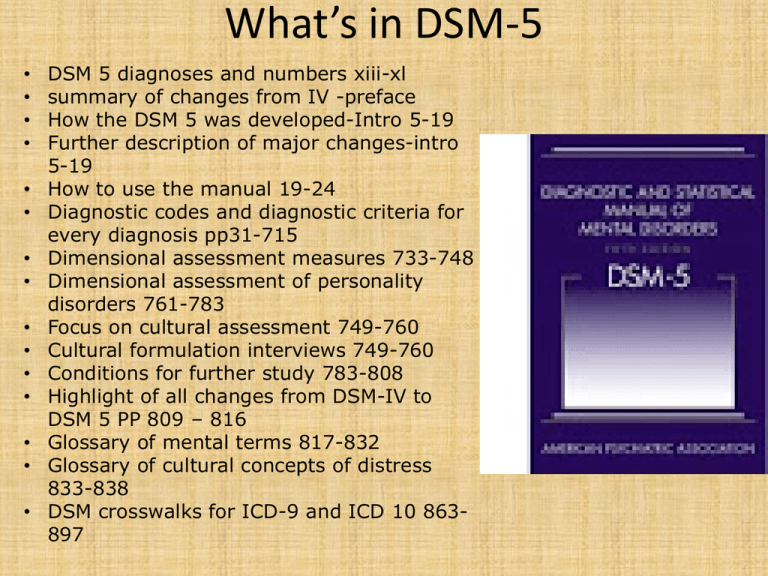
What’s in DSM-5
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
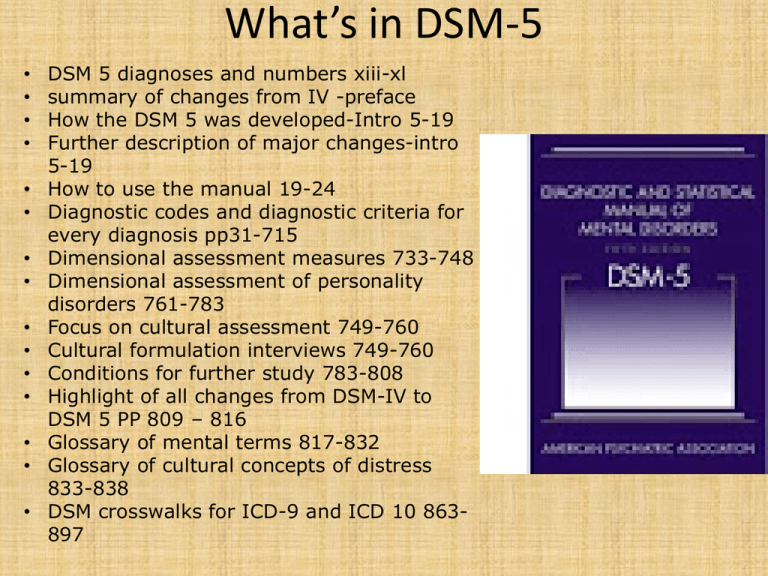
DSM 5 diagnoses and numbers xiii-xl
summary of changes from IV -preface
How the DSM 5 was developed-Intro 5-19
Further description of major changes-intro
5-19
How to use the manual 19-24
Diagnostic codes and diagnostic criteria for
every diagnosis pp31-715
Dimensional assessment measures 733-748
Dimensional assessment of personality
disorders 761-783
Focus on cultural assessment 749-760
Cultural formulation interviews 749-760
Conditions for further study 783-808
Highlight of all changes from DSM-IV to
DSM 5 PP 809 – 816
Glossary of mental terms 817-832
Glossary of cultural concepts of distress
833-838
DSM crosswalks for ICD-9 and ICD 10 863897
WHY CHANGE?
• DSM-IV’s organizational structure failed to
reflect shared features or symptoms of related
disorders and diagnostic groups (like psychotic
disorders with bipolar disorders, or
internalizing (depressive, anxiety, somatic) and
externalizing (impulse control, conduct,
substance use) disorders.
• DSM-IV Thin on Culture
•Did not represent or
integrate the latest
findings from
neuroscience, genetics
and cognitive research
•Multi axial structure
was out of line with
the rest of medicine
•Global assessment of
functioning was an
unreliable measure
•Decision trees did not
increase inter-rater
reliability
Other problems
• Separates diagnoses from treatment
• Diagnosis has become an end in itself! (billability &
pressure for scientific determinism)
• Minimizes TIME as a major factor in making diagnoses
• Minimizes emergent symptoms
• Minimizes lack of symptom clarity as an issue
• Ignores internal unobservables
• Funnels tx focus to symptom negation rather than wellbeing
• Forces clinician to make immediate diagnoses
• Forces clinician to more severe DX
• There have been no no established "zones of
rarity" between diagnosis (much symptom
overlap)
• Law-like biological markers have not yet been
found
• Categorical measurement (depressed vs NOT
depressed) doesn’t capture clinical variance
DSM III & IV limits
Focus on only what is observable; limits diagnostic
possibilities
Limited number of observable signs & symptoms
(12 to 19 symptoms )
Because law-like biomarkers have not been found,
Elements that cannot be seen directly
are excluded. This is exactly the opposite of
medicine which strives to see below the surface.
Limited number of observable signs/symptoms
But 400 diagnoses in DSM = diagnostic confusion
Simple counting of the number of symptoms in
Order to make a diagnosis DOES NOT WORK
DSM III & IV – problems with measuring
Limited number of observable signs and
Symptoms, Elements that cannot be seen directly
are excluded. This is exactly the opposite of
medicine which strives to see below the surface.
Limited number of observable signs/symptoms
But 400 diagnoses in DSM
# 1 Problem = under- determination of
diagnosis
Consequences = - boundary problems (paris)
- false positives
- rise of comorbidity
- problems of differential dx
- one size fits all diagnoses
- only agreement on most severe
The relationship between Categorical Dx,
comorbidity and increased reliability
• 1. no major depression; 2. major depression
• 1. No generalized anxiety 2. generalized anxiety
Depression
1
2
3
4
5
6
7
8
None minimal mild minor moderate major severe maximal
1
2
3
General anxiety
4
5
6
7
8
None minimal mild minor moderate major severe maximal
Categorical measurement increases potential for inter-rater
reliability. 50% chance of inter-rater reliability
Fewer choices = easier= less information = more possibility of
making mistake = inflated comorbidity
Categorical measures = No clinical variance & no diagnostic threshold
Decreasing variance increases potential for inter rater reliability and
increases potential for specious comorbidity
Dimensional measure
inter-rater reliability
lower = 12%
More choices = harder=
more info
Subtle distinctions ; less
Potential for specious
• DSM III & IV turned assessment into yes/no
decision trees
• Inflated comorbidity
• Inflated inter-rater reliability (but did not
increase it)
• Never established true biological markers
• Reduced the rigorousness of good assessment
in the name of clinical utility
DSM 5
1. Emphasizes dimensional measurement
2. Provides World Health Organization measure
of overall well-being
3. Does away with Axes
4. Focuses more on culture
5. Attempts to “Re-organize” diagnostic
categories according to what we now (think
we)know
6. Attempts to “re-group” individual diagnoses
according to what we now (think we) know
7. Includes crosswalks with ICD-9 and ICD 10
http://www.dsm5.org/Pages/Default.aspx
1. Dimensional measures
http://www.psychiatry.org/practice/dsm/dsm5/online-assessment-measures#Level1
• Allows clinician opportunity to “fine tune”
diagnosis
• Captures diagnostic complexity
• Should reduce inflated comorbidity. By allowing
inclusion of crosscutting symptoms (such as
anxiety) within other diagnoses
• Focuses assessment on crosscutting symptoms
• Creates "severity specifier" for many diagnoses
• Dimensions make diagnosis congruent with upto-date neurocognitive research indicating
symptoms are on a continuum
• DSM 5 adds dimensional
measures WITHOUT
abandoning categorical
measures
• Criteria are basically the
same as they were in the
DSM-IV
Crosscutting symptoms
(symptoms that can occur across many DXs)
• Captures symptom comorbidity without diagnostic
comorbidity
• Cross-cutting symptom measures may aid in a
comprehensive mental status assessment by drawing
attention to symptoms that are important across diagnoses.
