Munchausen`s Syndrome by Proxy
advertisement
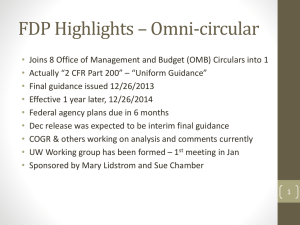
Beyond MSBP or, Why I Hate Munchausen Syndrome by Proxy John Stirling, MD Santa Clara Valley Medical Center San Jose CA Stanford University Beyond MSBP or, Why I Hate Munchausen Syndrome by Proxy John Stirling, MD Santa Clara Valley Medical Center San Jose CA Stanford University Bea Yorker, RN, JD University of California, Los Angeles The standard medical talk… • • • • • Pathophysiology Symptoms Diagnosis Treatment Polite applause The trouble with “Munchausen Syndrome by Proxy” • • • • • • • It’s an eponym It’s not really a syndrome It’s not really a disease It’s not really a diagnosis It’s medical… and psychiatric… and social It’s very hard to treat It’s hard to spell “Primum non nocere” The trouble with “Munchausen Syndrome by Proxy” • • • • What to call it? Who can diagnose? Where’s the threshold? When to involve the authorities? Take Home Points • Not a single condition, but a variety of presentations along a spectrum of severity • MBP is a dyadic diagnosis; PCF/FDP are individual diagnoses • Child abuse is child abuse, whatever the context • Evaluations have to be exhaustive • …and involve physicians Beyond Munchausen Syndrome by Proxy: Identification and Treatment of Child Abuse in a Medical Setting Pediatrics 2007;119;1026-1030 A clinical report from the Committee on Child Abuse and Neglect of the American Academy of Pediatrics Why Another Report? To remind pediatricians: • Children are injured by factitious illness • Harm often requires physician’s complicity • We can’t usually diagnose it alone (much less treat it), but • Medical input is essential to diagnosis • Our focus is on harm to the child Background Background • Asher, 1951: “Munchausen Syndrome” • Kempe, 1975: “Uncommon manifestations of Battered Child Syndrome” • Meadow, 1977: “Munchausen Syndrome by Proxy: The hinterland of child abuse” • Rosenberg, 1987: “The web of deceit” Diagnosis Definition Rosenberg (1987): • Illness in a child which is simulated and/or produced by someone in loco parentis • Presentation of the child for medical assessment and care, usually persistently, often resulting in multiple medical procedures • Denial of knowledge by the perpetrator • Acute symptoms abate with separation Definition DSM-IV (1994) “Factitious Disorder by Proxy”: (A) Intentional production or feigning of physical or psychological signs or symptoms in another person who is under the individual's care. (B) The motivation for the perpetrator's behavior is to assume the sick role by proxy. (C) External incentives for the behavior (such as economic gain) are absent. (D) The behavior is not better accounted for by another mental disorder. (p. 727) Definition Jenny (2008),“Medical Child Abuse”: A child receiving unnecessary and harmful or potentially harmful medical care at the instigation of the caretaker. DSM – V (proposed) Factitious Disorder Imposed on Another (previously, Factitious Disorder By Proxy) • To make this diagnosis, all 4 criteria must be met. Note that the perpetrator, not the victim, receives this diagnosis. • 1. A pattern of falsification of physical or psychological signs or symptoms in another, associated with identified deception. • 2. A pattern of presenting another (victim) to others as ill or impaired. • 3. The behavior is evident even in the absence of obvious external rewards. • 4. The behavior is not better accounted for by another mental disorder such as delusional belief system or acute psychosis. Presentations Spectrum: • Exaggeration of symptoms • Fabrication of symptoms • Induction of symptoms resulting in harm to child, through actions of caregiver, in a medical setting Presentations: Top ten: – Apnea/cyanosis – Feeding problems/anorexia – Seizures – Behaviors – Asthma/allergy – Fever/pain… No common presentation! Presentations: • Symptoms actively produced in 57% – Suffocation, drugs, poisons, etc. – Half while child was in the hospital! • Many had unrelated injuries, neglect, FTT • Average of 3.25 medical conditions What do we know? Web of deceit: a literature review of Munchausen Syndrome by Proxy - Rosenberg, Donna A., Child Abuse & Neglect, 1987 The deceit continues: an updated literature review of Munchausen Syndrome by Proxy - Sheridan, Mary S., Child Abuse & Neglect, 2003 Warning! Caveats: • Literature review isn’t random • Diagnoses not equally certain • Series often span years • Inconsistent approaches Typology: Victims • • • • Male = Female Average age: 48 months Time to diagnosis: 22 months Outcomes: long-term disability in 7-8%, death in 6-9% • Siblings: 25% of sibs dead, half under “suspicious circumstances” Typology: Perpetrators • • • • • Female >> Male Mothers heavily represented Medical background: 14-27% Munchausen features in caregiver: 29% Psych diagnosis: 23% – Depression, personality disorders, somatization Terminology/Definition • Pediatric or Psychiatric diagnosis? • MSBP or MBPS? • Pediatric focus: identify and mitigate harm to the child “Primum non nocere” Terminology/Definition • APSAC: PCF + FDP = M(S)BP • Pediatric Condition Falsification, plus • Factitious Disorder by Proxy, equals • Munchausen by Proxy Terminology/Definition • FDP is not a mental disorder • PCF and FDP can occur independently • Examples: – PCF without FDP – Harm to the child without PCF or FDP – “Lookalikes” “…a rose by any other name…” MSBPA? MSBP? MBPS? PCF + FDP? = Child Abuse! Special Note: … if a physician has real evidence to suspect child abuse, regardless of the motive of the perpetrator, it must be investigated and the perpetrators brought to swift and effective justice! In contrast, often the agenda behind Munchausen Syndrome by Proxy is to be able to make an accusation without evidence, but by the Munchausen Syndrome By Proxy profile . If it is in fact a crime has been committed, call it by it's real name...suffocation, poisoning, tampering with urine sample, etc....offer evidence! You don't need fancy labels or self-proclaimed experts to line their pockets pretending to be the only ones who know how to diagnose a crime. Backlash! Diagnosis • What’s a diagnosis? – “Differential diagnosis” – Degrees of certainty • Diagnostic criteria – Inclusion vs exclusion Diagnosis • How important is the caretaker’s motive? • How useful is a profile? Diagnosis Difficult because: • Presentations vary greatly • Medical personnel are involved in harm • Multiple institutions, scattered records • Failure to consider the diagnosis • Failure to involve other professionals Diagnosis What’s proof?: • Confessions? • Improvement out of home? • Covert video surveillance? • Lab findings? Treatment • Child’s safety is the first priority • Use least restrictive option – Close observation – In-home dependency – Foster care – Criminal prosecution Clinical Advice • Consult child abuse pediatrician • Gather and review all medical records • Work as multidisciplinary team • Involve state Child Protection agency prn • Involve whole family in treatment Take Home Points • Not a single condition, but a variety of presentations along a spectrum of severity • MBP is a dyadic diagnosis; PCF/FDP are individual diagnoses • Child abuse is child abuse, whatever the context • Evaluations have to be exhaustive • …and involve physicians john.stirling@hhs.sccgov.org Case 1 • 3yo boy • 14 visits to PCP in past year, 3 to ED, usually after visitation • Parents share custody • Allegations of poor care: constipation, abdominal pain, possible sexual abuse • Father doesn’t adhere to Mom’s special diet Case 2 • 8yo twin girls • Mother describes allergic reactions to aero-allergens, behavioral symptoms • Naturopath supports her • Children missed 30 days of school last yr • Sleep on wooden panels, in mylar blankets, wear masks outside Case 3 • 6yo boy with asthma sx per mom • “meds don’t help” • Peak flow decreased in office, but improves w/ albuterol neb • Improvements not sustained at home • Mom asks for steroids • Wants disability papers filled out Other Cases?