Dual X-ray Absorptiometry (DXA) I
advertisement

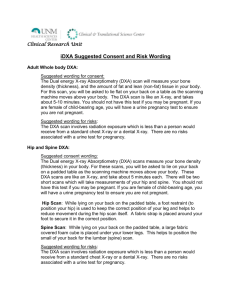
Dual X-ray Absorptiometry (DXA) Scan Request (Please see also Guidelines for Referral 2005) The Ipswich Hospital NHS Trust Please send request to Rheumatology Department (S601) Hospital number: Patient hospital number NHS number: NHS number Date of Birth: Date of birth Report and copies to be sent to: Name: Title Forename Surname Address: Patient address house Patient address road Patient address post town Patient post code Telephone: Patient home telephone number Mobile: Patient mobile telephone number GP/Consultant: Clinical details and reasons for obtaining DXA scan (see below): Previous DXA scan and date (s): Please sign: Print name: Date: Reasons to consider obtaining a DXA scan Primary osteoporosis risk factors Menopause age <45 (+ < 5y HRT) Prolonged secondary amenorrhoea Radiological osteopenia (especially spine) History of maternal hip fracture Previous fragility fracture* Heavy long-term smoking Low BMI (kg/m²) of <19 Prolonged immobilisation (e.g. MS) Excessive long-term alcohol consumption Secondary osteoporosis (Diseases associated with osteoporosis/bone fragility) Rheumatoid arthritis, ankylosing spondylitis, SLE Hyperparathyroidism**, hyperthyroidism Male Hypogonadism Chronic liver disease, e.g. primary biliary cirrhosis Chronic inflammatory bowel disease e.g. Crohn’s disease** Previous gastrectomy, Malabsorption** e.g.Coeliac disease** Chronic renal failure** (CKD3-5) Hypopituitarism, Cushing’s syndrome, Type I DM Haemochromatosis Organ Transplant patients Anorexia/Bulimia Nervosa Secondary osteoporosis (Medications that can cause osteoporosis) Commitment or exposure to oral glucocorticoids for 3/12 or more or equivalent parenteral steroid dose Aromatase inhibitors or depoprovera Androgen deprivation therapy for prostate cancer e.g. cyproterone, flutamide, buserelin etc. Chronic excessive exposure to thyroxine (endogenous or exogenous) or anticonvulsants(± osteomalacia) Other situations Monitoring change in bone density (to aid compliance and assess efficacy of treatment). *Fracture sustained with no trauma or fall from standing height. Most usually spine, hip, forearm, pelvis and proximal humerus. ** DXA may identify low bone density due to osteomalacia or PTH* in these conditions (i.e. DXA is not specific for osteoporosis) Using DXA to predict fracture Low bone density measured by DXA is a strong predictor of future fracture. The lower the bone density (or T score) the higher the risk. Lumbar spine and hip (femoral neck or total hip area) DXA is the gold standard technique for assessing the risk of fracture at each site. DXA results can be used as part of a full fracture assessment (FRAX) Lumbar spine DXA measures in the elderly may be invalid owing to degenerative changes in the spine and soft tissue calcification skewing the results (essentially over-estimating bone density). We recommend scans are rarely helpful in those > 80 years old given the above and that bones are invariably in the ‘osteoporotic range’ anyway at that stage. Be aware that the validity of DXA measures may need to be substantiated by viewing corresponding lateral and AP spinal radiographs. Using DXA to monitor changes in bone density DXA may be useful to assess initial efficacy of therapy (2-5 years after starting bisphosphonates or 12 months after starting strontium ranelate). Repeat DXA assessments may be useful to aid adherence to drug therapy, but are not routinely recommended. In the future monitoring of anti-resorptive therapy such as bisphosphonates over the short-term may be best done in practice by assessing biochemical measures of bone collagen crosslinks in serum or urine. If in doubt please contact Dr Gavin Clunie, Consultant Rheumatologist, (gavin.clunie@ipswichhospital.nhs.uk, extension 1039 or bleep 332) or administrator sue.holdaway@ipswichhospital.nhs.uk extension 1571 (702571) V2 GC 03/05