate: Hepatic Vein Flow in PAH Patients •Systolic filling fraction: Vs/ (Vs + Vd) < 55% sensitive and specific for increased RA pressure • Abnormal: A wave is larger than systolic S wave Abnormal A A A D S S D Normal: Systolic predominance in hep. vein flow Abnormal: Vs/Vd< 1 (eg; High RA pressure) D How should you define mild, moderate, and severe PH? • Not by RVSP • Not by the ratio of RVSP to systemic BP • Define PH severity by the degree of: – RV dilatation – RV dysfunction – RA pressure elevation – Decrease in cardiac index Modified from Garvan Kane Right Ventricular Afterload RESISTANCE PVR: mean PAP – PCWP = TPG Flow (CO) CO Reflects the arterial load to steady flow Doppler correlate: Peak TR pressure gradient / RVOT TVI (although does not incorporate LV filling pressure) Modified from Garvan Kane PVR PVR = [(TRV/TVIRVOT) x 10] + 0.16 (Abbas Formula)* = (3.9 / 10.2) x10 + 0.16; = 0.38 x10 + 0.16; = 3.8+ 0.16 = 3.98 WU PVRc = (RVSP – E/e’) / VTIRVOT (Corrected Dahiya equation)# *Abbas, AE et al. JACC 2003. 41: 1021-1027 #Dahiya, A et al . Heart 2010. 96: 2005-2009 PA – W Sign Right Ventricular Afterload Compliance / Capacitance Can be estimated by SV / Pulse Pressure (by cath or ECHO) May be as (more) important in PH as resistance Pulsatile component of pressure and flow is 30-50% of power transferred from RV to pulmonary bed Less than 1.0 is abnormal and < 0.8 mL/mm Hg predicts mortality in PAH patients PVCAP = Stroke Volume = LVOT Area x TVI PA Pulse Pressure* 4 (TR Vmax2 – PRendV2) PVCAP = Pulmonary vascular capacitance * PA systolic – PA diastolic Mahapatra, S et al. J. Am Soc Echocardiogr, 2006, 19: 1045-1050 Indirect Echocardiographic Findings in PH PV AccT 72 ms = 47 mm Hg Mean PA pressure : = 79 - (0.45x PAAT) • Or = 90 – (0.62 x PAAT) • Or =80 – 0.5 x (PAAT) • RVOT Acceleration time < 90 msec •“Flying W” sign by M-Mode (mid-systolic notching) • Dilated Coronary Sinus Reynolds, BS, RDCS, Terry. The Echocardiographer’s Pocket Reference. Arizona: 2007. Print. 30 Echocardiographic Features of PAH US/DS/MAR11/001 RV Apical 4 Chamber view: Obtain apical long axis views optimized to visualize RV RV centric LV centric RA / RV Morphology in PAH RV Dilatation / LV Compression RAE / IAS Displacement Flattening / D-shaped Septum Apex-forming RV RV size: Qualitative “Eyeball” Estimate Normal Normal Mild RVE RV Similar to LV/ Shares apex RV 2/3 size of LV Moderate RVE RV Larger than LV Severe RVE Very large RV/ Apex forming D shaped septum Quantitative Estimate of RV Size Length (> 86 mm*) Mid diameter (> 35 mm*) Basal diameter (>42 mm*) RV area > 28 cm2* * Measures indicate dilatation • RV end-diastolic diameter has been identified as a predictor of survival in patients with chronic pulmonary disease Tips • Measure at end diastole from an RV focused apical 4-chamber view • Optimize image to have maximum diameter without foreshortening the ventricle Rudski,LG et al. J. Am Soc Echocardiogr 2010.23: 685-713 US/DS/MAR11/001 RVH: RV thickness > 0.5 cm RV measurements in 2D • RV end-diastolic diameter has been identified as a predictor of survival in patients with chronic pulmonary disease • RV Enlargement: RVD1 > 42 mm or RVD2 > 35 mm or RV Length > 79 mm RV Area > 28 cm2 J Am Soc Echocardiogr 2010;23:685-713. RVH: RV thickness > 0.5 cm 36 Septal Flattening- Eccentricity Index D1 D2 Eccentricity Index : D1/D2 > 1 In Diastole= volume overload In Systole= volume and pressure overload E.I = 40/25 = 1.6 (D1/D2) 37 Pericardial Effusion: A bad Sign in PH • Associated with greater disease severity • Increases mortality risk • Likely reflects high venous pressure and poor lymphatics drainage rather than a risk of cardiac tamponade