They are intended to help identify additional areas of
inquiry that may guide treatment and prognosis. The crosscutting measures have two levels: Level 1 questions are a
brief survey of 13 domains for adult patients and 12
domains for child and adolescent patients, and Level 2
questions provide a more in-depth assessment of certain
domains.
http://www.psychiatry.org/practice/dsm/dsm5/online-assessment-measures#Level1
Table 1: Adult DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measure:
domains, thresholds for further inquiry, and associated Level 2 measures for
adults ages 18 and over
Domain
I.
Domain Name
Mild or greater
LEVEL 2—Depression—Adult (PROMIS Emotional Distress—Depression—Short
Form)1
Anger
Mild or greater
LEVEL 2—Anger—Adult (PROMIS Emotional Distress—Anger—Short Form)1
Mania
Anxiety
Mild or greater
Mild or greater
LEVEL 2—Mania—Adult (Altman Self-Rating Mania Scale)
LEVEL 2—Anxiety—Adult (PROMIS Emotional Distress—Anxiety—Short Form)1
Somatic Symptoms
Mild or greater
LEVEL 2—Somatic Symptom—Adult (Patient Health Questionnaire 15 Somatic
Symptom Severity [PHQ-15])
VI.
VII.
VIII.
Suicidal Ideation
Psychosis
Sleep Problems
Slight or greater
Slight or greater
Mild or greater
None
None
LEVEL 2—Sleep Disturbance - Adult (PROMIS—Sleep Disturbance—Short Form)1
IX.
X.
Memory
Repetitive Thoughts
and Behaviors
Mild or greater
Mild or greater
None
LEVEL 2—Repetitive Thoughts and Behaviors—Adult (adapted from the Florida
Obsessive-Compulsive Inventory [FOCI] Severity Scale [Part B])
XI.
XII.
Dissociation
Personality
Functioning
Substance Use
Mild or greater
Mild or greater
None
None
Slight or greater
LEVEL 2—Substance Abuse—Adult (adapted from the NIDA-modified ASSIST)
II.
III.
IV.
V.
XIII.
Depression
Threshold to guide DSM-5 Level 2 Cross-Cutting Symptom Measure available online
further inquiry
DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measure—Adult
During the past TWO (2) WEEKS, how much (or how often) have you been bothered by the
following problems?
None
Slight
Not at
Rare, less
than a day
or two
all
I.
Mild
Moderate
Several
days
Severe
(clinician)
1. Little interest or pleasure in doing things?
0
1
2
3
4
2. Feeling down, depressed, or hopeless?
0
1
2
3
4
II.
3. Feeling more irritated, grouchy, or angry than usual?
0
1
2
3
4
III.
4. Sleeping less than usual, but still have a lot of energy?
0
1
2
3
4
5. Starting lots more projects than usual or doing more risky things than usual?
0
1
2
3
4
6. Feeling nervous, anxious, frightened, worried, or on edge?
0
1
2
3
4
7. Feeling panic or being frightened?
0
1
2
3
4
8. Avoiding situations that make you anxious?
0
1
2
3
4
9. Unexplained aches and pains (e.g., head, back, joints, abdomen, legs)?
0
1
2
3
4
IV.
V.
10. Feeling that your illnesses are not being taken seriously enough?
0
1
2
3
4
VI.
11. Thoughts of actually hurting yourself?
0
1
2
3
4
VII.
12. Hearing things other people couldn’t hear, such as voices even when no
0
1
2
3
4
13. Feeling that someone could hear your thoughts, or that you could hear what another
person was thinking?
0
1
2
3
4
VIII.
14. Problems with sleep that affected your sleep quality over all?
0
1
2
3
4
IX.
15. Problems with memory (e.g., learning new information) or with location
(e.g., finding your way home)?
0
1
2
3
4
X.
16. Unpleasant thoughts, urges, or images that repeatedly enter your mind?
0
1
2
3
4
17. Feeling driven to perform certain behaviors or mental acts over and over again?
0
1
2
3
4
XI.
18. Feeling detached or distant from yourself, your body, your physical surroundings, or
your memories?
0
1
2
3
4
XII.
19. Not knowing who you really are or what you want out of life?
0
1
2
3
4
20. Not feeling close to other people or enjoying your relationships with them?
0
1
2
3
4
21. Drinking at least 4 drinks of any kind of alcohol in a single day?
0
1
2
3
4
22. Smoking any cigarettes, a cigar, or pipe, or using snuff or chewing tobacco?
0
1
2
3
4
23. Using any of the following medicines ON YOUR OWN, that is, without a doctor’s
prescription, in greater amounts or longer than prescribed [e.g., painkillers (like
Vicodin), stimulants (like Ritalin or Adderall), sedatives or tranquilizers (like sleeping
pills or Valium), or drugs like marijuana, cocaine or crack, club drugs (like ecstasy),
hallucinogens (like LSD), heroin,
inhalants or solvents (like glue), or methamphetamine (like speed)]?
0
1
2
3
4
one was around?
XIII.
Highest
More than
Nearly Domain
half the days every day
Score
THE CROSS-CUTTING SYMPTOM MEASURES CAN DO THREE THINGS
1. POINT YOU IN THE RIGHT DIRECTION DIAGNOSTICALLY (LEVEL I)
2. GIVE YOU A BASIC SENSE OF THE CLINICAL PROFILE OF EACH CLINET
3. CAPTURE SYMPTOMS THAT ARE LIKELY TO OCCUR ACROSS
DIAGNOSIS, BUT NOT NECESSARILY QUALIFY FOR ITS OWN DX
DEPRESSION
ANXIETY
SOMATIC SYMPTOMS
SLEEP ISSUES ETC.
