Safe Patient Handling Initiative - UCLA Health
advertisement

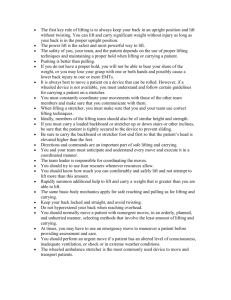
Safe Patient Handling Initiative January 29, 2014 1 BACKGROUND – Injury Rates • The CDC rates musculoskeletal injuries from overexertion in healthcare occupations as one of the highest rates of injuries among all U.S. industries. Data from the Bureau of Labor Statistics (BLS) showed that in 2011, the average rate of overexertion injuries across all industries were 38 per 10,000 FTEs. By comparison, the overexertion injury rate for hospital workers was twice that average (76 per 10,000 FTEs) during the same time period. • The single greatest risk factor for overexertion injuries in healthcare workers was from manual lifting, moving and/or repositioning of patients. 2 BACKGROUND – AB 1136 • On January 1, 2012, the Hospital Patient and Health Care Worker Injury Protection Act (aka Safe Patient Handling) became effective. This law required general acute care hospitals to adopt a safe patient handling policy as part of their Injury and Illness Prevention Program. • Requirements included: replacing manual lifting and transferring of patients with powered patient transfer devices, adding trained lift teams, training staff on safe patient handling practices and investigating injuries associated with patient handling. • The general lifting restriction is 35 pounds 3 UCLA’S Plan • UCLA has been ~75% compliant due to current lift teams • Lifting restriction is 35 pounds, so lift team can’t handle all patient lifts with present staffing. • Have also selectively purchased equipment and started training staff • Product demos conducted over past 8 months; multidisciplinary teams • Decided on Arjo-Huntleigh and SAGE products 4 Implementation Plan LIFT TEAMS: • Focus on ICUs & step down units (where heaviest lifting needs are) • Available for consultation / special circumstances on the floors • Lift Team will have a set of equipment to use 5 Implementation Plan, cont. EQUIPMENT: • Selectively purchase equipment for each unit, based on unit’s lifting needs • Be sure lifts are readily available to staff; “parking spaces” identified on each unit. • Most supply items are single patient use items available on unit supply carts • Materials Management to track par levels; available through Owens & Minor 6 EQUIPMENT • Maxi Move (Arjo): hoyer lift) For max/dependent patients (like a • Sara Plus (Arjo): For moderate assistance for standing up; can be used for transfers to chair, toilet, commode 7 EQUIPMENT • Sara Stedy (Arjo): For min-moderate assist; patient must be able to stand and grip; for transfers to chair, toilet, commode • Flites (Arjo): Antifriction sheet used for lateral transfers, bed repositioning, etc. 8 EQUIPMENT • Maxi Air (Arjo): Blow up air mattress for lateral transfers; bariatric patients, etc. • Maxi Sky (Arjo): Ceiling lift, for future consideration. Rooms need to be retro fit. 9 EQUIPMENT • Prevalon Bed Sheet (SAGE): Used for bed repositioning, lateral transfers; stays under the patient • Includes positioning wedges and liner (can use chucks) • Single patient use – issued to patient 10 EQUIPMENT • Prevalon Chair Sheet (SAGE): Used for chair repositioning • Line with chucks • Single patient use 11 TRAINING • Core team at each campus: Training coordinator Rehab Lift Team 2 Nursing champions per unit (day/night shift) • 1 full day training for core teams • Create “Culture of Safety” • ICU staff will be trained by lift team, as equipment is deployed 12 TRAINING • Spend 1 week on each nursing unit • Day and night shift hours • Coordinator and unit champions to make sure all staff are trained • After training, spend rest of the week on the unit coaching, problem solving, retraining, etc. • Training algorithms & resource binders available, including pictures of each lift • Competency forms for files • HR Tracking 13 TRAINING • After initial training, return to each unit for additional training, problem solving, etc. • Accountability if employee refuses to use lift • Part of unit orientation for new hires • Include in annual competencies, as needed (should be high frequency use!) (plan in progress) 14 IMPLEMENTATION TIMLINE • October: Proposal approved Equipment ordered • Early-mid November: Training for core teams • Mid-November: Deploy SAGE products to ICUs • December, 2013 – February, 2014: Unit training • To date, ~100 champions and ~200 staff nurses trained • February, 2014: Unit retraining, if necessary 15 PUBLICITY- Training Stickers 16 PUBLICITY – Badge Holders 17 PUBLICITY – Flyers Plus lots of emails, presentations, and articles! 18 Sustaining the Program Safe Patient Handling Coordinator • Full time FTE • Health System position (both campuses) • Duties: Investigate injuries; maintain statistics Follow new legislation; insure compliance Provide training / retraining Track new products; replace what doesn’t work Help track usage and par levels Represent UCLA at UCOP level Make regular rounds / trouble shoot 19 REPORTING & OVERSIGHT • Environment of Care Committee • Workman’s Comp Strategy Group • Periodic updates to Health System Leadership • Regular follow up with Unit Directors and other department heads • UCOP Safe Patient Handling Task Force 20 NEXT STEPS • Finalize the Safe Patient Handling Coordinator • Policy approval • Finalize plan for initial and annual competencies • Complete training on the inpatient units • Complete training in other areas: OR, ED, Radiology areas, Escort, Gonda, Transport, etc. • Create blog for SPH champions & equipment feedback • Closely track injury reduction! • Involvement on UCOP level 21 SPECIAL THANKS • Erik Eggins, Safety Department • Materials Management • MOC • Loading Dock • Facilities • Nursing Leadership • Rehab & Lift Team 22 23