Clinical Coaching
advertisement

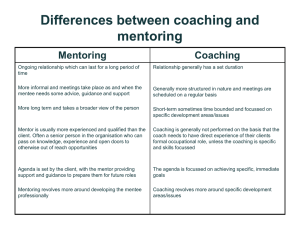
Clinical Coaching: An Approach to Motivating Clinical Practice Change in Home Care Adele W. Pike RN, EdD Background: New Trends, New Ideas and Better Practices in Geriatric Home Care Motivating clinical practice change among home care clinicians has many challenges given the autonomy of their roles and the multiple (and often competing)demands for their time and attention. In 2007, Adele Pike was selected as a Geriatric Practice Change Fellow (www.practicechangefellows.org) Her change project was to create a model for motivating evidence-based practice change among home care clinicians and then to use that model to improve core geriatric competency. The critical objective of this project was to increase the knowledge, skill and confidence of front line managers in motivating clinical practice change. Clinical Coaching was identified as the tool front line managers identified as holding the greatest promise for motivating practice change among clinicians. Consensus on What is “Clinical Practice” Clinical Practice is the hands on care that clinicians provide at the bedside, the chairside, or the home-side. It includes patient and family assessment, critical thinking about the assessment and ensuing creation of a plan of care. Additionally, clinical practice is the actual “hands on” application of interventions, and evaluation of the patient’s family’s response to interventions. Clinical Coaching Clinical coaching is a purposeful, planned, regularly occurring meeting between clinician(s) and manager for the purpose of envisioning, planning and improving patient care in accordance with evidence based practice. One to one coaching meetings are goal driven with a clear articulation of the purpose, the expected outcomes, and the agenda for each encounter. Coaching in this context can be conceived of as a “thinking partnership” between manager and clinician, and must be grounded in mutual trust and respect. Managers use skills such as active listening, asking thought provoking questions, providing feedback, reinforcement of practice strengths, reframing of clinical situations, and transforming ideas into action steps to help clinicians integrate changes into their clinical practices. Managers use a formalized process to follow up on these action steps. What’s the Goal? To facilitate ongoing development of the clinician in the context of practice and to enhance the delivery of care. -Hines-Martin, V. and Robinson, K. (2006). Supervision as Professional Development for Psychiatric Mental Health Nurses. Clinical Nurse Specialist. 20(6), 293-297 Styles of Clinical Supervision ≈ Prescriptive ≈ Informative ≈ Confronting ≈ Supportive ≈ Catalytic Clinical Coaching Skill Set •Managing Meetings •Prepping for coaching sessions •Differentiating when a clinician will benefit from coaching and when a clinician needs a corrective action plan •Formulating Socratic Questions •Active Listening •Giving Feedback •Timely and consistent follow up Steps in Clinical Coaching 1. The Invitation to Clinical Coaching 2. Selecting the Location 3. Planning the Logistics 4. Plan for the Session 5. Running the session 6. Plan for follow up 7. The Follow Up The Invitation to Clinical Coaching Inviting clinicians into a coaching relationship takes thought and planning. Clinicians’ defenses and suspicions can go up quickly and coaching can readily be perceived as a disciplinary tool. Selecting the Location In the office? Out of the office? At the curbside? Planning the Logistics Time to Meet Prevent Interruptions Avoid Distractions Seating Arrangement Planning for the Session When preparing for a coaching session, ask yourself, “What do I really want to be the outcome?” and use that as your compass. Running the session The two riskiest times in a coaching session tend to be at the beginning and at the end. -Patterson, K., Grenny, J., McMillan, \R., and Switzler, A. (2002) Crucial Conversations. McGraw-Hill Center for Creative Leadership’s Framework for Coaching: A- Assess C- Challenge S- Support www.ccl.org Center for Creative Leadership’s Coaching Framework Applied to Clinical Coaching in Home Care Coaching Element What’s Involved? ASSESS (allow 10 minutes) CHALLENGE (allow 20 minutes) SUPPORT (allow 10 minutes) Identifying what you see as an area for practice improvement Discovering the clinician’s perspective about what you have identified Assessing clinician’s motivation to improve this area of practice; to grow and/or change his or her practice What are the clinician’s strengths and interests and areas for growth What would the clinician consider improvement or success in this area of practice Engage the clinician in dialogue, problem solving about a particular patient situation, and/or envisioning about how care could be even better than it is now You want to create a bit of a disequilibrium for the clinician between current practice and what practice could be You want to challenge the clinician – or better yet- get him or her to challenge him/herself to growth his or her practice around this issue Support a plan for practice growth, but not a plan to “do for “ the clinician End the session by getting the clinician to identify learning needs and then help in finding resources to meet those needs Help by managing or problem solving barriers to the clinician addressing learning needs Recognize wins and set backs Acknowledge small gains and improvements Celebrate success Skills that can help Socratic Questioning Active Listening Socratic Questioning Active Listening Written action or follow up plans Regularly planned follow up meetings Regular and spontaneous feedback Socratic Questioning Thinking is driven by questions, not by answers What’s a “Good Question”? •One • that causes clinicians to reflect on their practice • One that probes the decisions clinicians have made in a particular patient situation • One that encourages clinicians to think about how care could be different One that causes clinicians to question the assumptions on which they base clinical judgments • One that engages clinicians in discovering their own answers to clinical problems Sample Socratic Questions What is your experience with this clinical problem? How do you manage this problem when it occurs with a patient in your care? Describe how patients have responded when you have managed the problem this way? What other ways are there of managing this problem? What is another perspective you could consider? What is another approach to care you could try? What would superb care of this patient look like? What would be the outcomes of this care? What do you think about the outcomes your patients achieve? Planning for Follow Up The two riskiest times in a coaching session tend to be at the beginning and at the end. -Patterson, K., Grenny, J., McMillan, \R., and Switzler, A. (2002) Crucial Conversations. McGraw-Hill The Follow Up Leaving following up to chance reduces clinical coaching to a nice chat! Practice and Reflection “It takes a lot of practice to adopt a coaching approach to practice improvement and to stop wrestling with clinicians and start partnering with them” -Diane Garrow Patient Service Manager Visiting Nurse Association of Boston Opportunities for Practice and Reflection •Every other week “Coaching for the Coaches” Rounds •Role Plays and Video Case studies •Small, rapid cycles of change: try something new and out of the box and see what happens •Using clinical coaching with joint visit: Discovering of the power of Curbside Coaching