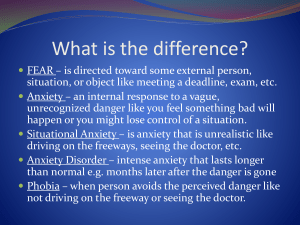
The Anxiety Disorders Some Practical Questions & Answers
advertisement
Social Phobia A Patient-Centered, Evidence-Based Diagnostic and Treatment Process A Presentation for the Students of Ohio University Heritage College of Osteopathic Medicine Kendall L. Stewart, MD, MBA, DFAPA November 29, 2011 Why is this important?1 • • • • • • • The 12-month prevalence rate of Social Anxiety Disorder (SAD) is – 6.6% for males and – 9.1% for females. People with this disorder have a persistent and admittedly irrational fear of performing in social situations. They are convinced that they will perform poorly and be humiliated as a result. Their fears may be specific2 or generalized. These patients experience anticipatory anxiety and/or panic attacks. Avoidance is a common complication. Impairment results.3 1Goldman, • After mastering the information in this presentation, you will be able to – Describe how patients with Social Anxiety Disorder often present, – Detail the diagnostic criteria, – Describe some of the associated features, – List some differential diagnoses, – Write a preliminary treatment plan, and – Identify some of the frequent treatment challenges. • This disorder is also called Social Phobia. 2008 most common fear is the fear of public speaking. 3The wages of a person with SAD are 14% lower than those without the disorder. 2The How might a patient with Social Anxiety Disorder present?1 • This is a 22-year-old medical student. • “I’m thinking of dropping out of medical school.” • “I simply cannot give an oral presentation.” • “I was always able to get out of giving speeches in high school and college.” • “I would have no problem with writing a paper, but the idea of speaking in front of a group is unbearable.” • “When I’ve tried to do it before, I’ve experienced panic and had to leave the room.” 1Goldman, 2008 2People—particularly 3Even • “Just thinking about having to do it makes gives me palpitations and triggers diaphoresis.” • “I can’t sleep and I can’t concentrate on my studies.” • “If you can’t make an exception, I will have to drop out of school.” • “My father dropped out of law school for the same reason.” • “I hate being this way.”2,3 men—are often deeply ashamed of symptoms of depression and anxiety. accepting treatment may be too much to bear. A patient refused to take antidepressants and died. What are the diagnostic criteria for Social Phobia? • • • • • The person experiences excessive and persistent fear of one or more social performance situations. He or she experiences feelings of anxiety, fear or panic immediately upon encountering the feared social situation. The person recognizes that the fear is excessive, unreasonable or out of proportion to the actual risk in the situation. The patient tends to avoid the feared social situation, or if he or she does not avoid it, the situation is endured with intense anxiety or discomfort. The patient’s symptoms of anxiety and avoidance behavior cause significant distress or impairment. • • The problem must be present for at least six months in children under 18. The symptoms of anxiety are not caused by – – – • • • A medical condition or Substance abuse. If the patient has another medical condition with visible symptoms such as stuttering, the fear must not be only of others noticing these medical symptoms. If the individual fears most social situations, the SP is viewed as generalized. SP can occur in very specific social situations too. You can watch a sufferer’s description here. What do people with Social Anxiety Disorder fear and avoid?1 • Performance Situations • Social Interaction Situations – Public speaking – Talking in meetings or classes – Participating in sports or working out in front of others – Performing music or acting on stage – Writing in front of others – Eating or drinking in front of others – Using public restrooms while others are nearby – Making mistakes in front of others1 – Being in public areas such as a shopping mall or in a bus 1Suffering public humiliation is no fun. I once teed off first in Augusta. – Going to parties – Having a conversation with others – Talking to strangers – Inviting friends over for dinner – Talking on the phone – Expressing personal opinions – Asserting oneself – Being in intimate situations – Talking to authority figures – Returning items to a store – Sending food back in a restaurant What associated features might you see?1 • • • • • • • • • • • • Excessive sensitivity to criticism Problems with appropriate assertiveness Low self-esteem Feelings of worthlessness Test anxiety Inept social interactions Poor work history Social introversion Suicidal thought Epidemiological studies suggest the disorder is more common in women, but males are more common in most clinical samples Typical onset in teens Course is typically fluctuating but lifelong 1DSM-IV-TR, 2Be • Physical manifestations of anxiety – – – – – • • • Academic underachievement Inadequate social support Comorbid psychiatric disorders – – – – – • Tremulousness Shaky voice Cold, clammy hands Sweating Dilated pupils Other anxiety disorders2 Mood disorders Substance-related disorders Eating disorders Personality disorders More frequent among first-degree biologic relatives 2000 sure to look for Generalized Anxiety Disorder. What is the most frequently-missed lesion on a medical image? What other diagnoses might you include in the differential diagnosis?1 • • • • Panic Disorder with Agoraphobia usually begins with an unexpected panic attack and continues with subsequent avoidant behavior not limited to social situations. People with Agoraphobia typically prefer to be with a trusted companion. Children with Separation Anxiety Disorder resist being separated from their caretaker, but they are usually comfortable in social situations when the caretaker is present.2 While fear of embarrassment or humiliation may accompany Generalized Anxiety Disorder or Specific Phobia, these are not the principal foci of the patient’s dread. 