level II measures(Dimensional)
• Level II crosscutting measures
– Focus on one specific domain
– Provides a more varied clinical profile within that
domain
– Allows for follow-up exploration with more than one
domain in order to specify diagnostic boundaries. (For
example, in my dealing with major depression with a
co-occurring anxiety disorder or major depression,
with anxious features
– Provides clinical verification before diagnosis
Level 2 measures of symptoms
• Level 2 questions provide a more in-depth
assessment of certain domains:
http://www.psychiatry.org/practice/dsm/dsm
5/online-assessment-measures# Level2
• Level 2 is given as a specific follow up, once
the clinician is ‘oriented’ in a symptomatic
direction they are focused WITHIN a specific
symptom domain
List of all the level 2 (disorder specific) cross-cutting symptom measures
Level 2 Cross-Cutting Symptom Measures
For Adults
LEVEL 2—Depression—Adult (PROMIS Emotional Distress—Depression—Short Form)
LEVEL 2—Anger—Adult (PROMIS Emotional Distress—Anger—Short Form)
LEVEL 2—Mania—Adult (Altman Self-Rating Mania Scale [ASRM])
LEVEL 2—Anxiety—Adult (PROMIS Emotional Distress—Anxiety—Short Form)
LEVEL 2—Somatic Symptom—Adult (Patient Health Questionnaire 15 Somatic Symptom Severity Scale [PHQ-15])
LEVEL 2—Sleep Disturbance—Adult (PROMIS—Sleep Disturbance—Short Form)
LEVEL 2—Repetitive Thoughts and Behaviors—Adult (Adapted from the Florida Obsessive-Compulsive Inventory [FOCI]
Severity Scale [Part B])
LEVEL 2—Substance Use—Adult (Adapted from the NIDA-Modified ASSIST)
For Parents of Children Ages 6–17
LEVEL 2—Somatic Symptom—Parent/Guardian of Child Age 6–17 (Patient Health Questionnaire 15 Somatic Symptom
Severity Scale [PHQ-15])
LEVEL 2—Sleep Disturbance—Parent/Guardian of Child Age 6–17 (PROMIS—Sleep Disturbance—Short Form)
LEVEL 2—Inattention—Parent/Guardian of Child Age 6–17 (Swanson, Nolan, and Pelham, version IV [SNAP-IV])
LEVEL 2—Depression—Parent/Guardian of Child Age 6–17 (PROMIS Emotional Distress—Depression—Parent Item Bank)
LEVEL 2—Anger—Parent/Guardian of Child Age 6–17 (PROMIS Emotional Distress—Calibrated Anger Measure—Parent)
LEVEL 2—Irritability—Parent/Guardian of Child Age 6–17 (Affective Reactivity Index [ARI])
LEVEL 2—Mania—Parent/Guardian of Child Age 6–17 (Adapted from the Altman Self-Rating Mania Scale [ASRM])
LEVEL 2—Anxiety—Parent/Guardian of Child Age 6–17 (Adapted from PROMIS Emotional Distress—Anxiety—Parent Item
Bank)
LEVEL 2—Substance Use—Parent/Guardian of Child Age 6–17 (Adapted from the NIDA-Modified ASSIST)
For Children Ages 11–17
LEVEL 2—Somatic Symptom—Child Age 11–17 (Patient Health Questionnaire 15 Somatic Symptom Severity Scale [PHQ-15])
LEVEL 2—Sleep Disturbance—Child Age 11–17 (PROMIS—Sleep Disturbance—Short Form)
LEVEL 2—Depression—Child Age 11–17 (PROMIS Emotional Distress—Depression—Pediatric Item Bank)
LEVEL 2—Anger—Child Age 11–17 (PROMIS Emotional Distress—Calibrated Anger Measure—Pediatric)
LEVEL 2—Irritability—Child Age 11–17 (Affective Reactivity Index [ARI])
LEVEL 2—Mania—Child Age 11–17 (Altman Self-Rating Mania Scale [ASRM])
LEVEL 2—Anxiety—Child Age 11–17 (PROMIS Emotional Distress—Anxiety—Pediatric Item Bank)
LEVEL 2—Repetitive Thoughts and Behaviors—Child Age 11–17 (Adapted from the Children’s Florida Obsessive Compulsive
Inventory [C-FOCI] Severity Scale)
LEVEL 2—Substance Use—Child Age 11–17 (Adapted from the NIDA-Modified ASSIST)
Table 1: Adult DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measure:
domains, thresholds for further inquiry, and associated Level 2 measures for
adults ages 18 and over
Hypothetically scores on our client using level I crosscutting symptoms indicated
the following areas circled
Domain
I.
II.
III.
IV.
V.
Domain Name
Depression
Threshold to guide DSM-5 Level 2 Cross-Cutting Symptom Measure available online
further inquiry
b
Mild or greater
LEVEL 2—Depression—Adult (PROMIS Emotional Distress—Depression—Short
Form)1
Anger
Mild or greater
LEVEL 2—Anger—Adult (PROMIS Emotional Distress—Anger—Short Form)1
Mania
Anxiety
Mild or greater
Mild or greater
LEVEL 2—Mania—Adult (Altman Self-Rating Mania Scale)
LEVEL 2—Anxiety—Adult (PROMIS Emotional Distress—Anxiety—Short Form)1
Somatic Symptoms
b
Mild or greater
b
LEVEL 2—Somatic Symptom—Adult (Patient Health Questionnaire 15 Somatic
Symptom Severity [PHQ-15])
VI.
VII.
VIII.
Suicidal Ideation
Psychosis
Sleep Problems
Slight or greater
Slight or greater
Mild or greater
None
None
LEVEL 2—Sleep Disturbance - Adult (PROMIS—Sleep Disturbance—Short Form)1
IX.
X.
Memory
Repetitive Thoughts
and Behaviors
Mild or greater
Mild or greater
None
LEVEL 2—Repetitive Thoughts and Behaviors—Adult (adapted from the Florida
Obsessive-Compulsive Inventory [FOCI] Severity Scale [Part B])
XI.
XII.
Dissociation
Personality
Functioning
Substance Use
Mild or greater
Mild or greater
None
None
XIII.
b
b
Slight or greater
LEVEL 2—Substance Abuse—Adult (adapted from the NIDA-modified ASSIST)
LEVEL 2—Depression—Adult* *PROMIS Emotional Distress—Depression—Short Form
Name:
Age:
Sex: Male Female
Date:_
If the measure is being completed by an informant, what is your relationship with the individual receiving care?
In a typical week, approximately how much time do you spend with the individual receiving care?
hours/week
Instructions: On the DSM-5 Level 1 cross-cutting questionnaire that you just completed, you indicated that during the past 2 weeks you (the
individual receiving care) have been bothered by “no interest or pleasure in doing things” and/or “feeling down, depressed, or hopeless” at a mild
or greater level of severity. The questions below ask about these feelings in more detail and especially how often you (the individual receiving
care) have been bothered by a list of symptoms during the past 7 days. Please respond to each item by marking (P or x) one box per row.
Clinician
Use
In the past SEVEN (7) DAYS....
Never
Rarely
Sometimes
Often
Always
1.
I felt worthless.
q 1
q2
q3
q4
q5
2.
I felt that I had nothing to look forward to.
q 1
q2
q3
q4
q5
3.
I felt helpless.
q 1
q2
q3
q4
q5
4.
I felt sad.
q 1
q2
q3
q4
q5
5.
I felt like a failure.
q 1
q2
q3
q4
q5
6.
I felt depressed.
q 1
q2
q3
q4
q5
7.
I felt unhappy.
q 1
q2
q3
q4
q5
8.
I felt hopeless.
q 1
q2
q3
q4
q5
Total/Partial Raw Score:
Prorated Total Raw Score:
T-Score:
Item
Score
LEVEL 2—Substance Use—Adult* *Adapted from the NIDA-Modified ASSIST
Name:
Age:
Sex: q Male q Female
Date:
If the measure is being completed by an informant, what is your relationship with the individual receiving care?
In a typical week, approximately how much time do you spend with the individual receiving care?
hours/week
Instructions: On the DSM-5 Level 1 cross-cutting questionnaire that you just completed, you indicated that during the past 2 weeks you
(the individual receiving care) have been bothered by “using medicines on your own without a doctor’s prescription, or in greater amounts
or longer than prescribed, and/or using drugs like marijuana, cocaine or crack, and/or other drugs” at a slight or greater level of severity.
The questions below ask how often you (the individual receiving care) have used these medicines and/or substances during the past 2
weeks. Please respond to each item by marking (P or x) one box per row.
During the past TWO (2) WEEKS, about how often did you use any of the following
medicines ON YOUR OWN, that is, without a doctor’s prescription, in greater amounts
or longer than prescribed?
Clinician
Use
Not at all
One or
two days
Several
days
More than
half the days
Nearly
every day
a.
Painkillers (like Vicodin)
q 0
q1
q2
q3
q4
b.
