CPAP
advertisement

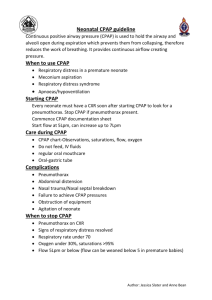
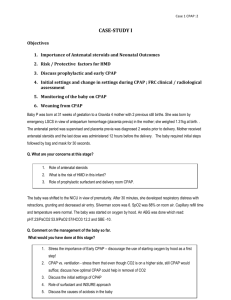
1 RSPT 2353 – Neonatal/Pediatric Respiratory Care CPAP Lecture Notes Reference & Reading: Whitaker Chapter 15 I. Actions of CPAP A. It raises the mean Airway pressure, which increased the FRC back to normal, which brings the lung compliance back up. This has the action of decreasing the WOB B. The CPAP recruits alveoli, which increases surface area of alveoli so that the PaO2 rises. C. CPAP can stent open upper airways to help in obstructive apnea D. CPAP can stent open lower airways to decrease airway closure (Remember, this particular technique one can result in air trapping.) II. Indications for CPAP A. There are two basic categories that would indicate CPAP: 1. Clinical states that require an increased FRC (increasing the FRC will stimulate respiration by altering stretch receptor reflexes mainly Hering-Breur reflex) 2. Clinical state that require positive pressure to maintain the patency of the airways. B. Patient has a PaO2 of less than 50 torr on an Fi02 of more than 50% C. Patient has Apnea of Prematurity with or without a degree of upper airway obstruction D. Patient has a reasonable pH (above 7.25) and PaC02 of 50-55 torr III. Contraindiations for CPAP (per AARC Clinical Practice Guidelines) A. bronchiolitis B. abnormal upper airway anatomy C. cardiovascular instability 2 D. unstable respiratory drive with multiple apnea associated with desaturations E. ventilatory failure (C02 ≥ 60 torr & pH ≤ 7.25) F. untreated diaphramatic hernia IV. Initial settings for a neonatal patient A. Place on same FiO2: either from hood or <60% B. As per AARC CPG: Begin CPAP at 3-6 cmH2O, increase by 2 cmH2O to stabalize PaO2 >50 torr at an FiO2 <70% C. Deciding acuity Baby Girl A On 50% oxyhood, SpO2 is 83% and RR is 70 bpm Placed on NCPAP of 4 and FiO2 50%, SpO2 increases to 92%, RR is now 55 bpm Pt is stable and assessment remains the same Can this patient remain on CPAP? Baby Boy B On 50% oxyhood, SpO2 is 83% and RR is 70 bpm Placed on NCPAP of 4 and FiO2 50%, SpO2 only rises to 85% CPAP is gradually increased to 10, FiO2 60% SpO2 remain 85%, RR is 70 bpm Assessment remains the same despite efforts to increase CPAP & FiO2 Can this patient remain on CPAP? D. Do not exceed 10-20 cmH2O. It can result in: 1. inflation of the belly and causing nausea and vomiting 2. may decrease the Vt so that the PaCO2 rises V. Delivery Systems – There are two main types A. Continuous flow: provides non-interrupted supply of gas and does not require the patient to initialize a breath B. Demand flow: 1. Usually incorporated in mechanical ventilators 2. The pt must initiate a breath for gas to be delivered most machines now have a bias flow to deliver flow triggered breaths 3 VI. Resistors – opposes the flow, resulting in a baseline pressure as a result of the back pressure from the circuit A. Flow - The simplest way to create CPAP is to increase the flow rate past the point where the resistance of the exhalation valve can allow the gas to leave. Because the flow fills up the circuit faster than it is vented out, the back pressure creates positive pressure. B. Threshold - a device that creates PEEP and CPAP by the use of a spring or other type of device that keeps a preset level of pressure on the exhalation valve… within the specified flow rate of that equipment. VII. Freestanding CPAP – Some patients in this population do not require the use of a ventilator to administer CPAP. To create a freestanding CPAP system you will need the following: A. O2 blender with a regular flowmeter that gets 10-12 lpm B. O2 line and adapter to 22 mm C. O2 analyzer probe D. H formation for IMV with bag E. Heated humidifier F. Corrugated/aerosol hose (standard length) G. Thermometer/temperature probe H. In line pressure pop off I. Brigg’s adapter (T-Tube)for connection to the infant’s ET tube or prongs J. 15 inches of aerosol hose K. Spring-loaded PEEP adjustable threshold resistor (type found on resuscitator bags exhalation ports) VIII. Delivering CPAP A. Endotracheal tube: 1. ADVANTAGE: easy to suction and can bag if patient gets into trouble. 2. DISADVANTAGE: tempted to bag too often. Increased RAW through the tube B. Nasal-pharyngeal tube placement: 1. ADVANTAGE less resistance, but confusing to people who think the patient has become extubated. 2. DISADVANTAGE this tube can direct the air right into the stomach and cause increased gastric distention and vomiting C. Nasal mask such as BiPap is poor choice for children under 1- 3 years of age 4 D. Head chamber is unsuitable because the patient is at risk for airway occlusion as well as N & V (pp. 302, fig. 18-7) E. Nasal prongs: if you pick one that is too long it has increased RAW… VESTA brand bad choice. ARGYLE is most popular ***NOTE: Problems with the nasal prongs there are great differences between the RAW between various types of NCPAP interfaces. The longer narrower prongs that stay inside the nose, have much higher RAW than the ones that look more like nasal cannula. (reference: Respiratory Care 31:18, 1986) IX. Monitoring the pt while on CPAP A. Monitoring after initially placing on NCPAP 1. Sp02 above 88-92% or per MD order/facility policies 2. Respiratory rate back down to normal 3. Retractions diminished 4. Apnea and bradycardia decrease 5. ABG indicates that the acid base balance is not acidic and that there is no hypercapnia B. Monitor the airway patency: If there is some type of occlusion the SpO2 drops, the patient may have decreased breath sounds, the patient may have apnea & bradycardia 1. Remove nasal prongs, have someone hold O2 to face while you irrigate and suction the nasal pharynx of the baby 2. If the patient’s airway is not patent on nasal CPAP he might require intubation with CPAP C. Monitor 1. 2. 3. 4. 5. 6. for the s/s of respiratory distress, WOB Retractions present or increase Increased HR and/or RR Grunting presents See saw respirations Decreasing SpO2 Cyanosis D. Monitor the FiO2: if the Fi02 is above 50% there is a increased chance of O2 toxicity E. Monitor acid/base balance 5 1. If the pH shows acidosis 2. PaCO2 rises to ≥ 55 3. PaCO2 rises gradually with each blood gas, may indicate mechanical ventilation X. Weaning CPAP A. Monitor blood gases: PaO2 above 60 and CO2 below 55 B. First wean the FiO2 C. Once the FiO2 is down to 40%, start to wean the CPAP by increments of 1-2 cwp D. Watch the PaO2 and SpO2 for oxygenation status improvement E. Monitor the patient for increased WOB or desaturations