A2 Developing and Deploying HRH
advertisement

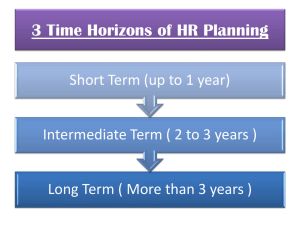
Reforming the Health Work Force to support Universal Health coverage in Africa. Dr Patrick KADAMA Executive Director of the Platform on Human Resources for Health at the African Centre for Global Health and Social Transformation (ACHEST) Presentation Outline • PHC experience & the emerging concerns with Inequality in health outcomes • The case for new direction & HRH Challenges • Need for New thinking and effort • Competency Based Education • Way forward From WHR 2008 - PHC Now More than Ever UHC – the means to manage Concerns with INEQUALITIES The world health report 2008 identified as one the four broad policy directions for renewal of primary health care the need to Deal with HEALTH INEQUALITIES by moving towards UNIVERSAL COVERAGE in three aspects at the very minimum: 1. Extend of health-care networks (INFRASTRUCTURE) to where they are not available; a) Implications for reform of HRH policies b) c) Implications for Health Infrastructure Implications for essential medical products, commodities and a supply chain 2. Shift from reliance on user fees levied on the sick to the solidarity and protection provided by pooling and prepayment; a) Implications for reform of Health Financing Mechanisms 3. Develop of mechanisms of social health protection. a) Implications for Governance to contribute to cross-sectoral development of policy for Social Security (?pensions / terminal benefits for employees as well as child and unemployment support for indigents). Human Resources for Health require Reform (WHR 2000) Why New Directions? • Global shortage: 4.3m,African shortage 1m. • Globalized connected world with inequities • Tensions: Health Professionals vs Population expectations: vocation or jobs, distribution, commercialization, working environment • Changing scope of practice; unmet skills needs: Nurse Practitioners, Task Shifting, Needs based training etc Education: Critical Solution • Underlying global HWF crisis is failure to train and retain enough • Education Institutions are factories: good factory = good product; bad factory = bad product • Sub Saharan African Medical Schools Study: faculty shortages, infrastructure, private sector Environment in Africa • Large population • Limited resources • Human Resource shortages Population Physician workforce • Big Disease burden www.worldmappers.org Disease Burden HS definition African HWF spectrum Contributing factors: •Good governance, law and order •Gender •Social justice •Social and economic development Nat'l referral Regional referral General Practitioners Mid-level Sub-district level Household & community CHWs SHARED District level Super-specialists Specialists 11 AU Health Strategy & WHO Road Map Focus not only on numbers but on skill mix and quality • Determine the categories of professional, auxiliary (mid-level) and community health workers that will provide an appropriate human resource mix for their needs. • Develop costed national human resources development and deployment plans, including revised packages and incentives, especially for working in disadvantaged areas. • Fund the establishment of the training capacity required to produce the desired number of health workers. • Build multi-purpose trained staff as the nucleus of health care delivery. Scale-up framework INDICATOR: MDGs GOAL: HEALTH OUTCOMES Integrated Health Service Delivery Networks PRIORITIZED SKILL MIX "CLOSE-TO-CLIENT HEALTH TEAMS" Defined within country context EXISTING CAPACITY TECHNICAL - Training - Institutions - Infrastructure - Connectivity - Partnerships DEVELOPMENT OF NEW CAPACITIES POLITICAL - Supportive environment - Leadership - Commitment - Legislation - Policy - Partnerships FINANCIAL - Resources - Incentives - Partnerships 13 Critical success factors for scaling up Study of GHWA Task Force on Education and Training • 9 country experiences across regions Critical factors identified: • Political commitment and good governance – Sustained high level support, 'one' country-led health plan, significant financial investment • Enabling environment – Multi-sector participation, Good information systems, effective management and leadership, labour market capacity and policy • Workforce planning – Plan long term, act short-term and update regularly, commitment to production / appropriate skill mix integrated teams, needs based, expansion of pre-service programmes New directions Needs Based Education Competency/ Outcome Based Education Key issues with the Health Work Force to meet needs 1. 2. 3. 4. 5. 6. Mismatch of competencies to needs Weak teamwork Gender stratification Hospital dominance over primary care Labour market imbalances Weak leadership for health system performance Summarized from the report on the Health Work Force for the 21st Century Evolution of Medical Education reforms from the report on the Health Work Force for the 21st Century Moving toward a Health Work Force Fit-for Purpose What is fit for purpose: • good enough to do the job for which it was designed • Possess attributes required to achieve intended objective • Experts, Professionals, Leaders What FFP is Not • • • • Low quality HWF for the poor only HWF with restricted market Origins of FFP HWF: Africa first missionaries FFP HWF: UK (Surgeons); USA surgical technicians Competency Based Education • Education aimed at imparting underlying characteristics related to job performance • Encompasses knowledge, traits, skills and abilities. • Fit for Purpose Required Competencies • Prepared to work where services are most needed. • Able to respond to health needs of community. • Able to deliver quality care with available (limited) resources. • Able to be leaders and change agents • Continuous self directed learners • Effective communicators Achieving Competencies • Selection process for candidates • Right attitudes, belong to community (underserved areas) • Training in real life practice environment • Mentorship • Team Based Learning • Strong linkages with communities Kampala Declaration and Agenda for Global Action • Key elements: – Building coherent national and global leadership for health workforce solutions – Ensuring capacity for an informed response based on evidence and joint learning – Scaling up health worker education and training with needs based skill mix – Retaining an effective, responsive and equitably distributed health workforce – Managing the pressures of the international health workforce market and its impact on migration – Securing additional and more productive investment in the health workforce 23 Implications for Countries • • • • Prioritize Education and Training of HWF Link with National Development Plans Plan long term, act short and review frequently Link E &T to Population health needs & health systems • Create Country Multi-stakeholder Alliances (CCF) • Establish HWF Information Systems (Observatories)