Echo and RV Function • 3D ECHO might become gold standard • No other valid quantitative assessment of RV function – – – – – – – – Subjective evaluation Tricuspid annular plane systolic excursion (TAPSE) Tricuspid annulus TDI velocities (S’) RIMP (Tei Index) RV area fractional shortening Dp/dt RV longitudinal strain measurement Measurement of cardiac output Echo measures of RV Function: TAPSE TAPSE • Simple, reproducible • Represents longitudinal function • Correlates well with radionuclide angiography in determining RV systolic function. Relatively load dependent. • Normal > 20 mm. • TAPSE < 18 mm has negative prognostic implications • Angle and load dependent To execute: – In Apical-4 chamber view, place M-Mode cursor through the lateral tricuspid annulus – Measure excursion from end-diastole to end-systole – Average over 3 beats – Off-axis views tend to overestimate TAPSE (as with the apex-forming RV) J Am Soc Echocardiogr 2010;23:685-713., Heart 2006;92:i19-i26 doi:10.1136/hrt.2005.082503 40 Echo Measures of RV Function: TV annular velocity (S’) by TDI TV Annular velocity s’ • MPI=(TCO-ET)/ET • Simple, sensitive, reproducible • Good indicator of basal free wall function • By TDI, several indices of RV function can be obtained from a single cardiac cycle Peak velocities Isovolumic parameters Tei index • Angle dependant • Relatively independent of loading conditions • Correlated with RVEF by first pass radionuclide ventriculography •Normal > 10 cm/s • Normal MPI by TDI < 0.55 The RV Index of Myocardial Performance (RIMP) Global Indicator of Systolic and Diastolic Function. • Needs the measurements of 2 different cardiac cycles (tricuspid inflow and RV outflow by PW Doppler) • Normal values below 0.4 (mean 0.28) • Relatively independent of HR and from loading conditions • Prognostic in PH • May get pseudonormalized with high RVDP/ RAP Haddad F et al. Circulation 2008;117:1436-1448 Tei C, et al: J Am Soc Echocardiogr. 1996; 9: 838-847 RV FAC (Fractional Area Change) / Apex-forming RV RV FAC%= 100x RVarea diastole – RVareasystole / Rvareadiastole 27.2 - 21.7 / 27.2 = 20% 43 Dp/dt Rate of rise of LV or RV pressure Normal dp/dt> 400 mm Hg/sec Role of ECHO in Therapy, Longitudinal F/U and Prognosis Prognostic Parameters and Determinants of Risk in PAH LOWER RISK DETERMINANTS OF RISK HIGHER RISK No Clinical evidence of RV failure Yes Gradual Progression of symptoms Rapid II, III WHO class IV Longer (>400 m) 6MWD Shorter (<300 m) Peak VO2>10.4 mL/kg/min CPET Peak VO2<10.4 mL/kg/min Echocardiography Pericardial effusion, significant RV enlargement/dysfunction; RA enlargement Minimal RV dysfunction (TAPSE in ESC guidelines) RAP <10 mm Hg; CI >2.5 L/min/m2 Hemodynamics RAP >20 mm Hg; CI <2.0 L/min/m2 Minimally elevated BNP Significantly elevated Syncope is poor prognostic sign added in the ESC guidelines McLaughlin VV et al. J Am CollCardiol. 2009;53:1573-1619. 46 Prognostic Value of Echo Parameters of RV Function • 47 pts with PAH •2-year survival = 88 % if TAPSE > 18 mm • 2-year survival = 50 % if TAPSE < 18 mm •Forfia PR – Am J RespirCrit Care Med 2006; 174: 103441 Prognostic Value of MPI YeoTc – Am J Cardiol 1998; 81:1157-61 Tei, C- JASE 1996; 9: 838-47 Prognostic Value of MPI Meluzin J – Eur J Echocardiogr 2003; 4: 267-71 Van Wolferen, SA et al. Eur Heart J (2007) 28, 1250–1257 Kaplan-Meier Survival Curves for Echocardiographic Predictors of Outcomes 81 pts prostacyclinevs placebo F/U 36 months, 20 deaths, 21 transplantations Raymond, R. J. et al. J Am CollCardiol 2002;39:1214-1219 Right atrial area > 20 cm2, abnormal; > 27 cm2 associated with poor prognosis Eccentricity index > 1 abnormal; > 1.7 carries poor prognosis