Document 5483481
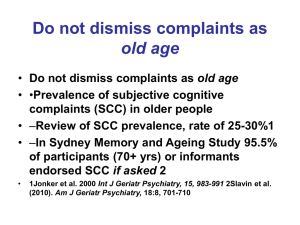
advertisement
Behavioural and Psychological Symptoms of Dementia Non-pharmacological and pharmacological approaches Dr Joy Ratcliffe, Consultant Psychiatrist Dr Julie Colville, Clinical Psychologist Lorraine Smith, Advanced Practitioner Manchester Mental Health and Social Care Trust & CMFT BPSD What is it? Heterogeneous group non- cognitive behaviours Not a diagnostic category – but very important Think as a list of disturbed behaviours e.g. Wandering Agitation Sexually disinhibited behaviours Aggression Paranoia/suspicion Eliciting psychological/psychiatric problems e.g. depression, anxiety, delusional ideas/psychosis All adds to risk BPSD Behavioural and psychological symptoms of dementia (BPSD) are common They can be problematic in clinical practice and can form a significant part of the day-to-day work of primary care teams, later life psychiatry teams. CMHTs, inpatient and community settings. We need to improve recognition and management of BPSD Improved management can have a positive impact on the quality of life of our patients and carers both at home and in nursing/residential setting s Positive management may also delay 24hr care BPSD - Prevalence Vary widely Approx 2/3rds will experience BPSD at any one time Approx 1/3 in the ‘clinically significant ‘range Can rise to 80% in care homes 20% for BPSD in Alzheimer’s disease BPSD tends to fluctuate with psycho-motor agitation most common and persistent BPSD - Impact BPSD rather than cognitive features are the major causes of care giving burden Paranoia, aggression, disturbed sleepwake cycles important drivers for 24hr care BPSD also associated with worse outcome and illness progression Adds significantly to direct and indirect care costs Multiple Factors that influence Behaviour Non Pharmacological management of BPSD – Must be ‘collaborative’ Needs thorough Assessment - multiple factors Need nursing home staff to input into assessment e.g. what do they know about their client? Need staff e.g. Nursing Home to play key part e.g. ABCs - helps identify factors such as over/under stimulation, pain etc Need staff to implement and monitor plans Care Staff do need training in dementia Need medical staff to ensure physical problems optimally treated e.g. infection, pain Non Pharmacological management of BPSD Understanding client’s history, lifestyle, culture and preferences, including their likes, dislikes, hobbies and interests. Providing opportunities for the person to have conversations with other people. Ensuring the person has the chance to try new things or take part in activities they enjoy. Environmental factors-signage, lighting, photographs. Reminiscence therapy. Shared Care Shared care plans to enhance communication and collaboration. Discuss shared care plan. Principle of Behaviour Management - Observing and Describing What is happening When does it happen How often does it happen Who is there when it’s happening What is communication like Why do you think it is happening Any other observations Principles of Behaviour Management - Contingencies What are we targeting: Frequency/ severity High frequency/ low severity (lower consequences) Low frequency/high severity (higher consequences) High frequency/High severity (highest consequences) What are ‘contingencies? e.g. positive and negative reinforcement Biological Management • • • • • • • • Treat underlying cause Psychotropics? Severity Risk Distress Medical comorbidity / other meds esp vascular risks Capacity Views carers Assessment Delirium (caution not to miss hypoactive)? PINCH ME (pain, infection, nutrition, constipation, hydration, medications, environment) PAIN (physical / pain, activity related, iatrogenic, noise / environment) START LOW GO SLOW Review target symptoms and adverse effects How long to treat for Gradual withdrawal Licensed? • • • • • • • Psychosis- risperidone (0.25-0.5mg bd), olanzapine (2.510mg), quetiapine (25-150mg) amisulpiride, aripiprazole, zuclopethixol Aggression- as above, trazadone, clomethiazole Agitation / anxiety- as above, citalopram, mirtazepine, memantine (AD), pregabalin Depression- sertraline, citalopram, mirtazepine Mania- valproate, lithium, antipsychotics Apathy- sertraline, citalopram, cholinesterase inhibitor (D, R, G) Sleep- temazapam, zopiclone, melantonin Lewy Body Dementia (LBD) CAUTION WITH ANTIPSYCHOTICS- quetiapine, aripiprazole, clozapine 1st choice cholinesterase inhibitors Clonazepam for REM sleep disorders Vascular Dementia (VD) Cholineterase inhibitors and memantine not licensed but majority of cases mixed AD / VD Cholinesterase Inhibitors Bradycardia Prolonged QTC LBBB Gastric bleeding risk (pmhx, aspirin, NSAIDS, warfarin) COPD / asthma Epilepsy Antipsychotics ECG, QTC, other changes Vascular risks Increase cognitive impairment Antidepressants Sedation GI bleeding Na Falls (inc SSRIs) Citalopram –QTC, max dose 20mg Anticonvulsants Limited evidence Adverse effects Case Example Case example 75, female, vascular dementia, 24 hr care for 12 months Complaints from care staff agitation ‘breathless’ hyperventilating, ‘attention seeking’ – calling every 5 mins Saying pain (but where?) toileting – incontinent faeces falls, (needing extra monitoring) Case Example PERSONAL – lived alone many years – over stimulated - remove to quieter environment DEMENTIA – vascular with periods disorientation unable to express distress (language) - try and reorientation/reassurance spend time with Case Example PHYSICAL – incontinence = ‘overflow’ compacted, meds 2 x laxatives and codeine (opposite actions?), pain (unable to express) - Elimination of acute physical illness as triggers for BPSD. Reviewed with Advanced Practitioner GP to check pain and review meds, FALLS – interaction meds Trazadone and codeine , over –sedated - meds review, Falls Team, Physio, frame Case Example PSYCHOLOGICAL – fear of falling exacerbated by previous falls, highly anxious (premorbidly – calling ambulance, GP, police etc) Ongoing assessment by Psychology, anxiety still prominent Linked to disorientation and/or premorbid anxiety Activity/distraction, optimal? Co pharmacological treatments – optimally treated?