Giving Effective Feedback
Using the RIME Method for
Effective, Brief Evaluation &
Feedback in the Clinical Setting
Objectives
3.
4.
1.
2.
Explain the purpose of the RIME feedback method.
Describe the RIME Schema and associated behaviors/competencies.
Practice using this method to give feedback.
Reflect on the outcomes of using this method and consider ways to improve your application of the method in the future.
What is it?
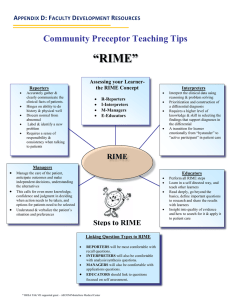
The R-I-M-E Method
(Reporter-Interpreter-Manager-Educator)
Provides a systematic, objective framework to “diagnose” a learner’s functional level & then provide recommendations on how to move to the next level;
Uses manageable, observable & easily understood concepts that demonstrate growing levels of professional knowledge & behavior;
Facilitates focused verbal assessment of learners on competencies such as problem identification, reasoning, communication, physical examination, written documentation, & professional attributes;
Allows clear, brief, meaningful & useful feedback to learners in a timely manner.
How Does it Work?
The RIME method, developed by Louis Pangaro, MD
allows brief, constructive & timely evaluation & feedback, uses a simple level of competency rubric, reinforces appropriate behavior, motivates students via immediate, brief, focused & constructive feedback, can improve inter-rater reliability by providing a systematic rubric.
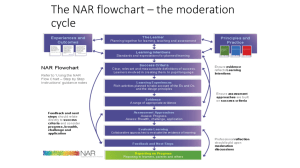
The RIME schema describes expected cognitive & behavioral progression in the development of medical skills. Instructors use the competency schema to:
quickly assess student performance, decide what skills to provide feedback on at each teaching opportunity, frame their feedback so as to encourage significant improvement.
Pangaro, LN. A new vocabulary and other innovations for improving descriptive in-training evaluations. Acad Med. 1999
Nov;74(11):1203-7
Reporter
The learner:
accurately gathers & clearly communicates the clinical facts on his/her patients,
demonstrates a clear sense of responsibility, develops consistency in “bedside” skills.
These skills must be mastered as a criterion for passing the clerkship (and to fulfill competencies required for graduation).
Interpreter
Transitioning from “reporter” to “interpreter” is essential for a third year student, but often very difficult.
Clinical test data provide an “interpreting” opportunity that requires:
a high level of knowledge,
skill in selecting clinical findings that support the diagnosis, skill in applying results appropriately in a specific case.
The student must transition emotionally & cognitively from “bystander” to active participant in patient care.
Manager
Requires increasing knowledge, confidence & judgment in deciding when action needs to be taken and in selecting among & proposing options for patient care.
Student must learn to tailor the plan to the patient’s specific circumstances & preferences.
Can’t expect that a student’s diagnostic & treatment suggestions will always be “right”– so it’s best to ask them for 3 options.
Educator
Success in each prior step depends on self-directed learning & mastery of basics.
An advanced trainee (educator level) will demonstrate:
the drive to look for evidence on which clinical practice can be based,
the skill to recognize evidence that can stand up to scrutiny,
going beyond the required basics to read deeply and share new learning with others,
the insight to identify questions that are important to research in more detail,
the maturity & confidence to share leadership in educating the team
(and even the faculty).
RIME Schema
Reporter
Interpreter
Manager
Educator
Behaviors for Feedback
Reliably, respectfully, honestly gathers information from patients & communicates clearly with faculty.
Gets the basic work done.
Answers the “what” questions.
Presentation shows selectivity, prioritization & implies analysis.
Demonstrates active involvement in thinking through the patient’s problems, interpreting the data & acquiring the knowledge to offer a reasonable differential diagnosis.
Answers the “why” questions.
Works with patients on diagnostic & therapeutic decisions, continually developing expertise -- as demonstrated in clinical planning.
Consistently answers “how” to resolve problems.
Personal planning & reflection demonstrate a commitment to develop expertise.
Demonstrates ongoing efforts to self-correct & improve.
Tips for Using the RIME Method
Evaluate or “diagnose” the learner based on current level of knowledge & skill development, as well as any noticeable improvements in performance.
Recognize that the learner’s development is in process, and consider performance in that light.
Carry a pocket-sized card that summarizes the RIME levels so you can refer to it quickly when giving feedback, and can share the rubric with the learner.
Avoid personal biases & comparisons with others when assessing the learner’s performance.
It is most effective to focus first on what the learner has achieved, and then briefly highlight areas where you see the possibility for further growth.
Maximize the learner’s motivation to improve by using constructive, encouraging words
& giving clear examples of how to change his/her behavior.
Quick Review
1.
2.
The RIME feedback method is designed to provide: a. a detailed & comprehensive method for competency-based feedback & evaluation.
b. a quick & easy method for meaningful, competency-based feedback & evaluation. c. a system of feedback & evaluation that allows learners to guide the feedback process in order to improve their clinical skills.
One example of a competency that can be evaluated effectively using the RIME method is: a. showing commitment to self-correction & self-improvement.
b. accepting that, as learners, the resolution of problems will be above their skill level.
c. always relying on the attending or resident to outline a treatment plan.
Quick Review
3.
To give effective feedback to a student via the RIME method, you: a. Ask her to write a comprehensive H&P, then present the patient to you with differential & detailed recommendations for a treatment plan. After finishing your rounds for the day, you review the student’s written recommendations and then give her feedback the next time she rounds with you.
b. Check to see if she has transitioned from an observer to an active participant in the patient’s care by asking her for a diagnosis & treatment plan (“Manager” level). You then reinforce any accuracies in her diagnosis & treatment plan, and ask her opinion about alternatives you think she should consider.
c. Point out the fact that her diagnosis & treatment suggestions are inaccurate and unfounded based on details of the patient’s history that the student seems to have ignored. You suggest that, if she wishes to become a competent physician, she should be more thorough and pay better attention to details.
Quick Review
4.
To improve your application of the RIME method in the future, it would be helpful to: a . Reflect on the fact that the student is still developing clinical skills, so you should focus on pointing out errors and shortcomings to help improve performance in the future.
b. Realize that the student will likely be able to perform better next time if you point out how well student “x” performs, and set that as a goal for the student to work towards.
c. Reflect on the student’s response to your feedback, and adjust your style of communication in the future to provide encouragement for her to continue learning & improving.
Answers
1. (b) much of the value of the method is due to it’s ease of use
& brevity. Therefore, “a” is wrong because it suggests a long, complex process; and “c” is wrong because the instructor, not the student, should guide the process.
2. (a) is correct because it reflects a developing competency, while “b” and “c” do not indicate any motivation to develop skills of analysis & planning.
3. (b) reflects appropriate use of the RIME model & skill in encouraging the learner; “a” involves too much time lapse, and “c” discourages the learner.
4. (c) will help you reframe your teaching to encourage the student to do better; while “a” & “b” will reinforce your thinking that the student is a poor performer and will likely lead to behaviors that will discourage her improvement.