Benign diseases of the vulva, vagina and cervix
advertisement

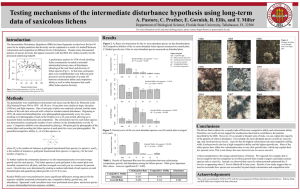
Benign diseases of the vulva, vagina and cervix The vulva • Is the part of the female genital tract located between the genitocrural folds laterally, the mons pubis anteriorly, and the anus posteriorly. • Embryologically, it is the result of the junction of the cloacal endoderm, urogenital ectoderm, and paramesonephric mesodermal layers. • This hollow structure contains – – – – – – – – – LABIA MAJORA LABIA MINORA CLITORIS VESTIBULE URINARY MEATUS VAGINAL ORIFICE HYMEN BARTHOLIN GLANDS SKENE DUCTS. The vulva • Different epithelia, from keratinized squamous epithelium to squamous mucosa, cover the vulva. • The labia minora are rich with sebaceous glands but have few sweat glands and no hair follicles. • The epithelium of the vestibule is neither pigmented nor keratinized and contains eccrine glands. BENIGN LESIONS OF THE VULVA • According to the International Society for the Study of Vulvar Disease (ISSVD) in 1989: – Inflammatory diseases. – Blistering diseases. – Pigmentary changes. – Benign tumors, hamartomas and cysts – Congenital malformations. Inflammatory diseases 1. Lichen sclerosus 2. Squamous cell hyperplasia (+/- atypia) 3. Lichen simplex chronicus (localized neurodermatitis) 4. Primary irritant dermatitis 5. Intertrigo 6. Allergic contact dermatitis 7. Fixed drug eruption 8. Erythema multiforme 9. Toxic epidermal necrolysis 10.Atopic dermatitis 11.Seborrheic dermatitis 12.Psoriasis 13.Reiter disease 14.Lichen planus 15.Lupus erythematosus 16.Darier disease 17.Aphthosis and Behçet disease 18.Pyoderma gangrenosum 19.Crohn disease 20.Hidradenitis suppurativa 21.Fox-Fordyce disease 22.Plasma cell vulvitis 23.Vulvar vestibulitis syndrome Blistering diseases 1. Familial benign chronic pemphigus (Hailey-Hailey disease) 2. Bullous pemphigoid 3. Cicatricial pemphigoid 4. Pemphigus vulgaris 5. Erythema multiforme 6. Epidermolysis bullosa Pigmentary changes 1. Acanthosis nigricans 2. Lentigo 3. Melanocytic nevus 4. Postinflammatory hyperpigmentation 5. Postinflammatory hypopigmentation 6. Vitiligo Benign tumors, hamartomas, and cysts 1. Bartholin cysts 8. Hidradenoma 2. Epidermal inclusion cyst (Dermoid cyst) 9. Lipoma 3. Endometriosis 10. Chronic Inflammatory swellings 4. Hydrocele of the canal of Nuck 11. Hemangioma 5. Skene duct cyst 12. Lymphangioma 6. Seborrheic keratosis 13. Angiokeratoma 7. Acrochordon (fibroepithelial polyp) 14. Pyogenic granuloma 8. Fibroma, fibromyoma, and dermatofibroma 15. Sebaceous gland hyperplasia 16. Papillomatosis BENIGN LESIONS OF THE VULVA • BARTHOLIN’s CYST • ATROPHIC LICHEN (LICHEN SCLEROSUS ET ATROPHICUS) • SQUAMOUS HYPERPLASIA • LICHEN SIMPLEX CHRONICUS • HIDRADENOMA PAPILLIFERUM Bartholin’s Cyst/Abscess • Medial to labia minor • Blockage of duct following infection – N. gonorrhea – Staphylococci – Anaerobes • Thomas Bartholin • Danish professor • In 1652 he gave the first full description of the human lymphatic system. Marsupalization lichen What is lichen? A fungus, usually of the class Ascomycetes, that grows symbiotically with algae, resulting in a composite organism that characteristically forms a crustlike or branching growth on rocks or tree trunks. In pathology…. Any of various skin diseases characterized by patchy eruptions of small, firm papules. Lichen Sclerosus et Atrophicus • Most patients are post-menopausal women • Stenosis of the introitus develops Lichen Sclerosus et Atrophicus Note the white, parchment-like or plaque-like lesion Lichen Sclerosus et Atrophicus • During early stages the patient may not have symptoms. • Some patients develop intractable pruritus • Burning and pain are less likely manifestations. • Figure-of-8 or