Psychology of Persistent Pain

Psychology of Persistent Pain
Putting Pain in Perspective
Pain defined
• “ An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”
International Association for the Study of Pain , 1994
Subjectivity of Pain
• Pain is always a subjective experience
• Everyone learns the meaning of “pain” through experiences usually related to injuries in early life
Dimensions of Chronic Pain
Loneliness
Social Factors
Hostility
Anxiety
Depression
Psychological Factors
Pathological Process
Physical Factors
A.G. Lipman, Cancer Nursing, 2:39, 1980
Is pain a learned behavior?
• William Fordyce - Operant conditioning model
• Pain behaviour is rewarded by
– solicitous attention
– not having to work
– access to drugs
• To treat need to: ignore pain behavior, reward non-pain behavior (e.g. physical activity)
Fordyce WE. Behavioral methods in chronic pain and illness. St. Louis: Mosby; 1976.
Biobehavioral Model
Pre-dispositional
Factors
Cultural and spiritual factors
Physiological/pathological
Tissue injury
Social factors
Pain perceptions
Behavioral factors
Psychological factors
Neuroplasticity/central sensitization
Functional outcomes
Fear Avoidance Model
Fear of Pain and Re-injury
• Fear of pain, movement, or re-injury thought to lead to avoidance behaviors and hyper-vigilance to pain
Disability
Social & Environmental Factors
• Environmental responses to pain behaviors can inadvertently reinforce pain & disability.
• There are several examples of reinforcements:
– Attention and affection from partner/caregivers
– Attention from health care provider(s)
– Pain medication
– Financial incentives/disincentives
Cognitive Factors
• Beliefs about Pain
• Readiness to Change
• Self-Efficacy
• Cognitive Coping Skills
• Cognitive Errors
Cognitive Errors
• Catastrophizing
• Dichotomous Thinking
• Overgeneralization:
Cognitive Errors
• Selective Abstraction
• “Should” statements
• Entitlement Fallacy
Personality Styles
• High needs for Perfectionism, Control, and/or
Approval from others
• Intolerance of Uncertainty
• Extroversion is associated with higher pain thresholds
• External Locus of Control vs. Internal
• Experiential Avoidance
• Psychological Inflexibility
• A Heightened Sense of Entitlement
Comorbidities and pain
• Anxiety/Fear (25%-50%)
• Anger and Frustration
(50%-80%)
• Insomnia (50%-80%)
• Medication Misuse
• Sexual Dysfunction
• Family Dysfunction
Depression and Pain
• Depression is common in patients who experience persistent pain
• Degree of depression is also greater in patients who rate their pain higher
Fishbain, D. A., Cutler, R., Rosomoff, H. L., & Rosomoff, R. S. (1997). Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clin.J Pain 13, 116-137.
OR
Fishbain, D. A., Cutler, R., Rosomoff, H. L., & Rosomoff, R. S. (1997). Chronic painassociated depression: antecedent or consequence of chronic pain? A review. Clin.J
Pain 13, 116-137.
Treatment – Psychological Approach
Cognitive Behavioral Treatment
(CBT)
• Mindful Meditation
• Education/Motivational Enhancement
• Goal Setting (Realistic Expectations)
• Relaxation/Imagery
• Hypnosis/Distraction
• Biofeedback
• Correcting Cognitive Errors
• Graded Activity Exposure (Behavioural Activation)
Mindfulness Defined
• “ The awareness that emerges through paying attention on purpose, in the present moment, and non-judgmentally to the unfolding of experience moment to moment.
”
• Kabat-Zinn, 2003.
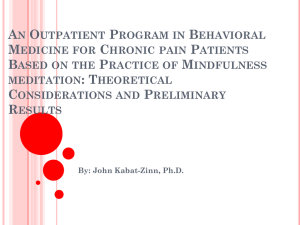
The clinical use of mindfulness meditation for the selfregulation of chronic pain.
Kabat-Zinn J, Lipworth L, Burney R.
Ninety chronic pain patients were trained in mindfulness meditation in a 10week Stress Reduction and Relaxation Program. Statistically significant reductions were observed in measures of present-moment pain, negative body image, inhibition of activity by pain, symptoms, mood disturbance, and psychological symptomatology, including anxiety and depression. Pain-
related drug utilization decreased and activity levels and feelings of self-
esteem increased. Improvement appeared to be independent of gender, source of referral, and type of pain. A comparison group of pain patients did not show significant improvement on these measures after traditional treatment protocols. At follow-up, the improvements observed during the meditation training were maintained up to 15 months post-meditation
training for all measures except present-moment pain. The majority of subjects reported continued high compliance with the meditation practice as part of their daily lives. The relationship of mindfulness meditation to other psychological methods for chronic pain control is discussed.
J Behav Med. 1985 Jun;8(2):163-90.
Being Mindful
- Jon Kabat-Zinn
•
Mindfulness creates space around our pain, allowing us to work with it without being overwhelmed.
Mindfully Working with Pain
3 Basic Strategies for Working with Pain:
1.
focusing on the pain
2.
focusing on the mental and emotional reactions to the pain
3.
focusing away from the pain onto something soothing and pleasant
Mindfully Working with Pain
Methods:
Free-Floating with the Discomfort
Breath Pleasure
Relaxing with Out Breath
Pleasure of O
2
Entering the Body
Acute exacerbation of pain- CBT management
• Provide information
• Relaxation Techniques including
– Breathing
– PMR (progressive muscle relaxation)
– Imagery
– Hypnosis
• Cognitive (i.e., Positive Coping Self- Statements,
Distraction, Sensory Focus)
Relaxation video – Guided Imagery
http://www.healingchronicpain.org/content/re lax/default.asp
Progressive
Relaxation
Guided Imagery
CBT – Chronic Pain Management
• Teach Activity-Rest
Cycling (Pacing)
• Patients learn that activity causes pain
• Pain and suffering increase over time
• Activity decreases over time
CBT – Chronic Pain Management
• Time-Contingent Medication Use
• Relapse Prevention
• Acceptance (e.g., Mindfulness Meditation)
• Couples/Family Communication Therapy
• Treat Co-morbid Conditions
Motivate Self management
• Maintain Respect for the Dignity of the Patient
• Defuse Myths about Chronic Pain
• Avoid “Psychologizing” the Problem
• “Listen” and Avoid Power Struggles
• Communicate Understanding in the Reality of
Pain Experience
Motivating Self management
• Introduce a Model (eg., Gate Control)
• Encourage Realistic Expectations
– (eg., 50% pain reduction, improved daily function, etc.)
• Get a Commitment from the Patient
• Collaborate With the Patient Against “it”
Avoid these messages to the client
• Let pain be your guide
• The pain is being caused by psychological factors
• The pain is not real – there is no reason for your pain
Messages to Give Clients
• Pain can cause suffering
• Can’t always change pain, but you can reduce suffering
• Reducing suffering and pain behavior can lead to reduced pain
“Pain may be inevitable but misery is optional”
Dee Malchow, RN, amputee