Briefing on MHRA routine inspection of non
advertisement
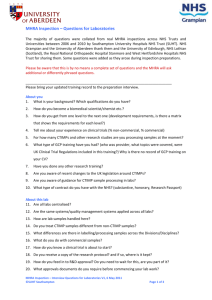
Briefing on MHRA routine inspection of noncommercial clinical trials Routine Good Clinical Practice (GCP) MHRA Inspection, University of Aberdeen 2011 Aims MHRA inspections MHRA inspection at University of Aberdeen How should staff prepare? Advice for staff on key areas of weakness So that: You can identify and address any actions required You can participate in the interviews with confidence University of Aberdeen can demonstrate that clinical trials are following current legislation and are conducted to high safety and quality standards. Why do the MHRA Inspect? EU directive 2001/20/EC transposed into UK law May 2004 as Medicines for Human Use (Clinical Trials) Regulations 2004 Legal obligation to conduct Clinical Trials of Investigational Medical Products (CTIMPs) to Good Clinical Practice (GCP). MHRA is statutory body responsible for compliance with UK regulations MHRA inspect (CTIMPs) on humans covered by the regulations 3 Types of MHRA Inspection Routine Triggered Requested University of Aberdeen inspection is routine Provisionally 4 days week of 20 June 2011 Who do the MHRA inspect? Legally able to inspect all organisations ‘sponsoring’ or ‘hosting’ clinical trials in the UK Includes commercial and non-commercial organisations Adapt inspection to organisation type Routine inspections focus on systems What do the MHRA inspect? University has systems in place to support conduct of CTIMPs in compliance with regulations (and GCP). Specific examples of CTIMPs to demonstrate those systems Areas of interest include: Approval processes and regulatory submissions Contract Management Trial file and data management Quality assurance and monitoring Training IT systems Pharmacovigilance Archiving Laboratories Pharmacy What happens before the inspection? ■ University notified by MHRA of inspection 4th February 2011 ■ Dossier sent to MHRA on 4th March 2011. Including a list of CTIMPs (live and complete) to give an overview of clinical trial activity. MHRA provide draft agenda approx 6 weeks prior to the inspection Teleconference to finalise agenda approx 2 weeks prior to inspection University will coordinate the inspection What are we doing to prepare? MHRA Inspection Internal Working Group Gap analysis and action plan Monitoring and Audit Informing staff of the inspection Staff training – GCP What are the key areas of weakness? 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Qualifications and training Communication Delegation of duties Standard Operating Procedures Evidencing of information Study file and filing Pharmacovigilance Informed Consent Equipment Study closure and archiving Pharmacovigilance Sponsor responsibility to ensure events are reported in accordance with regulations. Currently have central reporting (documented in CI delegation letter) . New SOP to be issued with updated process Monitoring/Audit Sponsored studies will be audited to ensure that essential documents are present in the Trial Maser File. Training record will be required for trial personnel on a study delegation log. What can you do to prepare? Handout available with recommendations for addressing key areas of weakness. SOPs for maintaining a Trial Master File, Investigator Site File, Pharmacovigilance will be available soon What happens during the inspection? Opening meeting – inspectors present inspection plan Document review – including medical notes Interviews with selected staff Tour of facilities Additional requests Closing meeting – summary of findings and provisional grading Interviews with study personnel on study conduct These assess knowledge of GCP and regulatory requirements, and probe for evidence of robust processes for ensuring compliance with GCP You should read through the example questions and answers provided. Common Themes During Interview: Training Communication Safety reporting Protocol procedures & adherence Investigational medicinal product handling Informed consent Approval process including amendments Annual reports to ethics/MHRA Statistics and data handling Out of hours/leave cover Randomisation & unblinding procedures End of trial & archiving procedures Dos and Don’ts during Interview Be honest - we know we have some gaps and are addressing them - failure to recognize the gaps is more problematic than acknowledging the gaps Avoid being confrontational - esp. avoid giving the impression that this is ‘bureaucratic detail’ Be ‘alert’ to areas of improvement Avoid being defensive. Dos and Don’ts during Interview Only answer the question asked If mistakes are made or wrong answers given, correct them at an appropriate time, or ensure somebody else does so. Try your best to correct any deficiencies noted by the inspectors before they leave Demonstrate confidence in your trial systems and data – you know it best. Be positive. Dos and Don’ts during Interview Should inspection findings be made, make sure that you understand them completely – it is easier to ask the inspector for clarification during the inspection rather than after the report is issued. Don’t volunteer information It is appropriate to challenge a finding made by an inspector if you are certain they are incorrect, but do not persist in your objection. What happens after the inspection? MHRA to report issues within 30 days of the inspection, summarising findings. University response will include an action plan, timelines to address any findings. MHRA receive response - will issue a closing letter and GCP Inspection Statement. Future inspections will be performed at a frequency determined by the MHRA. Possible routine GCP inspection of NHS Grampian Summary ■ Review your trial documentation and training files for staff. ■ ■ ■ ■ ■ Have evidence of training (GCP certificate, CV) Ensure you can explain your role in the trial Review the typical questions and answers provided Familiarise yourself with new SOPs when available Be confident of your trial and processes. Remember that you know your trial better than anyone else. Any Questions? Main Contacts: Prof Phil Hannaford – p.hannaford@abdn.ac.uk Prof Alison MacLeod – mmd175@abdn.ac.uk Dr Gail Holland – g.holland@abdn.ac.uk Tel: 01224 - 555076 Lynda Sime – lynda.sime@nhs.net Tel: 01224 -554656