(SBI) in and Employee Assistance Program
advertisement
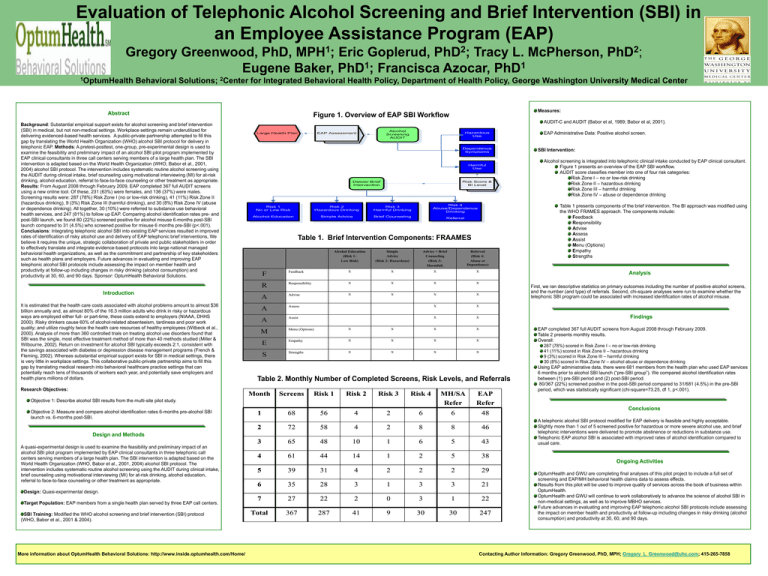
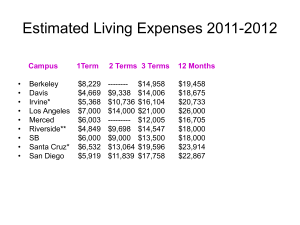
Evaluation of Telephonic Alcohol Screening and Brief Intervention (SBI) in an Employee Assistance Program (EAP) 1 MPH ; 2 PhD ; Gregory Greenwood, PhD, Eric Goplerud, Tracy L. McPherson, 1 1 Eugene Baker, PhD ; Francisca Azocar, PhD 1OptumHealth 2 PhD ; Behavioral Solutions; 2Center for Integrated Behavioral Health Policy, Department of Health Policy, George Washington University Medical Center Abstract Background: Substantial empirical support exists for alcohol screening and brief intervention (SBI) in medical, but not non-medical settings. Workplace settings remain underutilized for delivering evidenced-based health services. A public-private partnership attempted to fill this gap by translating the World Health Organization (WHO) alcohol SBI protocol for delivery in telephonic EAP. Methods: A pretest-posttest, one-group, pre-experimental design is used to examine the feasibility and preliminary impact of an alcohol SBI pilot program implemented by EAP clinical consultants in three call centers serving members of a large health plan. The SBI intervention is adapted based on the World Health Organization (WHO, Babor et al., 2001, 2004) alcohol SBI protocol. The intervention includes systematic routine alcohol screening using the AUDIT during clinical intake, brief counseling using motivational interviewing (MI) for at-risk drinking, alcohol education, referral to face-to-face counseling or other treatment as appropriate. Results: From August 2008 through February 2009, EAP completed 367 full AUDIT screens using a new online tool. Of these, 231 (63%) were females, and 136 (37%) were males. Screening results were: 287 (78%) Risk Zone I (no or low-risk drinking), 41 (11%) Risk Zone II (hazardous drinking), 9 (3%) Risk Zone III (harmful drinking), and 30 (8%) Risk Zone IV (abuse or dependence drinking). All together, 30 (10%) were referred to substance use behavioral health services, and 247 (81%) to follow up EAP. Comparing alcohol identification rates pre- and post-SBI launch, we found 80 (22%) screened positive for alcohol misuse 6-months post-SBI launch compared to 31 (4.5%) who screened positive for misuse 6 months pre-SBI (p<.001). Conclusions: Integrating telephonic alcohol SBI into existing EAP services resulted in improved rates of identification of risky alcohol use and delivery of EAP telephonic brief interventions, We believe it requires the unique, strategic collaboration of private and public stakeholders in order to effectively translate and integrate evidence-based protocols into large national managed behavioral health organizations, as well as the commitment and partnership of key stakeholders such as health plans and employers. Future advances in evaluating and improving EAP telephonic alcohol SBI protocols include assessing the impact on member health and productivity at follow-up including changes in risky drinking (alcohol consumption) and productivity at 30, 60, and 90 days. Sponsor: OptumHealth Behavioral Solutions. Figure 1. Overview of EAP SBI Workflow AUDIT-C and AUDIT (Babor et al, 1989; Babor et al, 2001). Large Health Plan Research Objectives: Alcohol Screening AUDIT EAP Assessment Hazardous Use Dependence Symptoms Harmful Use Risk Score & BI Level Deliver Brief Intervention Risk 1 No or Low Risk Risk 2 Hazardous Drinking Risk 3 Harmful Drinking Alcohol Education Simple Advice Brief Counseling Risk 4 Abuse/Dependence Drinking Referral Table 1. Brief Intervention Components: FRAAMES Introduction It is estimated that the health care costs associated with alcohol problems amount to almost $36 billion annually and, as almost 80% of the 16.3 million adults who drink in risky or hazardous ways are employed either full- or part-time, these costs extend to employers (NIAAA, DHHS 2000). Risky drinkers cause 60% of alcohol-related absenteeism, tardiness and poor work quality; and utilize roughly twice the health care resources of healthy employees (Witbeck et al., 2000). Analysis of more than 360 controlled trials on treating alcohol use disorders found that SBI was the single, most effective treatment method of more than 40 methods studied (Miller & Wilbourne, 2002). Return on investment for alcohol SBI typically exceeds 2:1, consistent with the savings associated with diabetes or depression disease management programs (French & Fleming, 2002). Whereas substantial empirical support exists for SBI in medical settings, there is very little in workplace settings. This collaborative public-private partnership aims to fill this gap by translating medical research into behavioral healthcare practice settings that can potentially reach tens of thousands of workers each year, and potentially save employers and health plans millions of dollars. Alcohol Education (Risk 1: Low Risk) Simple Advice (Risk 2: Hazardous) Advice + Brief Counseling (Risk 3: Harmful) Referral (Risk 4: Abuse or Dependence) F Feedback X X X X R Responsibility X X X X A Advise X X X A Assess X X A Assist X X M Menu (Options) X X X X E Empathy X X X X S Strengths X X X X X Screens Risk 1 Risk 2 Risk 3 Risk 4 Objective 1: Describe alcohol SBI results from the multi-site pilot study. 