Anatomy of the Skin
advertisement

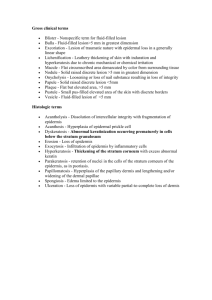
Anatomy of the Skin Rich Callahan MSPA, PA-C ICM I Summer 2009 Before Pathophysiology Comes Anatomy • One of the keys to your knowledge of skin disease is understanding the anatomy of the skin and the particular way a given skin disease affects it. • Anatomy of skin also important during dermatologic procedures like skin biopsy, excisions and ED&C. Skin Anatomy – Basic Overview • Skin essentially composed of 3 layers: epidermis, dermis and subcutis (subcutaneous tissue.) • Epidermis is outermost layer – primarily functional and protective. Subdivided into five layers which migrate upwards and whose purpose is ultimately to form the end layer, or stratum corneum – the outer layer of dead cells that protects us from our environment. Process is called keratinization. The first function of skin is physical protection from the environment. Protection From: • UV radiation • Physical trauma • Liquids (there is a reason we’re waterproof) • Dehydration • Sudden temperature shifts • Microbes First line of defense is the stratum corneum, which is primarily composed of laminated keratin. Definition of Keratin (From Taber’s Medical Dictionary) • “A family of durable protein polymers that are found only in epithelial cells. They provide structural strength to skin, hair and nails. The fibrous protein is produced by keratinocytes.” • Thoroughly understanding the process of keratinization which takes place in the epidermis will unlock answers for many skin diseases because so many of them are disorders of it. Keratin • Comes from the Greek word “keras” for horn. • The outer layer of epidermis, the stratum corneum, gets its name from the Latin word for horn. • My first question was: Where were the people who make up these names seeing a horn? Perhaps it is because the phenomenon of cutaneous horn is the most overt keratinizing process • Multiple underlying pathologies can cause a cutaneous horn: • Verruca vulgaris (common wart) • Actinic Keratosis (AK) • Squamous Cell Carcinoma (SCC) • Seborrheic Keratosis (SK) • Psoriasis • Sometimes no underlying pathology is found Layers of the Epidermis: From Inside to Outside Basal (bottom) layer: A single layer of cells arranged like columns – which divide and turn into the… • Spinous layer (stratum spinosum)whose cells, keratinocytes, begin to form keratin, an insoluble protein critical in later stages. • Granular layer (str. Granulosum) is where cells flatten out and stretch into the • Stratum lucidum and eventually die to form the • Stratum corneum. Old school dermatologists called this the “horny layer” (heh, heh.) Composed of laminated keratin. The “Horny Layer” huh? That term has largely been dropped in dermatology but is getting plenty of utilization elsewhere… Dermis – Divided into 2 layers from top to bottom • Superficial layer is the papillary dermis, a thin layer primarily of collagen fibers. • Arranged in domeshaped inclusions jutting into base of, and feeding small blood vessels into, the epidermis above. • Deep layer is Reticular dermis – composed of thickly layered collagen fibers. • Contains numerous small vessels, cutaneous nerves and apocrine glands. Subcutis – The Deepest Layer of skin (AKA superficial fascia or hypodermis) • A layer of fat loosely marbled with connective tissue and the deeper parts of apocrine glands. • Important route for small to medium-sized blood vessels, sensory and autonomic nerves, lymphatics. • Deep to this is the deep fascia then skeletal muscle.