Suggested Assessments and Timing for Follow-ups in patients with PAH: ESC Guidelines Role of Echo in Determination of PH Group Determining PH Type on Basis of ECHO • Caution is needed in distinguishing PAH from PH related to diastolic abnormalities solely on the basis of ECHO • Features of “diastolic dysfunction”, e.g., delayed relaxation pattern and reduced e’ (mitral annular tissue velocities), may occur in PAH ( secondary to bad RV) • Pulmonary vascular resistance (PVR) calculations by ECHO do not take into account left atrial pressurethey do not distinguish PAH from PVH. Left-sided vs. Right-sided Origin of Pulmonary Hypertension Left-Sided Origin of PH Right-Sided Origin of PH 2-D Echocardiographic Findings: LVH, LAE Variable LV function Normal RV size No interventricular septal bowing Normal LV size, normal LA size Normal LV function RV dilation (ratio of RV:LV size >1) Right to left interventricularseptal bowing Atrial septum neutral or bowed to right Atrial septum bowed to left Normal or mildly reduced RV function Mild to severe RV dysfunction No pericardial effusion Mild to moderate pericardial effusion Doppler Findings: ≥2+ mitral valve disease (MR or MS) Minimal or no MR or MS Grade II or III diastolic dysfunction Normal diastolic function or grade I diastolic dysfunction (E:A reversal) Variable TR Absence of notched pattern in Doppler signal obtained from RVOT Variable TR (TR severity > MR severity) Notched Doppler signal in RVOT Variable PASP (typically <70 mm Hg) Variable PASP (typically ≥70 mm Hg) 52 EchocardiographicParameters for the Assessment of Pulmonary Hypertension/ Right Ventricle • Size and surface areas of both atria. • Bi-ventricular size and systolic /diastolic function (RV), presence of RVH, CMY, any valvular abnormality (MS, MR, AS etc..), pericardial effusion or intracardiacshunt: – Subjective “eyeball” assessment of RV function ( good vs mild, moderate or severe RV dysfunction) – Percent Fractional Area Change (% FAC) – Tricuspid Annular Plane Systolic Excursion (TAPSE) – Eccentricity Index / D-shaping of the IVS – RV Myocardial Performance Index (MPI) or Tei index – TDI systolic velocity of the RV lateral annulus (S’), (and short IVRT on RV TDI) • Pulmonary artery pressure estimation / Hemodynamics: – Pulmonary Artery Acceleration Time (PAAT) and presence/ timing of Notching – Pulmonary artery pressures (Systolic, Diastolic, Mean) , Resistance and Capacitance • RA pressure ( IVC size and collapse) • Assessment of C.O ( LVOTdiameter and time-velocity integral of aortic flow by PW Doppler) • Bubble study (CHD, PFO) • 3D echocardiography, myocardial deformation techniques (strain imaging or Role of ECHO in PH: Summary ECHO is an essential tool and plays a key role the initial and subsequent evaluation of a patient with PH. Despite its limitations, it remains the most clinically useful nonivasive test for the assessment of the pulmonary circulation ECHO Provides a reasonably accurate estimate of the RV / PA pressures and hemodynamics . The prognostic value of the echocardiographic parameters discussed here are well established, and the regular assessment of these, as part of a goal-oriented therapy, is critical to monitor the progression of PH and the response of patients to PAH specific therapy, independent of clinical and RHC data Acknowledgements Lauren Skinner, RDCS: Preparation and acquisition of many of the slides Sonographers RDCS: • • • • Yvonne Golomb Liliana (Lily) Miranda Carol Mortier Yousef Kohen Partners – – – – – – – Jon Kobashigawa, M.D Jaime Moriguchi, M.D Michele Hamilton, M.D Jignesh Patel, M.D BabakAzarbal, M.D Michelle Kittleson, M.D David Chang, M.D THANK YOU Any questions?