Stimulants (like Ritalin, Adderall)
q 0
q1
q2
q3
q4
c.
Sedatives or tranquilizers (like sleeping
pills or Valium)
q 0
q1
q2
q3
q4
Or drugs like:
d.
Marijuana
q 0
q1
q2
q3
q4
e.
Cocaine or crack
q 0
q1
q2
q3
q4
f.
Club drugs (like ecstasy)
q 0
q1
q2
q3
q4
g.
Hallucinogens (like LSD)
q 0
q1
q2
q3
q4
h.
Heroin
q 0
q1
q2
q3
q4
i.
Inhalants or solvents (like glue)
q 0
q1
q2
q3
q4
j.
Methamphetamine (like speed)
q 0
q1
q2
q3
q4
Total Score:
Useless for alcohol. Perhaps ADS
Item Score
Level 2 cross-cutting scale for Somatic symptoms - Adult
LEVEL 2—Somatic Symptom—Adult Patient*
*Adapted from the Patient Health Questionnaire Physical Symptoms (PHQ-15)
Name:
Age:
Sex: q Male q Female
Date:
If the measure is being completed by an informant, what is your relationship with the individual receiving care?
In a typical week, approximately how much time do you spend with the individual receiving care?
hours/week
Instructions: On the DSM-5 Level 1 cross-cutting questionnaire that you just completed, you indicated that during the past 2 weeks you (the individual receiving care) have been
bothered by “unexplained aches and pains”, and/or “feeling that your illnesses are not being taken seriously enough” at a mild or greater level of severity. The questions below ask
about these feelings in more detail and especially how often you (the individual receiving care) have been bothered by a list of symptoms during the past 7 days. Please respond to
each item by marking (P or x) one box per row.
Clinician
Use
Item
Score
During the past 7 days, how much have you been bothered by any of the following problems?
Not bothered
at all
0
1.
Stomach pain
2.
Back pain
3.
Pain in your arms, legs, or joints (knees, hips, etc.)
4.
Menstrual cramps or other problems with
your periods WOMEN ONLY
5.
Headaches
6.
Chest pain
7.
Dizziness
8.
Fainting spells
9.
Feeling your heart pound or race
10.
Shortness of breath
11.
Pain or problems during sexual intercourse
12.
Constipation, loose bowels, or diarrhea
13.
Nausea, gas, or indigestion
14.
Feeling tired or having low energy
15.
Trouble sleeping
Bothered
a little
1
Bothered
a lot
2
Total/Partial Raw Score:
Prorated Total Raw Score: (if 1-3 items left unanswered)
LEVEL 2—Anxiety—Adult* *PROMIS Emotional Distress—Anxiety—Short Form
Name:
Age:
Sex: q Male q Female
Date:
If the measure is being completed by an informant, what is your relationship with the individual?
In a typical week, approximately how much time do you spend with the individual?
hours/week
Instructions to patient: On the DSM-5 Level 1 cross-cutting questionnaire that you just completed, you indicated that during the past 2
weeks you (individual receiving care) have been bothered by “feeling nervous, anxious, frightened, worried, or on edge”, “feeling panic
or being frightened”, and/or “avoiding situations that make you anxious” at a mild or greater level of severity. The questions below ask
about these feelings in more detail and especially how often you (individual receiving care) have been bothered by a list of symptoms
during the past 7 days. Please respond to each item by marking (P or x) one box per row.
Clinician
Use
In the past SEVEN (7) DAYS....
Never
Rarely
Sometimes
Often
Always
1.
I felt fearful.
q 1
q2
q3
q4
q5
2.
I felt anxious.
q 1
q2
q3
q4
q5
3.
I felt worried.
q 1
q2
q3
q4
q5
4.
I found it hard to focus on anything
other than my anxiety.
q 1
q2
q3
q4
q5
5.
I felt nervous.
q 1
q2
q3
q4
q5
6.
I felt uneasy.
q 1
q2
q3
q4
q5
7.
I felt tense.
q 1
q2
q3
q4
q5
Total/Partial Raw Score:
Prorated Total Raw Score:
T-Score:
Item
Score
Level 2 cross-cutting scale for anxiety in children – parent filled
Instructions to parent/guardian:
On the DSM-5 Level 1 cross-cutting questionnaire that you just completed, you
indicated that during the past 2 weeks your child receiving care has been bothered by “feeling nervous, anxious, or
scared”, “not being able to stop worrying”, and/or “couldn’t do things he/she wanted to or should have done because
they made him/her feel nervous” at a mild or greater level of severity. The questions below ask about these feelings in
more detail and especially how often your child receiving care has been bothered by a list of symptoms during the past
7 days. Please respond to each item by marking ( or x) one box per row.
In the past SEVEN (7) DAYS, my
child said that he/she …
Clinician
use
Never
1
almost never
2
Sometimes
3
Often
4
Almost always
5
1. Felt like something awful might
happen
2. Felt nervous
3. Felt scared
4. Felt worried
5.
Worried about what could
happen to him/her.
6. Worried when he/she went to
bed at night
7. Got scared really easy.
8. Was afraid of going to school.
9 Worried when he/she was at
home
10. Worried when he/she was
away from home
Total/partial raw score
Prorated total raw score
Item
score
LEVEL 2—Sleep Disturbance—Adult* *PROMIS—Sleep Disturbance—Short Form
Name:
Age:
Sex: q Male q Female
Date:
If the measure is being completed by an informant, what is your relationship with the individual receiving care?
In a typical week, approximately how much time do you spend with the individual receiving care?
hours/week
Instructions to patient: On the DSM-5 Level 1 cross-cutting questionnaire that you just completed, you indicated that during the past
2 weeks you (the individual receiving care) have been bothered by “problems with sleep that affected your sleep quality over all” at a mild or
greater level of severity. The questions below ask about these feelings in more detail and especially how often you (the individual receiving
care) have been bothered by a list of symptoms during the past 7 days. Please respond to each item by marking (P or x) one box per row.
Clinician
Use
In the past SEVEN (7) DAYS....
Not at all
A little bit
Somewhat
Quite a bit
Very much
1. My sleep was restless.
q 1
q2
q3
q4
q5
2. I was satisfied with my sleep.
q 5
q4
q3
q2
q1
3. My sleep was refreshing.
q 5
q4
q3
q2
q1
4. I had difficulty falling asleep.
q 1
q2
q3
q4
q5
In the past SEVEN (7) DAYS....
Never
Often
Always
5. I had trouble staying asleep.
q 1
Rarely
q2
Sometimes
q3
q4
q5
6. I had trouble sleeping.
q 1
q2
q3
q4
q5
7. I got enough sleep.
q 5
q4
q3
q2
q1
Poor
Fair
Good
q4
q3
q2
In the past SEVEN (7) DAYS....
Very Poor
8. My sleep quality was...
q 5
Very good
q1
Total/Partial Raw Score:
Prorated Total Raw Score:
T-Score:
DIMENSIONAL SEVERITY MEASURES
• In addition to a diagnosis, DSM MEASURES
SEVERITY OF MANY DIAGNOSIS
• SEVERITY HAS NEVER BEEN CONSISTENTLY
MEASURED IN DSM UNTIL NOW
– ONE EITHER WAS PSYCHOTIC OR ONE WAS NOT
– THERE WERE NO GRADATIONS
Severity - The DSM uses 2 methods of assessing
severity, depending on the diagnosis..
Method 1 involves using a specific dimensional
measure or scale Called “disorder specific severity
measures”. These can be find on the DSM 5 website
under online assessment measures (DIMENSIONAL
SCALE )
Method 2 involves counting the number of symptoms
and rating severity based on number of symptoms.