keyhole configuration. • In late stages normal architecture may be lost – atrophy of the labia minora, constriction of the vaginal orifice (kraurosis), synechiae, ecchymoses, fissures. • Squamous cell carcinoma develops in 3-6% cases Lichen Sclerosus et Atrophicus • Thinning of the surface epithelium with some hyperkeratosis. Lichen Sclerosus et Atrophicus • Etiology – Unknown. A higher prevalence of the disease in postmenopausal women suggests hormonal factors, but this has not been confirmed. – Studies identifying an infection are inconclusive – Weakly linked to autoimmune diseases and genetic factors – Local factors (eg, trauma, friction, chronic infection and irritation) – Recurrence near vulvectomy scars has been observed. Lichen Sclerosus et Atrophicus • Treatment – Potent topical corticosteroids – Testosterone propionate is ineffective and has many adverse effects – Close follow-up -----epithelial cancer. Squamous Hyperplasia Associated with a response to hormonal influences or exposure to exogenous irritants Precursor of squamous cell CA if cells are atypical Squamous Hyperplasia • This lesion produces hyperplastic thickening of the superficial squamous epithelium. • This lesion is a precursor of squamous cell carcinoma of the vulva Squamous Hyperplasia • Note the keratin horn cysts and the infiltrate of inflammatory cells at the base of the lesion. Squamous Hyperplasia • ITCHING is a common symptom. • If hyperkeratosis is not prominent, lesions may appear as reddish plaques. • The clitoris, labia minora, and inner aspects of the labia majora are more commonly affected. • Extensive lesions may result in stenosis of the vaginal introitus. Squamous Hyperplasia • Etiology – Repetitive scratching or rubbing from irritants – Treatment is aimed at halting the itch-scratch-itch cycle. Squamous Hyperplasia • Treatment – The same as lichen sclerosus – General attention to proper hygiene. – If the skin is moist or macerated, aluminum acetate 5% solution applied 3-4 times daily for 30-60 minutes is beneficial. – Systemic antihistamines or tricyclic antidepressants – Refractory lesions, intralesional injections of triamcinolone acetonide may be an alternative. lichen simplex chronicus • Hyperkeratotic, usually ill-defined, grayish, thickened, and sometimes excoriated lesion. • Usually located over the labia majora. • Hyperpigmentation. • Itching is always present and may be intense. lichen simplex chronicus • Lichen simplex chronicus of the vulva is the end stage of the itch-scratch-itch cycle. • The initial stimulus to itch may be: – Underlying seborrheic dermatitis. – Intertrigo – Tinea. – Psoriasis. – In most cases, the underlying cause is not evident and may have been transient vulvitis or vaginal discharge. • Any itching disease of the vulva may become secondarily lichenified. lichen simplex chronicus • Epidermal and epithelial hyperplasia, • Hyperkeratosis. • Fibrotic vertical streaks of collagen between the hyperplastic rete are present. lichen simplex chronicus • Treatment – Includes removal of irritants and/or allergens – Topical application of mild-to-high–potency corticosteroids. – Avoid soaps and cleansing agents other than aqueous cream. – Discourage excessive cleaning of the genital area; use of hot water; overheating; and wearing of synthetic, rough, and/or tight clothing. • Lichen simplex chronicus may be associated with underlying diseases (eg, Paget disease, Bowen disease) Lichen planus • Three types: – Papulosquamous – Erosive – Hypertrophic • Malignancy is possible in long-standing and ulcerative lichen planus. Lichen planus • The papulosquamous form: – Occurring as part of a generalized disease – Is the most common and is characterized by: • Flat-topped • Polyhedral, • Violaceous, shiny, and itchy papules located on keratinized skin of the labia and mons pubis. Delicate and whitish reticulated papules may be present on the mucosa, but no atrophy or scarring is observed. Lichen planus • The erosive form: – Involves the mucous membranes of the mouth and vulvovaginal area and may be locally destructive, leading to atrophy and scarring. – Synonyms include erosive vaginal lichen planus, desquamative inflammatory vaginitis, vulvovaginal-gingival syndrome, and ulcerative lichen planus. –Itching is rare, but pain, burning, and irritation occur and may be responsible for dyspareunia and dysuria. Lichen planus • The rare hypertrophic form: – Resembling lichen sclerosus, manifests with extensive white scarring of the periclitoral area with variable degrees of hyperkeratosis. – It may be very itchy. – Extensive vaginal involvement may result in a malodorous discharge. – Large denuded areas may become adherent, causing stenosis of the vaginal introitus and dyspareunia. – Marked atrophy may develop with time. ID/CC A 75 year old woman visits her gynecologist for a routine checkup and is found to have white spots on her genitalia HPI She complains of slight outer vaginal itching but denies any postmenopausal bleeding, vaginal discharge, or drug intake PE Hypochromic macules on labia majora extending to perineum and inner thighs in patchy distribution with scale formation; skin is thickened Pruritus vulva • Causes: – General – Local – Psychosomatic – Idiopathic • General Examination • Local examination: – Smears – Culture and sensitivity – BIOPSY: KEYE’s Dermatological knife BENIGN LESIONS OF THE Vagina • CYSTIC SWELLINGS • SOLID TUMORS • ATROPHIC VAGINITIS • VAGINAL ADENOSIS Cystic swellings • Gartner’s Cyst – Dilatation of the Gartner’s (Wollfian) duct – Anterior and lateral vaginal walls • Epithelial inclusion cysts • Endometrioma • Uretheral diverticulum Solid Tumors • Fibromyoma • Condyloma accuminata • Bilharzial polyps Atrophic vaginitis • Thinning and atrophy of vaginal epithelium • Most common in postmenopausal women with low estrogen levels • Dyspareunia and vaginal spotting (differential includes uterine cancer) Vaginal Adenosis • Persistent Mullerian columnar epithelium in the anterior wall and upper 1/3 of vagina • Manifestation of maternal DES exposure • Red, granular patches • Precursor of clear cell adenocarcinoma Vaginal Adenosis • Note the red granular patches on the vaginal mucosa on the left. The slide on the right shows glandular development. • Most patients are 7-35 years of age BENIGN LESIONS OF THE cervix • CERVICITIS • EROSION • POLYPS Inflammatory Lesions of the Cervix • Cervicitis (acute) • Symptoms: backache, bearing-down feeling in the pelvis, dull pain in the lower part of the abdomen, urinary tract symptoms Erosion of the Cervix • Characterized by columnar epithelium replacing squamous epithelium, grossly resulting in an erythematous area • Causes: – Physiological: – Cervicitis: Acute or Chronic – Hormonal therapy Erosion of the Cervix • Erosion of the cervix following delivery. A normal cervix is on the left Erosion of the Cervix • SMEAR – If infection---- Treat cause – IF CIN ------ Manage according to stage Chronic Cervicitis • Chronic inflammation, sometimes ulceration with repair, atypia or dysplasia, nabothian cysts from endocervical glands • Backache is a common symptom Chronic Cervicitis Nabothian Cysts • Endocervical glands blocked by inflammation or scarring. Chronic Cervicitis • Chronic inflammation underlies an area of cervical dysplasia Endocervical Polyps Postcoital bleeding and irregular vaginal spotting • Inflammatory proliferations of cervical mucosa; not true neoplasms • Soft; may protrude through the cervical os