May 2012 APDEM Agenda
advertisement

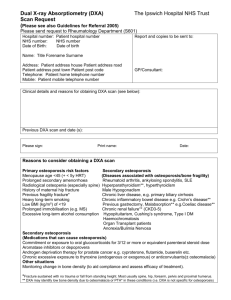
Friday, May 25, 2012 1. 2. 4. 5. 6. Welcome and Introduction ACGME “Next Accreditation System” (NAS) Update on the ESAP In Training Examination (ESAP-ITE) APDEM Site Visit Tool Box APDEM Procedural Requirements Task Force ESAP Ite 2012 • Total training programs: 128 • Total fellows: 525 • Mean score: 55.1% [28.3% to 81.7%] 1st years 2nd years Others Mean score 51.7 57.7 58.4 Number of fellows 239 175 111 Procedural Task Force Recommended Curricula, 1st draft Background • ABIM in discussions with different subspecialties about documentation of procedures • APDEM leadership met with endocrine representative to ABIM to discuss issues • APDEM created Procedural Task Force to discuss issue and develop list endocrine procedures Background (cont’d) • List of the following procedures was developed by task force: – Continuous Glucose Monitoring System – DXA Evaluation – Thyroid Ultrasound/FNA • After list was developed, representatives from APDEM, AACE, ATA, The Endocrine Society were asked to develop model curricula for review by APDEM membership and eventual discussion with ABIM representatives Thyroid Ultrasound/FNA • Understand indications for neck ultrasound in evaluation of thyroid nodules and for post-operative thyroid cancer surveillance • Interpret thyroid imaging, addressing: – – – – Quality of imaging Thyroid parenchyma echotexture and size of lobes Location and size of nodule(s) Sonographic features of nodule(s) • Perform thyroid ultrasound (minimum of 5 studies to be complete and competent with direct observation by Ultrasound proficient faculty member) with both documentation of images and reporting to include: – Measurement of each thyroid lobe in 3 dimensions with description of parenchyma echotexture – Measurement of isthmus in transverse view – Measurement of each nodule of interest in 3 dimensions with description of location and sonographic features (echogenicity, composition, presence of calcifications, margins, vascularity) • Perform ultrasound guided fine needle aspiration of thyroid nodules (minimum of 5 studies with the fellow documented to be competent by Ultrasound proficient faculty member) in the ability to place needle in nodules of interest accurately with ultrasound guidance Continuous Glucose Monitoring • • • Understand technology of continuous monitoring Understand guidelines and consensus statements concerning CGM from AACE and The Endocrine Society Professional CGM – – Understand the evidence base and indications for Professional CGM Analyze data • • – Provide a minimum of 5 interpretations and reports reviewed by CGM proficient faculty and competency documented summarizing the following: • • • • • Current therapy for diabetes Data adequacy Findings of tracings and logbook Suggested therapeutic changes based on findings and current therapy Personal CGM – – Understand the evidence base and indications for Personal CGM Understand Personal CGM features: • • – Be proficient in setting alarms Perform download of the data Interpret and initiate appropriate therapeutic changes based on the CGM data on a minimum of 5 CGM downloads reviewed by CGM proficient faulty, including: • • • • Adequacy of the report (MAD, paired readings, etc) Interpreting the data (integrating logbook with the CGM data) The patient’s current therapy for diabetes Findings on CGM Suggested therapeutic changes Pass a proficiency test – 50% questions and 50% interpreting reports with 2 Professional and 5 Personal CGM cases DXA • Understand indications for DXA as part of work-up for osteoporosis/metabolic bone disease – Know appropriate clinical and laboratory testing approaches for osteoporosis – Apply the WHO classification for diagnosis of osteoporosis – Assess and monitor the fracture risk of the patient • Understand the basic science of Bone Densitometry and Operating Principles – Describe basic DXA anatomy – Explain the basic principles of operation for • DXA – Central skeletal DXA – Peripheral DXA (pDXA) • QCT and pQCT • Quantitative Ultrasound (QUS) • Understand Radiation Safety and Quality Issues – List properties of x-rays and biological effects of radiation; radiation safety – Define the units of expressing radiation dose; typical dose or DXA exam DXA (cont’d) • Understand DXA Method, Diagnosis of Osteoporosis, and Assessment of Fracture Risk – – – – – – – – – • Understand Longitudinal Monitoring by DXA – – – • Patient positioning and scan analysis (PA spine, hip, forearm, total body); recognize common errors in DXA analysis Review skeletal anatomy relevant to DXA Recognize common artifacts on DXA scan images Define standardized scores used in bone densitometry (T-and Z-score) Compare and contrast use of different skeletal sites and regions of interest for diagnosis Discuss the diagnosis of osteoporosis in pre-menopausal women, children, men-of different ethnic groups Understand the use of central DXA for predicting fracture risk Define absolute vs relative risk Explain fracture risk assessment combining BMD with other risk factors (WHO FRAX model) Know how to calculate precision error and least significant change Know which skeletal site to measure, and how often to test Explain clinical relevance of changes in BMD Perform DXA Reports (minimum of 5) after reviewing scans with an ISCD-certified expert, utilizing: – – – – Standard nomenclature for use in bone densitometry reports ISCD basic recommendations for reporting densitometry results, or as appropriate, ISCD optional recommendations for reporting densitometry results Review for common errors in DXA reporting Apply the ISC recommendations using case examples • Next meeting APDEM Annual Meeting Hilton Americas Houston Room 335 June 24, 2012 5:30 p.m. EST