For example, ‘mild alcohol use Disorder = 2 – 3
symptoms: moderate alcohol use disorder = 4 – 5
symptoms; severe alcohol use Disorder= presence of 6
or more symptoms (Total number of diagnostic
crtieria)
Disorder-Specific Severity Measures For Adults
Severity Measure for Depression—Adult (Patient Health Questionnaire [PHQ-9])
Severity Measure for Separation Anxiety Disorder—Adult
Severity Measure for Specific Phobia—Adult
Severity Measure for Social Anxiety Disorder (Social Phobia)—Adult
Severity Measure for Panic Disorder—Adult
Severity Measure for Agoraphobia—Adult
Severity Measure for Generalized Anxiety Disorder—Adult
Severity of Posttraumatic Stress Symptoms—Adult (National Stressful Events Survey PTSD Short Scale [NSESS])
Severity of Acute Stress Symptoms—Adult (National Stressful Events Survey Acute Stress Disorder Short Scale [NSESS])
Severity of Dissociative Symptoms—Adult (Brief Dissociative Experiences Scale [DES-B])
For Children Ages 11–17
Severity Measure for Depression—Child Age 11–17 (PHQ-9 modified for Adolescents [PHQ-A]—Adapted)
Severity Measure for Separation Anxiety Disorder—Child Age 11–17
Severity Measure for Specific Phobia—Child Age 11–17
Severity Measure for Social Anxiety Disorder (Social Phobia)—Child Age 11–17
Severity Measure for Panic Disorder—Child Age 11–17
Severity Measure for Agoraphobia—Child Age 11–17
Severity Measure for Generalized Anxiety Disorder—Child Age 11–17
Severity of Posttraumatic Stress Symptoms—Child Age 11–17 (National Stressful Events Survey PTSD Short Scale [NSESS])
Severity of Acute Stress Symptoms—Child Age 11–17 (National Stressful Events Survey Acute Stress Disorder Short Scale
[NSESS])
Severity of Dissociative Symptoms—Child Age 11–17 (Brief Dissociative Experiences Scale [DES-B])
Clinician-Rated
Clinician-Rated Severity of Autism Spectrum and Social Communication Disorders
Clinician-Rated Dimensions of Psychosis Symptom Severity (also available in print book)
Clinician-Rated Severity of Somatic Symptom Disorder
Clinician-Rated Severity of Oppositional Defiant Disorder
Clinician-Rated Severity of Conduct Disorder
Clinician-Rated Severity of Nonsuicidal Self-Injury
This document is
found on page
743 of the DSM.
It allows the
clinician to rate
all of the salient
dimensions
that might be
present in a
disorder on the
schizophrenia
spectrum - IN
TERMS OF
SEVERITY using Likert scale
to rate the
dimensions
DSM 5 criteria for major depression
A. Five or more of the following symptoms of been
present during the same two-week period and
represent a change from previous functioning; at
least one of the symptoms is either depressed mood
or loss of interest or pleasure
1. Depressed mood most of the day, nearly every day as indicated
by subjective reporter observation. Yes or no
2. Marked diminished interest or pleasure in all our almost all
activities. Most of the day, nearly every day. Yes or no
3. Significant weight loss when not dieting or weight gain or
decrease in appetite, nearly every day. Yes or no
4. Insomnia or hypersomnia nearly every day. Yes or no
5. Psychomotor agitation or retardation nearly every day. Yes or
no
6. Fatigue or loss of energy nearly every day. Yes or no
7. Feelings of worthlessness or excessive or inappropriate guilt.
Yes or no
8. Diminished ability to think or concentrate or indecisiveness
nearly every day. Yes or no
9. Recurrent thoughts of death or recurrent suicidal ideation or
suicide attempt Yes or no
B. The symptoms cause clinically significant distress
or impairment Yes or no
C. The episode is not attributable to the
physiological effects of a substance or another
medical condition Yes or no
D. The occurrence of the major depressive disorder
is not better explained by schizoaffective
schizophrenia schizophreniform or anything else on
the schizophrenia spectrum Yes or no
E. There has never been a manic episode or
hypomanic episode Yes or no
Psycho-social HX
MSE
1. Lead with level I
crosscutting symptom
measures to assess all
symptom domains
2. Follow-up with level II
crosscutting measures in
order to capture clinical
nuances and potential
comorbid
3. Move to categories and
check off criteria
4. Assess severity
Adapted from the Patient Health Questionnaire–9 (PHQ-9) depression
Name:
Age:
Sex: Male q Female q Date:
Instructions: Over the last 7 days, how often have you been bothered by any of the following problems?
Clinician
Use
Item
score
Not at all
Several
days
More
than half
the days
Nearly
every
day
1.
Little interest or pleasure in doing things
0
1
2
3
2.
Feeling down, depressed, or hopeless
0
1
2
3
3.
Trouble falling or staying asleep, or sleeping too much
0
1
2
3
4.
Feeling tired or having little energy
0
1
2
3
5.
Poor appetite or overeating
0
1
2
3
6.
Feeling bad about yourself—or that you are a failure or
have let yourself or your family down
0
1
2
3
7.
Trouble concentrating on things, such as reading the newspaper or
watching television
0
1
2
3
8.
Moving or speaking so slowly that other people could have
noticed? Or the opposite—being so fidgety or restless that you have
been moving around a lot more than usual
0
1
2
3
9.
Thoughts that you would be better off dead or of hurting yourself in
some way
0
1
2
3
Total/Partial Raw Score:
Prorated Total Raw Score: (if 1-2 items left unanswered)
Levels of depressive symptoms severity
None
Mild depression
Moderate depression
Moderately severe depression
Severe depression
PHQ-9 Score
0-4
5-9
10-14
15-19
20-27
Method #2 for severity
Alcohol use disorder
A.
Problematic pattern of alcohol use leading to clinically significant impairment or
distress as manifested by at least two of the following occurring within a 12
month period
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
Alcohol taken in larger amount (need more for increased effect)
Persistent desire or efforts to quit Using alcohol
Time spent to obtain, use, recover from effects Of alcohol
Cravings Or urges to use Alcohol
Failure to fulfill significant roles
Continued use Alcohol despite persistent and recurrent problems
Important social/occupational activities are reduced
Recurrent use Of alcohol in physically hazardous situations
Use Of alcohol continues despite knowledge of impact of the problem
Tolerance, as defined by a. Increased amounts needed to achieve intoxication
or b. Diminished effect Of alcohol
11. Withdrawal From alcohol
Severity
Mild = presence of 2-3 symptoms
moderate = presence of four – five symptoms
severe = presence of six or more symptoms
Course specifiers
early remission = after full criteria were l
previously met none of the criteria met
for at least three months but less than 12 (with the exception of craving)
In sustained remission = after full criteria were previously met none exists except craving
during the period of 12 months or more
2. NO MORE GAF
WHODAS
• DSM IV-TR- HAD SOMETHING CALLED THE
GLOBAL ASSESSMENT OF FUNCTIONING
– THE ONLY DIMENSIONAL MEASURE IN THE DSM IV
TR
– USED BY CLINICIAN; COMPLETELY UNRELIABLE
AND NOT VALID
• REPLACED WITH A SCALE THAT HAS
RELIABILITY AND VALIDITY DATA
– THE WORLD HEALTH ORGANIZATION DISABLITY
ASSESSMENT SCALE (WHODAS PP 745-749)
DSM 5 recommends the following
1. Assess symptom severity/severity of
diagnosis-use severity scales
2. Use dimensional scales or standardized
scales whenever possible
3. Assess suicidality, capacity for self harm
or harming others- use separate
assessment protocol
4. Use World Health Organization disability
assessment scale to assess social and selfcare functioning
WHODAS 2.0
• Based on the International Classification of
Functioning, Disability, and Health (ICF)
• Applicable to any health condition
• Reliability and clinical utility established in
DSM 5 Field trials
see pages 745 to 748 in DSM 5
WHODAS Assesses the following six areas
1. Understanding and communicating
2. Getting around
3. Self-care
4. Getting along with people
5. Life activities
6. Participation in society
STANDARDIZED WAY TO MEASURE HEALTH AND DISABILITY ACROSS CULTURES
DOES NOT TARGET SPECIFIC DISEASE, SO CAN BE USED TO ASSESS DISABILITY ACROSS DISEASE
WHODAS 36 ITEM ON NEXT 3 SLIDES (PP745-749 IN DSM)
Domain 1
In the past 30 days, how much difficulty did you
have in:
Cognition
None
Mild
Moderate
Extreme or
cannot do
Severe
D1.1
Concentrating on doing something for ten
minutes?
