File - Mayo Clinic Center for Tuberculosis
advertisement
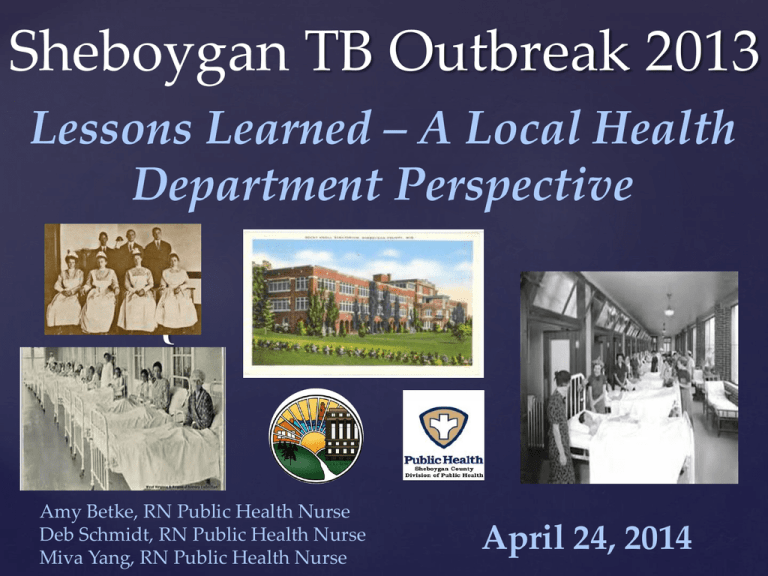
Sheboygan TB Outbreak 2013
Lessons Learned – A Local Health
Department Perspective
{
Amy Betke, RN Public Health Nurse
Deb Schmidt, RN Public Health Nurse
Miva Yang, RN Public Health Nurse
April 24, 2014
Disclosures
None
PRESENTATION OBJECTIVES
Overview of index case
and outline of outbreak
events
Lessons Learned –
Sheboygan
County Public
Health
Department
Perspective
Lessons Learned –
TB Nurse Case
Management
Strike Team
Perspective
TIMELINE OF INDEX CASE
Completed 6 months
INH - Sheboygan
Immigrated to
USA from Laos
(1 child, no husband)
TST 13mm
March 2012
Visited family for 1 month
in Thailand
Again offered
INH 7x.
Moved
to
Alaska
2013
2012
2011
2010
2009
2008
2007
First sign
of cough
2006
2005
2004
2003
2002
2001
2000
No recall of prior
TB treatment.
Offered Rifampin
or INH, but
became pregnant
1999
1998
1997
1996
1994
Prior to
1994
1995
September –
Moved to
Sheboygan
Took 6 weeks
of INH then
pregnant
Camp Ban
Vinai,
Thailand
Had 2
children
October 2012
Moved to
Sheboygan
continues with
cough
TIMELINE OF INDEX CASE
January 4
October 1
Moved back to Sheboygan
2
0
1
2
October 23
Dx with Pneumonia-ED
November
Flight to Las Vegas
December 4
Dx with Pneumonia-ED
December 20
Dx bronchitis and treated for
reflux-Office
CXR interpreted as no active TB disease
2
0
1
3
February
ED X2
February 22
Dx with asthma by a
pulmonologist
February 25 - March
Wausau
April 3
Went to clinic for depression, provider
ordered CXR, cavitary lesions observed
April 11
Dx with TB
OUTLINE OF EVENTS
April 11, 2013 - The Division of Public Health was notified of a
patient with suspected TB. Patient has several children.
April 15, 2013- Labs confirm this patient has active tuberculosis.
She was started on Rifampin, INH, Pyrazinamide, Ethambutol,
and Moxifloxacin.
April 16, 2013- Investigation of family: One child is coughing.
Three children have abnormal chest x-rays. Suspect with TB in
these 3 children. Children are excluded from 2 different schools.
April 17, 2013- INH resistant detected and INH stopped.
OUTLINE OF EVENTS
April 22, 2013- One more school child living outside the home is
identified and found to have an abnormal chest x-ray.
April 23, 2013- Total of 5 individuals Dx with active TB. Incident
Command System (ICS) activated. Contact investigation continues.
April 24-26, 2013- Meeting with SASD Administration to develop
joint plan.
April - May 2013- Targeted testing was completed at 2 local schools.
May 7, 2013- MDR TB Dx in Index Case. Resistant to both INH and
Rifampin. Patient hospitalized and started on Ethambutol,
Pyrazinamide, Moxifloxacin, Linezolid, Amikacin, and Ethionamide.
Sister’s
Parents
Patient
A’s House
1 active
2 infected
4 active
8 infected
9 kids
A
8 kids
{
Adult Child
1 infected
Niece’s
1 active
3 infected
OUTLINE
OF EVENTS
May 7-10, 2013- Centers for Disease Control, Mayo
Clinic, State TB Program, Sheboygan Area School
District Staff, Children’s Hospital and local Medical
Providers conferenced with Public Health on the
treatment and contact investigation recommendations.
Incident Command is expanded.
