BLOOD PLATELETS
advertisement
•
•
•
•
•
•
•
•
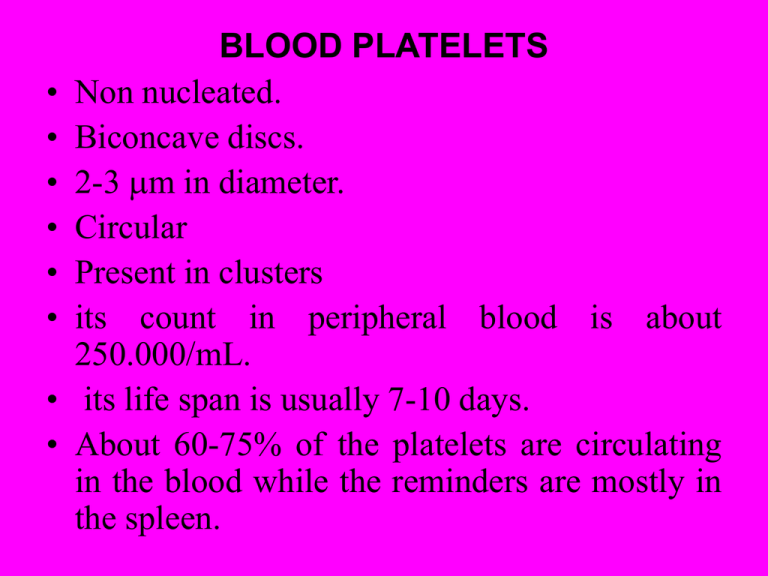
BLOOD PLATELETS
Non nucleated.
Biconcave discs.
2-3 m in diameter.
Circular
Present in clusters
its count in peripheral blood is about
250.000/mL.
its life span is usually 7-10 days.
About 60-75% of the platelets are circulating
in the blood while the reminders are mostly in
the spleen.
• Thrombocytosis: It is the increase in the
number of platelets, this occurs
physiologically in pregnancy and after
hemorrhage.
• Thrombocytopenia: It is the decrease in
the number of platelets, this occurs after
aplastic anemia, pernicious anemia, and
during menstruation.
• Thromboathenia: It is the decrease in
the functions of platelets.
The cytoplasm
The cytoplasm contains many active factors including:• Contractile proteins:
• A skeleton of microtubules
• Glycogen granules which are utilized for energy
production
• Lysosomes containing hydrolytic enzymes.
• endoplasmic reticulum and the Golgi apparatus which
which store large quantities of calcium ions.
• Mitochondria and enzyme system those are capable
of forming ATP and ADP.
• Enzyme system that synthesizes prostaglandin which
are local hormones those cause many different types
of vascular and local tissue reactions.
• Many granules:
• 2 types of granules
• A) Dense granules which contain non protein
substances such as ATP, ADP, serotonin and
calcium.
• B) Specific (alpha) granules: which contain
protein substances such as, fibrinogen, heparin
antagonist, (PF4) platelet derived growth factor
(PDGF), which stimulates wound healing through
stimulation of growth and multiplication of
vascular endothelial cells, smooth muscle cells and
fibroblasts.
Functions of platelet
• Haemostasis.
• Phagocytosis: viruses and antigenantibody complex are phagocytosed
by platelets
• Serotonin storage
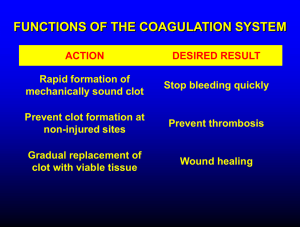
HAEMOSTASIS
• Haemostasis is the arrest of bleeding.
• Four major systems are involved
maintaining Haemostasis:• I- Vasoconstriction of blood vessels
in
• II- Platelets plug formation.
• III- facilitation if initial vasoconstriction.
• IV- Fibrin Forming system
- Vasoconstriction of blood vessels
1
The vascular system acts to prevent bleeding by:1- Contraction of vessels (vasoconstriction): and
reflex stimulation of adjacent vessels.
2- This reflex contraction is due to myogenic (direct
effect on the vessel wall) and due to
sympathetic stimulation.
3- Diversion of blood flow around damaged vessels
4- Initiation of contact-activation of platelet with
subsequent aggregation.
This mechanism may be sufficient to stop bleeding
from small vessel.
II- Role of platelets in haemostasis
• Platelets are intimately involved in primary
haemostasis, which is the interaction of
platelets and the vascular endothelium.
• The functions of platelets in haemostasis is
platelet plug formation.