1
2
3
4
5
D1.2
Remembering to do important things?
1
2
3
4
5
D1.3
Analysing and finding solutions to
problems in day-to-day life?
1
2
3
4
5
D1.4
Learning a new task, for example,
learning how to get to a new place?
1
2
3
4
5
D1.5
Generally understanding what people
say?
1
2
3
4
5
D1.6
Starting and maintaining a
conversation?
1
2
3
4
5
Domain 2
In the past 30 days, how much difficulty did you
have in:
D2.1
Standing for long periods such as 30
minutes?
Mobility
None
Mild
Moderate
Severe
1
2
3
4
Extreme or
cannot do
5
D2.2
Standing up from sitting down?
1
2
3
4
5
D2.3
Moving around inside your home?
1
2
3
4
5
D2.4
Getting out of your home?
1
2
3
4
5
D2.5
Walking a long distance such as a
kilometre [or equivalent]?
1
2
3
4
5
Domain 3
In the past 30 days, how much difficulty did you have
in:
Self-care
None
Mild
Moderate
Severe
Extreme or
cannot do
D3.1
Washing your whole body?
1
2
3
4
5
D3.2
Getting dressed?
1
2
3
4
5
D3.3
Eating?
1
2
3
4
5
D3.4
Staying by yourself for a few days?
1
2
3
4
5
Domain 4
Getting along with people
In the past 30 days, how much difficulty did you have in:
None
Mild
Moderate
Extreme or
cannot do
Severe
D4.1
D4.2
D4.3
Dealing with people you do not know?
Maintaining a friendship?
Getting along with people who are close to you?
1
1
1
2
2
2
3
3
3
4
4
4
5
5
5
D4.4
D4.5
Making new friends?
Sexual activities?
1
1
2
2
3
3
4
4
5
5
Domain 5
LIFE ACTIVITIES
Because of your health condition, in the past 30 days, how much difficulty
did you have in:
None
Mild
Moderate
Severe
Extreme or
cannot do
D5.1
Taking care of your household responsibilities?
1
2
3
4
5
D5.2
Doing your most important household tasks well?
1
2
3
4
5
D5.3
Getting all the household work done that you needed to
do?
Getting your household work done as quickly as needed?
1
2
3
4
5
1
2
3
4
5
D5.4
Domain 5
Because of your health condition, in the past 30 days how much
difficulty did you have in:
D5.5
Your day-to-day work/school?
Doing your most important work/school tasks well?
D5.6
WORK OR SCHOOL ACTIVITIES
None
Mild
1
1
2
2
3
3
4
4
Extreme or
cannot do
5
5
Moderate
Severe
D5.7
Getting all the work done that you need to do?
1
2
3
4
5
D5.8
Getting your work done as quickly as needed?
1
2
3
4
5
D5.9
Have you had to work at a lower level because of a health condition?
D5.10
Did you earn less money as the result of a health condition?
No
Yes
No
Yes
1
2
1
2
Domain 6
In the past 30 days:
Participation
None
Mild
Moderate
Severe
Extreme or cannot do
D6.1
How much of a problem did you have joining in community
activities (for example, festivities, religious or other activities)
in the same way as anyone else can?
1
2
3
4
5
D6.2
How much of a problem did you have because of barriers or
hindrances in the world around you?
1
2
3
4
5
D6.3
How much of a problem did you have living with dignity
because of the attitudes and actions of others?
1
2
3
4
5
D6.4
How much time did you spend on your health condition or its
consequences?
1
2
3
4
5
D6.5
How much have you been emotionally
affected by your health condition?
1
2
3
4
5
D6.6
How much has your health been a drain on the financial
resources of you or
your family?
1
2
3
4
5
D6.7
How much of a problem did your family have because of your
health problems?
1
2
3
4
5
D6.8
How much of a problem did you have in doing things by yourself
for relaxation or pleasure?
1
2
3
4
5
• If WHODAS is used, place
results at the very end of
assessment, after psychosocial
stressors
3. How to chart without axes
DSM-5 has moved to a nonaxial documentation of diagnosis (formerly
Axes I, II, and III), with separate notations for important psychosocial
and contextual factors (formerly Axis IV) and disability (formerly Axis V)
Taken from Northstar behavioral health system
http://www.northstarbehavioral.com/Overview%20of%20DSM%205%20changes%20HO%20Ver
sion%20for%20Web%208-13-13.pdf
Axis IV - psychosocial and environmental factors - are now
covered through an expanded set of V codes. V codes allow
clinicians to indicate other conditions that may be a focus
of clinical attention or affect diagnosis, course, prognosis or
treatment of a mental disorder
Axis V - CGAS and GAF - are replaced by separate measures
of symptoms severity and disability for individual disorders.
Change to the World Health Organization Disability
Assessment Schedule (WHO DAS 2.0)
Taken from Northstar behavioral health system
http://www.northstarbehavioral.com/Overview%20of%20DSM%205%20changes%20HO
%20Version%20for%20Web%208-13-13.pdf
All diagnoses are considered primary
diagnosis
• All diagnoses are listed consecutively (no distinction
between diagnosis previously listed on axis I, axis II
or axis III)
• List diagnosis that is the reason for visit 1st
Primary-reason for visit, 296.33, major depressive disorder, recurrent, severe.
Primary- Medical condition; Parkinson’s disease, moderate
Primary-305.00 alcohol use disorder, mild.
Primary -v15.81 non-adherence to medical treatment. (Patient continues to drink
while on antidepressants and does not take antidepressants regularly.)
• If the principal diagnosis that is a reason for visit is a
mental disorder caused by a medical condition, the
medical condition is listed 1st
Primary-Parkinson's disease-moderate with tremors and newly developed
postural instability (scored 3 on Hoehn and Yahr)
Primary-Reason for visit, 296.22; major depressive disorder, single
episode, moderate
Case example – for listing of DX
John is a 65-year-old white male who is morbidly obese and has been a smoker for 40 years. He quit
smoking 5 years ago after being diagnosed with Parkinson's disease. Over the last 5 years, John's ability
to perform physical activity, has progressively deteriorated. Although John reports bouts of depression,
beginning in adolescence and continuing throughout his adult life, he was not diagnosed with major
depressive disorder until 4 years ago (one year after the diagnosis of Parkinson’s). Since that time, he has
been on several antidepressant medications, most recently Remeron. John reports that he has been a
regular drinker since his days in college. Although he denies it, his alcohol use, according to his wife, has
increased since his diagnosis of Parkinsons. However, upon evaluation both john and his wife agree that
he drinks no more than 3 times per week – usually a six pack. Although John has been advised to
discontinue drinking, he has not done so. According to both John and his wife. He misses his medication
anywhere from 1 to 3 times per week.
