Junior doctor dementia induction 20110725
advertisement
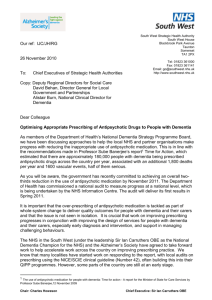
The Right Prescription A Call to Action for junior doctors on the use of antipsychotic drugs for people with dementia The numbers • 750,000 people with dementia in the UK • 180,000 people with dementia on antipsychotics • Only 36,000 will derive some benefit from antipsychotics, but: – 1800 additional deaths – 1620 additional CVAs Perhaps 2/3 of these prescriptions are unnecessary if appropriate support is available Non-cognitive symptoms of dementia Behavioural and psychological symptoms (BPSD) occur in 90% of people with dementia and may include… Behavioural disturbances • Agitation • Aggression • Wandering • Sleep disturbances • Changes in, or inappropriate eating behaviour • Inappropriate sexual behaviour Psychiatric symptoms • Depression • Anxiety • Delusions • Hallucinations • Paranoid ideas • Misidentifications Ask yourself – how many times have you seen these symptoms in someone with dementia? Remember, dementia is not just having a ‘poor memory’! Antipsychotics used in dementia • These include older antipsychotic drugs (e.g. halopeirdol) or newer medications (e.g. quetiapine, olanzapine, risperidone, amisulpride, aripiprazole) • Side effects: greater in older people - increased stroke risk, increased cardiovascular risk, Parkinsonian side effects, falls, additional deaths • These are class effects, not limited to one particular drug • Not licensed for the treatment of agitation (except risperidone) • 20-30% of people in nursing homes with dementia are on an antipsychotic • NHS survey 2007/8: 5.3% of people over 65 are prescribed an antipsychotic • These drugs are often inappropriately prescribed to ‘control’ BPSD Some alternatives to antipsychotics Simple patient-centred care plans can help prevent and soothe behavioural and psychological symptoms in patients with dementia whilst in hospital: • • • • High quality ward and nursing environment Availability of appropriate activities for patients with dementia in hospital Remember – collateral history is extremely helpful Your clinical assessment: – Behavioural assessment – ABC • • • • Antecedents Behaviour Consequences – Physical assessment, eg are they in pain? – Mental state assessment to consider alternative causes and treatments, eg for depression or sleep disturbance – Look at the mnemonic opposite as a guide for assessing causes of symptoms in people with dementia Refer if necessary to Medicine for the Elderly or Old Age Psychiatry Think ‘PINCH ME’ to identify any treatable causes of symptoms • Pain • Infection • Constipation • Hydration • Medication • Environmental Where you can make the difference • Establish if your patient with dementia has an individual care plan to help prevent and manage behavioural and psychological symptoms (BPSD) • Carry out a full medical assessment to consider other reasons for BPSD and try other treatments accordingly, eg: think ‘PINCH ME’! • Consider non-pharmacological alternatives such as reviewing the environment before prescribing antipsychotics for BPSD • Involve the patient (where possible), the patient’s carer and/or family in deciding what treatment is best • If you do prescribe an antipsychotic: – – – – Always monitor carefully for side-effects Always make it time limited for review at discharge, or clearly communicate with the patient’s GP why it was prescribed and that it needs review Do not prescribe antipsychotic drugs for longer than 12 weeks without consulting a specialist doctor Also consider referral to the care of the elderly team and/or old age psychiatry team Junior Doctor Call to Action We commit to carefully considering whether or not a prescription for antipsychotic medication is appropriate for someone with dementia who is in hospital and to reviewing the prescription on transfer or discharge from hospital Junior Doctor Call to Action Find out more and join us at www.institute.nhs.uk/HospitalDoctorsC2A And for a range of professional and patient leaflets and information, visit the Alzheimer’s society at www.alzheimers.org.uk