Introduction to the Integumentary System
advertisement
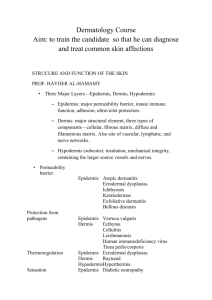
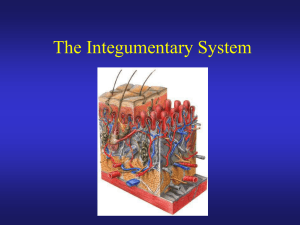
THE INTEGUMENTARY SYSTEM Our skin The components of the integumentary system… 1. 2. Skin – a.k.a. the integument OR cutaneous membrane Accessory organs Sweat glands Oil glands Hairs Nails Without our skin, we would quickly fall prey to bacteria and perish from water and heat loss!!! A little more information about our skin… The skin ordinarily receives very little respect from its inhabitants, but architecturally it is a marvel Some of its uniqueness includes: It covers the entire body It has a surface area of 1.5 – 2.0 m2 Weighs ~4 kg (9 lbs) Accounts for about 7% of the total body weight Consists of ~1/2 million cells that are constantly dying and being replaced It is pliable yet tough The major functions of the skin 1. 2. Protection – the skin covers and protects underlying tissue and organs from impacts, chemicals, and infections, while preventing the loss of body fluids Temperature maintenance – the skin maintains normal body temperature by regulating heat gain or loss to the environment The major functions of the skin con’t 3. 4. Storage of nutrients – the deeper portions of the dermis typically contains a large reserve of lipids in the form of adipose tissue Sensory reception – receptors in the integument detect touch, press, pain, and temperature stimuli and relay that information to the nervous system The major functions of the skin con’t… 5. Excretion and secretion – the integument excretes salt, water, and organic wastes (sweat) and produces milk (a specialized exocrine secretion) Bell Ringer… 1. 2. Why is temperature regulation so important for the body How does our skin protect us – there is more than one way The skin consists of two distinct regions: The epidermis – the superficial epithelium The dermis – underlying dense connective tissue The subcutaneous tissue just below the skin is known as the hypodermis or superficial fascia but strictly speaking, it is not considered part of the skin – it attaches to deeper structures such as muscles or bones The epidermis… The epidermis is composed entirely of stratified squamous epithelium in 5 zones called strata The epidermis is avascular - no blood supply Most cells of the epidermis are keratinocytes – produce keratin, a fibrous protein that makes the epidermis a tough protective layer The strata of the epidermis… 1. 2. 3. 4. 5. There are 5 strata zones – listed from inside to outside Stratum basale – contain epidermal pegs to help from this layer from slipping Stratum spinosum Stratum granulosum Stratum lucidum – found only in hairless area such as our palms and soles of feet Stratum corneum Stratum basale… Deepest cell layer of the epidermis Lies closest to the dermis, separated by basement membrane Contains the only epidermal cells that receive adequate nourishment via diffusion from the connective tissue Constantly undergoing cell division, producing millions of new cells daily, which make their way up to the superficial layer of the skin Life cycle of a skin cell produced in the basale layer… As the cell moves away from the basale layer, it moves through the other layers of the skin, picking up more and more keratin along the way It eventually reaches the outermost strata – stratum corneum, where it dies and is eventually shed We have totally “new” epidermis every 25 to 45 days Keratinization… The cell membranes of older skin cells (the ones nearer the surface) thicken and develop many desmosomes that fasten them to each other While this is happening, the cells begin to harden due to strands of tough, fibrous, waterproof keratin proteins being synthesized and stored within the cell (keratinization) Stratum Spinosum Called this because the keratinocytes in this layer appear “spiny” Scattered among the keratinocytes are melanin granules and Langerhans’ cells, which are most abundant in this layer Melanin granules – give skin its color and protects us from UV radiation Langerhans’ cells – help in immune responses Stratum Granulosum Consists of 3 – 5 layers where the keratinocytes appearance changes drastically They become flatten and fill with waterproofing lamellated granules All cells above this layer are to far from the capillaries and therefore die Stratum corneum… The outermost layer of skin composed of dead, completely keratinized cells It is 20 – 30 cells layer thick and accounts for ~ ¾ of the epidermal thickness Keratin is an exceptionally tough protein – its abundance allows this layer to provide a durable “overcoat” for the body, which protects deeper cells from the hostile environment and water loss This layer rubs and flakes off slowly but is steadily replaced by cell produced by the stratum basale Bell Ringer… List the layers of the epidermis in order from deepest to most superficial What layer is only seen in the palms of our hands and the soles of our feet? The dermis… The layer just below the basement membrane of the epidermis The boundary between the dermis and epidermis is usually uneven This is because the epidermis has ridges projecting inward and the dermis has conical dermal papillae passing into the spaces between the ridges, prevents the dermis from slipping laterally The dermis… The dermis binds the epidermis to the underlying tissues It is largely composed of irregular dense connective tissue that includes tough collagenous fibers and elastic fibers in a gel-like substance These fibers give the skin toughness and elasticity On average, the dermis is 1.0 – 2.0 mm thick, it may be as thin as 0.5 mm or less on the eyelids or as thick as 3.0 mm on our soles The dermis… Contains smooth muscle fibers, such as the arrector pili muscle which causes hair to stand on end Nerve cell processes are scattered through out the dermis, which pick up on sensations from the outer environment It also contains blood vessels, hair follicles, sebaceous glands and sweat glands Medicine delivery through our skin… There are several ways medication can be administered through our skin Intradermal injections 1. Injected within the skin Subcutaneous injections 2. Injected through a hollow needle into the subcutaneous layer a.k.a hypodermic injections Transdermal patches 3. The patch is attached to the skin where the medication diffuses through the epidermis and dermis entering the capillaries Review… What are the 5 functions of our skin? How would you distinguish a mucous and a serous membrane? Where is the subcutaneous layer located? Is it part of the skin?