OUTLINE OF EVENTS
May 20, 2013- Conference call with state legislators,
seeking appropriations from Joint Finance
Committee (JFC).
June 3, 2013- Governor Walker and Department of
Health Services issue a press release in support of
funding the TB outbreak.
June 4, 2013- JFC approved 4.6 million for
submission in the State biennial budget.
OUTLINE OF EVENTS
June 7, 2013- The CDC Epi-Aid team reported on the investigation, felt
containment was met.
June 11, 2013- Index Case transferred from hospital to Rocky Knoll Health
Care Facility negative-pressure room with no visitation. Final drug
susceptibility tests show only Index case with MDR; other 7 cases INH
resistant only.
June 26, 2013- Index Case returns to private single-family home in Sheboygan.
Client remained in isolation. County purchasing agent secured home, as a
rental property and obtained furnishing/necessary household items.
August 2013- Another school age child (Index case’s nephew) Dx with active
TB. Case count at 10, child had LTBI and progressed to active TB. An
additional active case was detected in Marathon County as well as, 4 new
LTBI contacts.
Outline of Events
Fall, 2013 – School begins. LHD receives school
assistance with DOT for students and faculty affected
by outbreak. Another round of school testing is
completed.
October 17, 2013- Index case released from isolation
following 27 weeks spent in hospital, LTCF and rental
property. Able to reunite with children.
November 2013 – TB work continues. Incident
Command modified as contact investigation wraps up
and individuals are beginning to complete directly
observed therapy for active as well as latent TB.
Lessons LearnedOur Agency Perspective
One Year Later…
What Have We Learned?
Greatest Assets During Outbreak
Dedicated Staff and Community Healthcare Partners
Staff Members Including PHN’s, Support Staff, HHS Interpreter with
strong TB knowledge including previous experience with MDR TB
Staff members willing to learn and do
Previous Emergency Preparedness Training
Compliance of the majority of clients with prescribed TB treatment
Strike Team Case Management
One Year Later…
What Have We Learned?
Greatest Assets During Outbreak (cont.)
Interdisciplinary Team
DOT Workers
Collaboration with SASD for DOT
Interdisciplinary Meeting with ASMMC.
Rocky Knoll Health Care Facility
Strong Support of Elected Officials and Leadership
Local Capacity Was Exceeded
Early in Outbreak
Staff Assigned
to Assist
Request Mutual
Aid and Obtain
Approval to
Hire Limited Term
Employees
Logistical Lessons
Technology – Expand cell phones with texting
availability and dictation use
Streamline and centralize medication supply –
Two person team to manage medication refills and
bubble packing.
Use of Communication Logs for DOT workers
Bring in support staff to act as runners, DOT
workers, etc.
Development of Communication Cards
Card for Clinic Use
INTERDISCIPLINARY
TEAM FORMATION
Complex needs of the family-financial, mental health,
family dynamics, and school-related issues.
TB NURSE
CASE MANAGEMENT
STRIKE TEAM PERSPECTIVE
Amy, Deb, Miva, Mai Kou pic
Additional Strike Teams
DPH Sub Teams
Medication Monitoring Team
DOT Team
Business/School Investigation Team
Cultural CompetencyLessons Learned
Assign Hmong Nurse and
Support Staff as part of the
Strike Team from the start
Consider the gender and
age of the interpreter
Education with the index
case as to the importance of
naming close contacts was a
priority
Cultural CompetencyLessons Learned
Involve family into the
treatment plan decisions
Importance of nutritional
needs/ethnic food
preference
Birth control and its
challenges in relation to
TB treatment
Tips for Providing Culturally
Competent Tuberculosis
Services to Hmong Persons
Tips for Providing Culturally
Competent Tuberculosis
Services to Hmong Persons
Interactions with Hmong clients and Family Members
Avoid speaking loudly
Avoid making direct eye contact
Avoid outwardly complimenting Hmong children
Avoid refusing refreshments that may be offered at a Hmong client’s
home
Be aware that a Hmong client may present with unusual physical
markings as well as wearing red cloth necklace or bracelets
Be sure to ask clients about their understanding of their illness and its
cause
Tips for Providing Culturally
Competent Tuberculosis
Services to Hmong Persons
Family and Cultural Issues
Before making a decision, family members are consulted
Mental Health (Worries)
Hmong may be ashamed or avoid discussion of mental health issues
Social Stigma
TB is often a cause for shame among the Hmong
Active TB vs. LTBI
Tips for Providing Culturally
Competent Tuberculosis
Services to Hmong Persons
Tuberculosis Diagnosis and Treatment
Hmong language lacks words for many medical terms
Hmong may delay or avoid seeking care
Deliver clear, consistent messages
Two-way communication and equal exchange between provider, client,
and family
Summary
References
http://www.cdc.gov/tb/publications/guidestoolkits/EthnographicGuides/
Hmong/chapters/tips.pdf Promoting Cultural Sensitivity: A
Practical Guide for Tuberculosis Programs That Provide Services
to Persons from Somalia
Francis J. Curry National Tuberculosis Center and California
Department of Public Health (2008). Drug-Resistant
Tuberculosis A Survival Guide for Clinicians, Second edition
Any Questions?