1 68 56 4 2 6 MH/SA Refer 6 SBI Training: Modified the WHO alcohol screening and brief intervention (SBI) protocol (WHO, Babor et al., 2001 & 2004). More information about OptumHealth Behavioral Solutions: http://www.inside.optumhealth.com/Home/ Alcohol screening is integrated into telephonic clinical intake conducted by EAP clinical consultant. Figure 1 presents an overview of the EAP SBI workflow. AUDIT score classifies member into one of four risk categories: Risk Zone I – no or low-risk drinking Risk Zone II – hazardous drinking Risk Zone III – harmful drinking Risk Zone IV – abuse or dependence drinking Table 1 presents components of the brief intervention. The BI approach was modified using the WHO FRAMES approach. The components include: Feedback Responsibility Advise Assess Assist Menu (Options) Empathy Strengths Findings EAP Refer 48 2 72 58 4 2 8 8 46 3 65 48 10 1 6 5 43 4 61 44 14 1 2 5 38 5 39 31 4 2 2 2 29 6 35 28 3 1 3 3 21 7 27 22 2 0 3 1 22 Total 367 287 41 9 30 30 247 Design: Quasi-experimental design. Target Population: EAP members from a single health plan served by three EAP call centers. SBI Intervention: First, we ran descriptive statistics on primary outcomes including the number of positive alcohol screens, and the number (and type) of referrals. Second, chi-square analyses were run to examine whether the telephonic SBI program could be associated with increased identification rates of alcohol misuse. Design and Methods A quasi-experimental design is used to examine the feasibility and preliminary impact of an alcohol SBI pilot program implemented by EAP clinical consultants in three telephonic call centers serving members of a large health plan. The SBI intervention is adapted based on the World Health Organization (WHO, Babor et al., 2001, 2004) alcohol SBI protocol. The intervention includes systematic routine alcohol screening using the AUDIT during clinical intake, brief counseling using motivational interviewing (MI) for at-risk drinking, alcohol education, referral to face-to-face counseling or other treatment as appropriate. EAP Administrative Data: Positive alcohol screen. Analysis Table 2. Monthly Number of Completed Screens, Risk Levels, and Referrals Month Objective 2: Measure and compare alcohol identification rates 6-months pre-alcohol SBI launch vs. 6-months post-SBI. Measures: EAP completed 367 full AUDIT screens from August 2008 through February 2009. Table 2 presents monthly results. Overall: 287 (78%) scored in Risk Zone I – no or low-risk drinking 41 (11%) scored in Risk Zone II – hazardous drinking 9 (3%) scored in Risk Zone III – harmful drinking 30 (8%) scored in Risk Zone IV – alcohol abuse or dependence drinking Using EAP administrative data, there were 681 members from the health plan who used EAP services 6 months prior to alcohol SBI launch (“pre-SBI group”). We compared alcohol identification rates between (1) pre-SBI period and (2) post-SBI period. 80/367 (22%) screened positive in the post-SBI period compared to 31/681 (4.5%) in the pre-SBI period, which was statistically significant (chi-square=73.25, df 1, p<.001). Conclusions A telephonic alcohol SBI protocol modified for EAP delivery is feasible and highly acceptable. Slightly more than 1 out of 5 screened positive for hazardous or more severe alcohol use, and brief telephonic interventions were delivered to promote abstinence or reductions in substance use. Telephonic EAP alcohol SBI is associated with improved rates of alcohol identification compared to usual care. Ongoing Activities OptumHealth and GWU are completing final analyses of this pilot project to include a full set of screening and EAP/MH behavioral health claims data to assess effects. Results from this pilot will be used to improve quality of services across the book of business within OptumHealth. OptumHealth and GWU will continue to work collaboratively to advance the science of alcohol SBI in non-medical settings, as well as to improve MBHO services. Future advances in evaluating and improving EAP telephonic alcohol SBI protocols include assessing the impact on member health and productivity at follow-up including changes in risky drinking (alcohol consumption) and productivity at 30, 60, and 90 days. Contacting Author Information: Gregory Greenwood, PhD, MPH; Gregory_L_Greenwood@uhc.com; 415-265-7858