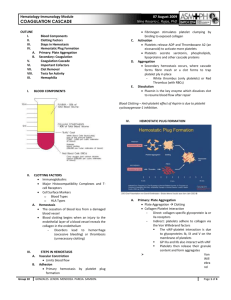
-Platelet Plug Formation
• Various processes are involved in the initial
formation of a platelet plug:• A- Platelet adhesion,
• B- Platelet release factors, and
• C- Platelet aggregation.
Adhesion and release factors
• Exposure of subendothelial connective
tissue, such as collagen fibers, initiates
platelet adhesion.
• When platelets adhere to the collagen they
swell up, becomes irregular and spread
radiating processes (pseudopodia).
• These pseudopodia, secret the contents
of various intracellular granules.
• These
secreted
substances:
ADP,
thromboxane A2, collagen, restocetocin and
cathepsin G……..ect
Aggregation
• These released substances stimulate other platelets
to adhere to the first one and causing platelet
adhesion.
• During platelet aggregation, the injured platelet
changes shape from discoid to spherical with
pseudopodia formation.
• Initial aggregation of platelets is caused by
adenosine diphosphate (ADP), which is released
from adherent platelets or endothelial cells.
• This aggregates forming a mass or plugs and seals
the injured sites.
• Platelet plug can`nt support stoppage of
bleeding in large arteries.
Coagulation of blood
• It is a process by which fluid blood is
converted into a semi-solid jelly like mass
called a clot.
• It is a process of plasma {many coagulation
proteins normally present in the plasma in an
inactive state (coagulation factor) mediate
this system}.
• It started by formation of prothrombin
activator as a result of vascular injury.
• Coagulation process is an enzyme cascade
and it is a complex phenomena.
• Coagulation process involves a series
of biochemical reactions, one reaction
trigger (activate) the next.
• This means the activation of one
clotting factor leads to activation of
the next factor.
• This
process
requires
plasma
proteins as well as phospholipids and
calcium.
• The clotting factor are listed blow:
•
•
•
•
•
•
•
•
•
•
•
•
•
F I fibrinogen
F II prothrombin
F III tissue factor
F IV calcium
F V labile factor
F VI not present
F VII stable factor
F VIII antihaemophilic factor
F IX Christmas factor
F X Stuart power
F XI factor XI plasma thromboplastin
F XII Hageman Factor.
F XIII fibrin stabilizing protein
• The formation of prothrombin activator depend
upon two pathways:
the extrinsic pathway and
the intrinsic pathway,
• Both of which share specific common
coagulation factors with the common pathway.
• Both pathways require initiation, which leads to
subsequent activation of various coagulation
factors in a cascading, waterfall.
• According to the cascade theory, each
coagulation factor is converted to its active form
by the preceding factor in a series of
biochemical chain reaction
EXTRINSIC PATHWAY
• When blood is exposed to tissue extracts,
blood clotting is rapidly initiated via the
extrinsic pathway by the interaction of tissue
factor (glycoprotein) and FIII (thromboplastin).
• tissue factor in presence of Ca++ combine with
factor VII and activate it.
• Activated factor VII in presence of Ca++
activate factor X.
• The activated factor X in the presence of
tissue phospholipids form prothrombin
activator.
INTRINSIC PATHWAY
• The intrinsic pathway starts when blood comes in
contact with foreign surface (exposed collagen from
blood vessel wall), factor XII activated and platelet
factor III released.
• Activated factor XII in the presence of Ca++ activate
factor XI which in turn in presence of Ca++ activate
factor IX which in turn in presence of Ca++ activate
factor VIII.
• In the presence of Ca++ activated factor VIII activate
factor X.
• Activated factor X in the presence of platelet factor
III form prothrombin activator.
COMMON PATHWAY
• The common final pathway involves the
conversion of:– Prothrombin (Factor II) to thrombin in the
presence of prothrombin activator.
– Thrombin in the presence of Ca++ convert
fibrinogen to a soluble fibrin (threads of fibrin)
– Soluble fibrin in the presence of Ca++ and FXIII
form insoluble fibrin clot (Mesh).
– This mesh entrap RBCs, WBCs and platelet to
form clot.
– The blood clot adheres to the injured vascular
walls and plugging it permanently.
Extrinsic Pathway
• (1-6 minutes)
Intrinsic Pathway •
(15 seconds)
Fate of the clot
• Few minutes after formation of the clot, the clot start
to shrink and release serum.
• This process is supported by platelet which adhere
to clot thread and extent their pseudopodia, which
contract and pull the fibrin thread close to each
other.
• Retraction the clot makes it firm & pulls the vessel
wall close to each other.