1DSM-IV-TR, 2Martha • • • • • • In Pervasive Developmental Disorder and Schizoid Personality Disorder social situations are avoided because of a profound lack of interest in social interaction. Avoidant Personality Disorder probably overlaps with SAD, Generalized Type. Social anxiety in a symptom is many other mental disorders, but it is not the principal symptom in these cases. Of course, anxiety frequently accompanies a variety of general medical disorders. Substance-Use Disorders also cause anxiety. Performance anxiety, stage fright, and shyness should not be diagnosed as SAD unless clinically significant impairment or marked distress results. 2000 McCranie told of taking a child to get a cola and losing money in the machine. What might a typical treatment plan look like?1 • Anticipatory Anxiety – Predict it – Consider medication options that follow • Panic Attacks – Consider short-term clonazepam 1mg twice per day initially and taper slowly as antidepressant kicks in. – Begin paroxetine 10-20mg twice per day • Avoidance Behavior – Real exposure therapy – Imagined exposure therapy – Gradual and repetitive confrontation of feared situations2 1DSM-IV-TR, • Generalized Anxiety – Buspirone 15mg twice per day – Most SSRIs are helpful • Maladaptive attitudes and behaviors – Cognitive behavioral psychotherapy • Education and Support – Refer to appropriate Internet sites – Provide citations – With consent, refer to other sufferers3 – Consider referral to self-help groups 2000 continuous exposure, mastery is quickly lost. 3Referrals to other patients doesn’t always work out well. “That woman is crazy, Doc!” 2Without What are some of the treatment challenges you can expect? • • • • • • • • • 1A 2A Noncompliance is always the principal challenge. Lack of motivation is often an issue. Acceptance of disability limits further progress. Excessive sensitivity to medication side effects frequently complicates treatment. These patients often have a variety of comorbid medical and psychiatric conditions Unrealistic expectations for a quick and permanent cure limit the patient’s ability to adopt a chronic disease management philosophy and practice. People with anxiety sometimes remain convinced that something “physical” is wrong and remains undiscovered. These patients can be very sensitive to your perceived rejection.1 These miserable people demand a lot of attention and easily morph into dependent, clinging emotional black holes. It is critical not to promise more than you can deliver.2 patient misinterpreted my sigh. Another patient suspected the Lysol© was intended for her. colleague of mine agreed to call a patient at 10 PM every day. I had to manage the case when he left. Where can you learn more? • • • • • • • • • • American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision, 2000 Sadock, B. J. and Sadock V. A., Concise Textbook of Clinical Psychiatry, Third Edition, 2008 Stern, et. al., Massachusetts General Hospital Comprehensive Clinical Psychiatry, 2008. You can read this text online here. Flaherty, AH, and Rost, NS, The Massachusetts Handbook of Neurology, April 2007 Stead, L, Stead, SM and Kaufman, M, First Aid© for the Psychiatry Clerkship, Second Edition, March 2005 Klamen, D, and Pan, P, Psychiatry Pre Test Self-Assessment and Review, Twelfth Edition, March 20093 Oransky, I, and Blitzstein, S, Lange Q&A: Psychiatry, March 2007 Ratey, JJ, Spark: The Revolutionary New Science of Exercise and the Brain, January 2008 Medina, John, Brain Rules: 12 Principles for Surviving and Thriving at Home, Work and School, February 2008 Stewart KL, “Dealing With Anxiety: A Practical Approach to Nervous Patients,” 2000 Where can you find evidence-based information about mental disorders? • • • • • • • Explore the site maintained by the organization where evidence-based medicine began at McMaster University here. Sign up for the Medscape Best Evidence Newsletters in the specialties of your choice here. Subscribe to Evidence-Based Mental Health and search a database at the National Registry of Evidence-Based Programs and Practices maintained by the Substance Abuse and Mental Health Services Administration here. Explore a limited but useful database of mental health practices that have been "blessed" as evidence-based by various academic, administrative and advocacy groups collected by the Iowa Consortium for Mental Health here. Download this presentation and related presentations and white papers at www.KendallLStewartMD.com. Learn more about Southern Ohio Medical Center and the job opportunities there at www.SOMC.org. Review the exceptional medical education training opportunities at Southern Ohio Medical Center here. How can you contact me?1 Kendall L. Stewart, M.D. VPMA and Chief Medical Officer Southern Ohio Medical Center Chairman & CEO The SOMC Medical Care Foundation, Inc. 1805 27th Street Waller Building Suite B01 Portsmouth, Ohio 45662 740.356.8153 StewartK@somc.org KendallLStewartMD@yahoo.com www.somc.org www.KendallLStewartMD.com 1Speaking and consultation fees benefit the SOMC Endowment Fund. Are there other questions? John Gilbert, DO OUCOM 1989 Kevin Kammler, DO OUCOM 1993 Safety Quality Service Relationships Performance