Unpacking Health System Performance for MCH and FP
advertisement
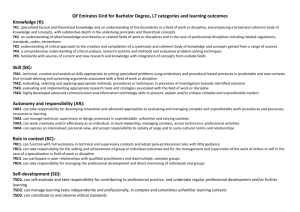
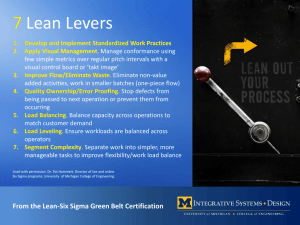
Health System Strengthening for Greater Health Impact We all say we do it and do it well, but what is it? How strong is the evidence base? Dan Kraushaar Management Sciences for Health We now have more and better “what”, “why” and “how much” • • • • • Understanding of the problem Proximal and distal of causes Evidence on intervention efficacy and effectiveness Improved modeling Much improved normative guidance Fragmented HSS efforts have created evidence on how to improve inputs and processes Inputs Leadership & governance Financing Information Health workforce Delivery Medical products, vaccines and technologies processes outputs outcomes impact The evidence base on system strengthening for health impact is weak • The black box of health system strengthening for health impact remains a black box. • Weak health systems remains the primary barrier • Lack of an agreed upon conceptual framework • Lack of appropriate evaluation designs and limited scientific method applied to HSS efforts • Consequently limited evidence of what works, why and under what conditions Two promising practices 1. Causal pathway analysis as a means of linking health system strengthening interventions to health outcomes. 2. Systematic application of key policy and managerial levers applied against concretely defined system bottlenecks. Most effective programs have defined HSS efforts based on causal pathway analysis in some way or another System requirements Evidence based interventions & coverage levels Problems and causes Measurable goal Allowing for system strengthening, program design and management along that defined causal path. HSS against specific health system bottlenecks Right inputs & processes Higher coverage Reduced problems, goals attained That, coupled with use of five policy and management levers for improved system performance • Five key features of the health system which can be manipulated by policy makers and managers. • When systematically applied have shown to influence the structure and function of the health system. • They are a promising approach to improving health system performance for greater health impact. *Modified from Hsiao, William C. (2009). Inside the Black Box of Health Systems: What Are the Policy Control Knobs? What are those levers? Health system bottlenecks 1. Changing how resources are mobilized and allocated and how risks are pooled 2. Changing the organization of financing and the appropriate involvement of public and private sectors 3. Changing the payment and incentive structures for providers and consumers and modifying costs of inputs Applied against system bottlenecks can improve system performance Health Information Health Financing Medical Products, Vaccine, and Technologies 4. Use of the coercive power of government through policy & regulation 5. Influencing beliefs, preferences and behavior of people, organizations and providers Leadership and Governance Health Workforce Health Services and Delivery Source: Roberts, Marc, William Hsiao, Peter Berman, and Michael Reich. Getting Health Reform Right - A Guide to Improving Performance and Equity. New York: Oxford University Press, 2008. Oxford Scholarship Online. Oxford University Press. Convincing evidence • Retrospective analysis of effective programs • Bill Hsiao, Harvard: 22 country analyses • Specific examples of country programs • Multiple examples the past few days Thailand national FP program Lever Policy and management action 1. Mobilize, allocate and manage resources 1. Massive and preferential increase in FP funding sustained by gov’t over time. Subsidies to private sector 2. Organization, roles of public and private sectors 2. Expanded community level gov’t facilities. Encouraged private provision. Created midwifery cadre and established midwifery schools for community FP delivery. Expanded FP logistics. Integrated FP into MCH system. Encouraged private sector. 3. Changing the payment and incentives and costs 3. Free services. FP currently covered by 30Bht scheme? 4. Policy and regulation 4. Policy allowed for private sector innovation. Allowed research on FP methods. 5. Influencing beliefs, preferences and behavior 5. Studied KAP of providers and consumers. Identified resistance points. Educated and trained all levels of providers. Multi media campaign. HSS in Jordan (Dr. Hamsa’s presentation) Lever Policy and management action 1. Mobilize, allocate and manage resources 1. Emergency financial allocations for mag sulfate. Cost analysis. Preferential financing. 2. Organization, roles of public and private sectors 2. Improved logistics and supply. Altered purchasing processes. Improved monitoring and supervision. Creation of motherhood committees. Improved program execution. 3. Changing the payment and incentives and costs 3. Improved accountability through use of motherhood committees. 4. Policy and regulation 4. Improved policies on use of mag. Sulfate. Clinical guidelines. 5. Influencing beliefs, preferences and behavior 5. Competency based training. Use of expert clinicians. Use of data and access to global evidence to influence provider attitudes and behavior. Self directed learning. Thinking Causally and application of policy levers: What are the benefits? 1. Evidence based. 2. Justifies multiple yet calculated policy and managerial actions based on predicted outcomes in a way that is empirically testable. 3. Defines policy and managerial tools for changing system performance. 4. Identifies the vital few interventions and the critical path to impact. 5. Helps identify the most appropriate indicators along that critical path. 6. Helps policy makers and managers focus on outcomes and impact vs inputs and processes using the 5 levers for HSS. What needs to be done? • More systematic application of causal pathway analysis. • Greater attention evidence • More rigorous analysis of health system bottlenecks based on causal analysis. • More systematic application of policy and management levers. • Creation of empirical evidence through more systematic evaluations to determine effectiveness of this approach