• The clot start to lysis after formation of fibrous tissue
which grow into the blood clot and permanently
seals the opening in the blood vessel.
• The clot is removed by protolytic enzymes
plasminogen which is converted to plasmin.
• Plasmin dissolve the clot, which in turn removed by
reticulo endothelial system.
Factors affecting clotting
• Factors preventing clotting
– Low temperature.
– Contact with non water
wettable surface (silicnized)
– Use of anticoagulant which
remove Ca++ ions from blood
(potassium oxlate, sodium
citrate)ز
– Use substances of biological
origin:•
•
•
•
Ptotamin.
Peptones.
Hirudin.
Dicumarol.
• Factors increasing clotting
– Warm.
– Contact with water wettable
surface.
– Injection of vit. K (for
promotion of factors II, VII, IX
and X)
Coagulation disorders
• Bleeding disorders
– Decrease fibrinogen
– Decrease prothrombin
– Decrease platelet
purpura
- Decrease clotting factors
hemophilia
• Intravascular clotting
– Thrombosis; it is a
blood clot which is
formed within blood
vessel.
– Embolus: it is a part
detached from the
clot
and
move
through
the
circulatory
system
and block
blood
vessel.
Anticoagulants
These are substances which are used to prevent
blood clotting inside the blood vessel or in test
tubes:Anticoagulant in vitro
These are substances used to prevent blood clotting
outside the body: • 1- Precipitation of Ca++ ions (inactivation of
calcium) by addition of sodium oxalate,
ammonium oxalate or sodium citrate.
• 2- Collection of blood in a siliconized non-wettable
electropositive charged container, which prevent
activation of factor XII and platelets.
• 3- Addition of heparin.
Anticoagulant in vivo
• These are substances used to
prevent blood coagulation inside the
body e.g. treatment of intravascular
thrombosis:– 1- Heparin.
– 2- Oral anticoagulant likes dicumarol.
1- Heparin: •
• It is a sulfate mucopoly-saccharide
with strong acidic properties.
• Mast cells and basophil leukocytes
form it.
• It is released into the general
circulation in minute amounts to
prevent any tendency of the blood to
clot inside the blood vessels.
• It is given by intravenous route.
Action of heparin:
• 1- It activates antithrombin II
• 2- It inactivates factor IXa, Xa, XIa, XIIIa
and thrombin.
• 3- It acts as a co-factor for lipoprotein
lipase, thus it clears blood from
lipids after meals.
• 4- It’s antidote is protamine sulphate
which is given to counteract the
high doses of heparin, where it
combine with heparin to neutralize
its action.
2- Dicumarol
• It is of plant origin, it inhibits
vitamin K.
• its
action
is
through
the
prevention of the formation of
prothrombin, factors VII, IX and X.
• - It has a slow onset and long
duration of action.
• - Its antidote is vitamin k.
Abnormalities of Hemostasis
Conditions that cause excessive
bleeding in man:
A- hemophilia
B- purpura
C- Vitamin K deficiency
11) Thromboembolic conditions in
human being.
I)
A) Hemophilia
It is a congenital sex-linked recessive disease
transmitted by females to their sons who
manifest signs of the disease.
The disease is characterized by bleeding
tendency and prolonged clotting time (1-12
hours).
Types of Hemophilia
1- Hemophilia A: 85% of cases it is due to lack of FVIII.
2- Hemophilia B: 10% of cases it is due to lack of FIX.
3- Hemophilia C: it is due to lack of FXI.
B- Purpura
• It is a disease characterized by spontaneous small
hemorrhages in the skin and mucous membrane
(petichae).
• In purpura there are defect in vasoconstriction of the
cut vessel (decreased serotonin), deficient clot
retraction
(retractozyme)
and
poor
platelet
aggregation.
• The formed clot is soft and poorly retracts.
• There is prolonged bleeding time.
Types of purpura
• 1- Thrombocytopenic purpura: It is due to decrease in
platelet count.
• 2- Thromboasthenic purpura: The count is normal but
its function is abnormal.
C- Vitamin K deficiency
• Vit. K is very important for the formation
of clotting factors II, VII, IX and X in the
liver.
• In the absence of this vitamin, bleeding
tendency from insufficiency of these
clotting factors can occur.
• This condition occurs when there is a
liver disease or obstruction of bile duct,
which causes poor absorption of vitamin
k from the intestine due to absence or
decrease in the bile secretion.
11) Thromboembolic conditions in human being.
• It is the formation of blood clot inside
blood vessel.
• This condition usually occurs when
there is a slow blood flow e.g. after
delivery and operation.