About 3 months ago john fell while at home. His wife at first thought it was a result of his drinking.
According to John he noticed that he was having more difficulty standing and walking while maintaining
his A recent neurological consult indicates that John does NOT have any neurological deficits that are out
of normal range for his age but has developed postural instability consistent with a progression of
Parkinson’s
Despite advice to the contrary, John has become progressively more sedentary and has discontinued all
forms of exercise. About 1 month ago, John's employers required that John start working part-time and
consider filing for early Social Security. According to them, John's ability to work has diminished. They
too noted that he was having difficulty walking. For the last 3 weeks, John has met all of the criteria for a
severe episode of major depression.
Primary diagnosis
Primary-reason for visit, 296.33, major depressive disorder, recurrent, severe.
Primary- Medical condition; Parkinson’s disease-recently upgraded to moderate
Primary-305.00 alcohol use disorder, mild.
Primary -v15.81 non-adherence to medical treatment. Patient continues to drink while on antidepressants
take antidepressants irregularly
V codes -psychosocial stressors
Greatly expanded in the DSM 5
• V codes (codes V01–V91) are used to describe encounters
with circumstances other than formal mental disorder
diagnoses disease or injury.
• V codes are taken from the ICD. Their conditions and
problems that may be the focus of clinical attention or
that otherwise might affect the diagnosis, course,
prognosis or treatment of the mental disorder.
• First Incorporated in the DSM-III
• Will become Z codes in ICD 10 -October 2014 (these are
listed in DSM 5)
Use V codes To indicate
V codes (codes V01–V91) are used to describe encounters with
circumstances other than formal mental disorder diagnoses
disease or injury
V codes are taken from the ICD. Their conditions and problems
that may be the focus of clinical attention or that otherwise
might affect the diagnosis, course, prognosis or treatment of the
mental disorder.
First Incorporated in the DSM-III
Will become Z codes in ICD 10 -October 2014 (these are listed in
DSM 5)
Code in the following ways
1. As a Focus or need for clinical attention
= Place code as a comorbid diagnosis
or as another primary diagnosis
2. As a Psychosocial/ Environmental
stressor = Place code as A stressor at
the end of all of the diagnoses
John is a 65-year-old white male who is morbidly obese and has been a smoker for 40 years. He quit 5 years ago
after being diagnosed with Parkinson's disease. Over the last 5 years, John's ability to perform physical activity,
has progressively deteriorated. Although John reports bouts of depression, beginning in adolescence and
continuing throughout his adult life, he was not diagnosed with major depressive disorder until 4 years ago (one
year after the diagnosis of Parkinson’s). Since that time, he is been on several antidepressant medications, most
recently Remeron. John reports that he has been a regular drinker since his days in college. Although he denies it,
his alcohol use, according to his wife, has increased since his diagnosis of Parkinsons. However, upon evaluation
both john and his wife agree that he drinks no more than 3 times per week – usually a six pack. Although John has
been advised to discontinue drinking, he has not done so. And according to both John and his wife. He misses his
medication anywhere from 1 to 3 times per week.
About 3 months ago john fell while at home. His wife at first thought it was a result of his drinking. According to
John he noticed that he was having more difficulty standing and walking while maintaining his A recent
neurological consult indicates that John does NOT have any neurological deficits that are out of normal range for
his age but has developed postural instability consistent with a progression of Parkinson’s
Despite advice to the contrary, John has become progressively more sedentary and has discontinued all forms of
exercise. About 1 month ago, John's employers required that John start working part-time and consider filing for
early Social Security. According to them, John's ability to work has diminished. They too noted that he was having
difficulty walking. For the last 3 weeks, John has met all of the criteria for a severe episode of major depression.
Primary diagnosis
Primary-reason for visit, 296.33, major depressive disorder, recurrent, severe.
Primary- Medical condition; Chronic Obstructive Pulmonary Disease, moderate
Primary-305.00 alcohol use disorder, mild.
Primary -v15.81 non-adherence to medical treatment. Patient continues to drink while on antidepressants
take antidepressants irregularly
Psychosocial stressors and factors that might affect treatment
v278.00 – Obesity
v69.9 - Problems related to lifestyle. John's diet and his progressive sedentary behavior, along with his
nonadherence and progressive isolation are contributing factors to his primary diagnoses
v62.29 - Other problems related to employment. John has recently had his work hours cut in half
WHODAS raw score = 98: domain averages:
Cognition = 1none
mobility = 4 severe
self-care = 2 mild
getting along with others = 2 mild
Life activities = 2.5 mild- moderate
work activities = 3, moderate
participation = 3.5moderate- severe
4. A cultural framework:
The DSM and cultural formulation
• DSM calls for systematic cultural assessment in these areas
1.
2.
3.
4.
5.
Cultural identity of the individual-describe reference group that
might influence his or her relationships resources, developmental,
and current challenges
Cultural conceptualization of distress-describe constructs that
influence how the individual experiences understands and
communicates symptoms or problems to others
Psychosocial stressors and cultural features of vulnerability and
resilience-identify key stressors and supports in the individual social
environment, role of religion, family and other social.
Cultural features or influencing factors of the relationship between
the individual and clinician.-Identify differences that may cause
difficulties in communication and may influence diagnosis
Overall cultural assessment-summarize the implications of the
components of the cultural formulation, identified earlier. (DSM 5,
pp749-750)
DSM and the cultural formulation
interview
• 16 questions used to obtain information about
the impact of culture on key aspects of a person's
clinical presentation
• Assesses 4 areas
1. Cultural definition of the problem (Q1 – 3)
2. Cultural perceptions of cause, context and support
(Q4 – 10)
3. Culture of factors affecting self coping and past help
seeking (Q 11 – 13
4. Cultural factors affecting current help seeking (Q 14
– 16)
This page and the 3 following are reprinted from the DSM 5
website at psychiatry.org. Please see provisions for copying at
the bottom of the slides
5. Overall organization of disorders
DSM categories organized over developmental lifespan
Initial occurrence
Younger
Neuro
develop
mental
Bipolar
Schizophrenia
Older
Anxiety
Depressive
Trauma
related
Obsessivecompulsive
and related
Somatic
symptom
related
Dissociative
Elimination
disorders
Feeding and
eating
disorders
Sexual
dysfunctions
Sleep wake
disorders
Gender
dysphoria
Disruptive
, impulse
control
disorders
Neurocognitive
disorders
Substance
related and
addictive
disorders
Personality
disorder
Paraphilia
disorders
Others
The progression from younger to older in the DSM is general and there are
specific disorders such as some early childhood feeding disorders that
clearly occur later
DSM categories organized using
empirically validated common factors
Internalizing
Symptom
factors
Neural
commonalities
Neuro
develop
mental
Bipolar
Schizophrenia
Anxiety
Depressive
Trauma
related
Obsessivecompulsive
and related
Externalizing
Symptom
factors
Physiological
Symptom
factors
Somatic
symptom
related
Dissociative
Elimination
disorders
Feeding and
eating
disorders
Sexual
dysfunctions
Sleep wake
disorders
Gender
dysphoria
Disruptive
, impulse
control
disorders
Neurocognitive
disorders
Substance
related and
addictive
disorders
Personality
disorder
Paraphilia
disorders
Others
Bio-genetic
similar
factors
These distinctions have some strong validation from recent neuro-scientific
and genetic research
6. Highlight of specific changes in diagnosis
Gone
• Disorders usually evident in infancy, childhood and adolescence.
