Anxiety Sans OCD - Turnaroundanxiety.com
advertisement
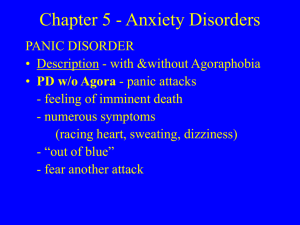
SA01 Understanding and Treating Anxiety Disorders Dr. David A Russ Licensed Psychologist www.turnaroundanxiety.com www.carolinas-counseling.com Notes and Powerpoint can be downloaded from: www.turnaroundanxiety.com/documents 1. 2. 3. 4. 5. Identifying the Core Elements of Anxiety Types of Anxiety Disorders Explanation of Treatment Example of Treatment Question and Answer Outline for this Workshop 1. 2. 3. 4. 5. False Alarm Anxiety Sensitivity Rapid and General Memorized/Learned Normal problem solving backfires Core Elements (Causes) Disorder - Reaction significantly incongruent with circumstances 1. 2. 3. 4. Intensity Frequency Interference Persistence What Makes it a Disorder? Panic OCD GAD Phobia Shared Elements 1. 2. 3. 4. Physiological Arousal Cognitive Distortion Avoidant Coping Reinforcing Cycle Specific Shared Elements Autonomic Nervous System Sympathetic and Parasympathetic big issue, often becomes part of disorder Can be triggered by event, multiple stressors, biology, etc Fight or Flight trumps everything Real Experience + Imagined Fear Loss of predictability Physiological Arousal Physiology “demands” focus on danger Problem is mental invention (What if?) Common Distortions Over-estimate danger Feel over-responsible - guilt All or nothing Filter out positive Intolerance of uncertainty Mind-Reading Cognitive Distortions Attempt to solve “invented” problem 1. Primary: Avoidance/Escape – literal or imagined 2. Secondary: If can’t avoid then make it as safe as possible – symptoms get more extreme and less functional – partially effective (huge problem) Avoidant Coping Trigger Primary Secondary Getting a shot don’t go distract self, don’t look at needle, request extra anesthesia Racing heart Don’t exert self Check pulse, have safe person with you, relaxation Food that could cause choking Don’t eat Have water, chew extra, eat soft food Interacting with people Avoid social situations Keep topic easy, avoid eye contact, take talkative friend, have excuse to leave Examples Trigger No Correction View as Threat Avoidant Coping Anxiety Reinforcing Cycle 1. 2. 3. 4. 5. 6. 7. Panic Separation GAD Social/Selective Mutism Phobias Trauma OCD and spectrum Types of Anxiety Fear of Fear • • • • Severe Distress Out of blue Fear of fear Agorophobia Panic Disorder palpitations sweating trembling or shaking sensations of shortness of breath or smothering feeling of choking chest pain or discomfort nausea or abdominal distress dizziness or lightheadedness derealization or depersonalization fear of losing control or “going crazy" fear of dying paresthesias chills or hot flushes Symptoms Fear of loss of protection/security • • • • • Characterized by extreme fear/distress when faced with separation - home or attached adults Worry about safety of self and caregivers School refusal Body complaints Being alone/sleep Separation Anxiety Fear of things going bad • • • • Pattern of exaggerated worry that is characterized by attention to negative or threat related information Must last 3 -6 months About multiple issues Physical complaints: pain, nausea, fatigue Generalized Anxiety Disorder Fear of embarrassment or judgment • • • • • Fear acting in way that is humiliating Fear of judgment Fear reaction can be panic Performance Anxiety Selective Mutism Social Phobia Fear of clearly discernible object or situation. Types • • • • • Phobias Natural Animal Blood/Shots/Injury Situational Other - Emetophobia Anxiety resulting from Trauma • • • • • Physical or Natural Re-experienced (flashbacks, dreams, etc. Avoidance Numbing Hyper-arousal Trauma related Fear of loss of core value • • Obsessions – thoughts in focus in spite of and contrary to desire of person. Thoughts cannot be suppressed even though not characteristic of self. Great distress as result Compulsions – urges to perform behavior or thinking actions to reduce anxiety or possible harm. Obsessive-Compulsive Disorder • Treatment for Core Elements: 1. 2. 3. • Physiological Arousal Calming Cognitive Distortion Accuracy Avoidant Courageous Coping Core error: Reacting to something that is bothersome as dangerous Treatment • • • • • Educational Directive Structured Symptom Reduction rather than insight oriented More coach, less therapist Approach • • • • Medication Skill Training – somatic management Distress tolerance Change Lifestyle Physiological Calming • • • • Teach thinking about thinking Tracking thoughts Identification of problem thinking Cognitive Restructuring Cognitive Accuracy 1. 2. 3. 4. What is the evidence? Are there other ways to think about the situation? What is the worst that could happen? What is the effect of believing idea? Keys to Disputing Thoughts ERP • Exposure • • • Deliberately evoking anxiety Remaining in distress Response Prevention • • • Prevent normal coping response Not doing anything to reduce distress before, during and after exposure Don’t employ Safety Behaviors Courageous Coping Exposure • Types • • • • • Thought Interoceptive Virtual In situation Create Hierarchy • • • • SUDs List of triggers and core fears Put in 3 categories - Easy, Medium, Hard Create an exposure for them Treatment - Exposure 1.Words 2.Short sentences 3.Paragraphs 4.Simple cartoon illustrations 5.Photos of sick people (no vomit) 6.Pictures of vomit 7.Pictures of people vomiting 8.Animated videos of vomit 9.Videos of people vomiting 10.Fake vomit and smell Emetophobia Hierarchy Safety Behavior Response Prevention Don’t look at words Stare at words, write the word Only do exposure with safe person or Exposure in places where might get in safe place sick (nurses office) Mental change to make story safe (just Describe story as scary as possible looking for something in toilet) Say words fast or mutter them Slow down speaking, enunciate Subtle actions (flick, spit, swallow, change posture) No flicking, fidgeting, spitting Example Response Prevention Turnaround www.turnaroundanxiety.com