• Factitious disorders and malingering
• adjustment disorders (now included in trauma and stress-related
disorders)
• NOS Diagnosis for all categories
Added
• neurodevelopmental disorders
• obsessive-compulsive and related disorders (moved out of anxiety)
• trauma and stress-related disorders (moved out of anxiety)
• Disruptive, impulse control, and conduct related disorders
• "Specified" and “Unspecified" disorder for all diagnoses
• "Suicide risk" is now specified for 25 diagnosis
Changed
• Delirium, dementia and cognitive disorders = neurocognitive
disorders
• psychotic disorders = schizophrenia spectrum and other psychotic
disorders
• mood disorders = bipolar and related disorders & depressive
disorders
• somatoform disorders = somatic symptom and related disorders
Neuro developmental disorders
1. The term "mental retardation" has been changed to intellectual disability
2. The term "phonological disorders" has been changed to "communication disorders".
1. A new diagnosis of social/pragmatic communication disorder has been added here
2. childhood onset fluency disorder new name for stuttering
3. Speech sound disorder is new name for phonological disorder
3. Autism spectrum disorder is the new term and DSM 5 which consolidates Aspergers
disorder, autism, and pervasive developmental disorder. Severity measures are included
4. Several changes have been made to the diagnostic criteria for attention deficit
hyperactive disorder
5. Specific learning disorder combines DSM-IV diagnosis of reading disorder mathematics
disorder disorder of written expression and learning disorder NOS
6. Language disorder combines expressive and mixed receptive expressive into one
7. Symptom onset for ADHD was extended to before age 12; Subtypes eliminated and
replaced by specifiers; now allowed to make a comorbid diagnosis with ASD; Symptom
criteria for adults reduced to 5 instead of 6
Schizophrenia spectrum and other
psychotic disorders
1.
2.
3.
4.
5.
6.
7.
The spectrum seems to emphasize degrees of psychosis
Change in criteria for schizophrenia now requires at least one
criteria to be either a. Delusions, b. Hallucinations or c.
Disorganized speech
Subtypes of schizophrenia were eliminated
Dimensional measures of symptom severity are now included
Schizoaffective disorder has been reconceptualized
Delusional disorder no longer requires the presence of “nonbizarre" in delusions. There is now specifier for bizarre delusions.
Schizotypal personality disorder is now considered part of the
spectrum
Bipolar and related disorders
• Diagnosis must now include both changes in
mood and changes in activity/energy level
• Some particular conditions can now be
diagnosed under "other specified bipolar and
related disorders“
• An "anxiety" specifier has now been included
• Attempts made to clarify definition of
'hypomania". However it was not successful
Depressive disorders
• New diagnosis included = "disruptive mood
dysregulation disorder”-use for children up to age
18
• New diagnosis included = "premenstrual
dysphoric disorder“
• What used to be called dysthymic disorder is now
"persistent depressive disorder“
• Bereavement is no longer excluded – used to be
an exclusion for 2 months
• New specifiers such as mixed features. And
anxious distress
Obsessive-compulsive and related
disorders
•
•
•
•
A completely new diagnostic grouping category
Hoarding disorder-new diagnosis
Excoriation (skin picking) disorder-new diagnosis
Substance induced obsessive-compulsive
disorder-new diagnosis
• Trichotillomania now called hair pulling disorder
• Tic specifier has been added
• Muscle dysphoria is now a specifier within body
dysmorphic disorder
Trauma and stress related disorders
• For diagnosis of acute stress disorder, it must
be specified whether the traumatic events
were experienced directly or indirectly
• Adjustment disorders (a separate class in the
DSM-IV) are included here as various types of
responses to stress
• Major changes in the criteria for the diagnosis
of PTSD
Anxiety disorders
• Obsessive-compulsive disorder has been moved out of
this category
• PTSD has been moved out of this category
• Acute stress disorder has been moved out of this
category
• Changes in criteria for specific phobia and social anxiety
have been made
• Panic attacks can now be used as a specifier within any
other disorder in the DSM
• Separation anxiety disorder has been moved to this
group
• Selective mutism has been moved to this group
Dissociative disorders
• Depersonalization disorder has been relabeled
“Depersonalization/Derealization disorder“
• Dissociative fugue is no longer a separate
diagnosis but is now specifier within the
diagnosis of "dissociative amnesia“
• Changes in criteria for the diagnosis of
"dissociative identity disorder"
Somatic symptom and related
disorders
• This is a new name for what was previously called
"somatoform disorders“
• The number of diagnoses in this category has
been reduced. The diagnoses of somatization
disorder, hypochondriasis, pain disorder and
undifferentiated somatoform disorder have all
been removed
• "Illness anxiety disorder" has been an added
diagnosis and replaces hypochondriasis
• Factitious disorder is now included in this group
Feeding and eating disorders
• "Binge eating disorder' is now included as a
separate diagnosis
• also includes a number of diagnosis that were
previously included in a DSM-IV TR in the
chapter "disorders usually 1st diagnosed
during infancy childhood and adolescence“.
– Pica and rumination disorder are 2 examples
Elimination disorders
• Originally classified in chapters on childhood and
infancy. Now have separate classification
Sleep wake disorders
• Primary insomnia renamed "insomnia disorder«
• Narcolepsy now distinguished from other forms of
hypersomnia
• Breathing related sleep disorders have been broken
into 3 separate diagnoses
• Rapid eye movement disorder and restless leg
syndrome are now independent diagnoses within this
category
Sexual dysfunctions
• Some gender related sexual dysfunctions have
been outed
• Now only 2 subtypes-acquired versus lifelong and
generalized versus situational
Gender dysphoria
• New diagnostic class and the DSM 5
• Include separate classifications for children
adolescents and adults
• The construct of gender has replaced the
construct of sex
Disruptive, impulse control and
conduct disorders
• New diagnostic grouping and DSM 5
• Combines a group of disorders previously included
in disorders of infancy and childhood such as
conduct disorder oppositional defiant disorder with
a group previously known as impulse control
disorders not otherwise classified
• Oppositional defiant disorder now has 3 subtypes
• Intermittent explosive disorder no longer requires
physical violence but can include verbal aggression
Substance related and addictive
disorders
• The distinctions between substance abuse and
substance dependence are no longer made
– Now includes criteria for intoxication, withdrawal
and substance induced disorders
• Now includes gambling disorder
• Cannabis and caffeine withdrawal are now
new disorders
Neuro-cognitive disorders
• New diagnostic group
• Dementia and amnestic disorder are included
in this new group
• Mild NCD is a new diagnosis
Personality disorders
Nothing changes
DSM 5 promised major changes in
criteria
• Promised dimensional focus
• Promised reduction in number of personaliity
disorders to five
• Changes did not occur
• Dimensional focus for personality disorders
was moved to section 3
Primary Criteria in DSM 5
(Unchanged from DSM-IV TR)
A.
Enduring pattern of inner experience & behavior that
deviates markedly from expectations of the culture. This
pattern is manifested in 2 or more of the following areas
A.
B.
C.
D.
B.
C.
D.
Cognition;
Affect;
Interpersonal;
Impulse control
Inflexible & pervasive across situation
Distress or impairment in social, occupational
interpersonal..…
Long-standing (back to adolescence or early adulthood)
Dimensional classification of
personality disorders
• Authors of DSM 5 had planned to use
dimensional measures to diagnose personality
disorders
• They plan to reduce personality disorders
from 10 to 5
• This changed in a closed-door meeting
• Dimensional measures are now in section 3
Proposed changes in assessment of PDs
Two
broad
dimensions
Overall
personality
functioning
self
Identity
Interpersonal
Self
direction
Empathy
5 Broad
Pathological
Trait Domains
Negative
affectivity
Intimacy
Detachment
Antagonism
Disinhibition
Psychoticism