(1) vascular constriction
advertisement
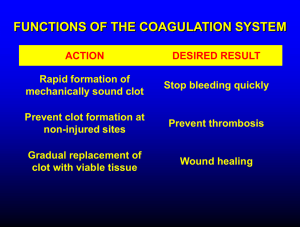
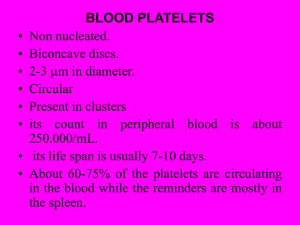
Hemostasis and Blood Coagulation Events in Hemostasis The term hemostasis means prevention of blood loss. Whenever a vessel is severed or ruptured, hemostasis is achieved by several mechanisms: (1) vascular constriction, (2) formation of a platelet plug, (3) formation of a blood clot as a result of blood coagulation, and (4) eventual growth of fibrous tissue into the blood clot to close the hole in the vessel permanently. Vascular Constriction Immediately after a blood vessel has been cut or ruptured, the trauma to the vessel wall itself causes the smooth muscle in the wall to contract; this instantaneously reduces the flow of blood from the ruptured vessel. The contraction results from (1) local myogenic spasm, (2) local autacoid factors from the traumatized tissues and blood platelets, and (3) nervous reflexes Mechanism of the Platelet Plug. When platelets come in contact with a damaged vascular surface, especially with collagen fibers in the vascular wall, the platelets themselves immediately change their own characteristics drastically. They begin to swell; they assume irregular forms with numerous irradiating pseudopods protruding from their surfaces; their contractile proteins contract forcefully and cause the release of granules that contain multiple active factors; they become sticky so that they adhere to collagen on the tissues and to a protein called von Willebrand factor that leaks into the traumatized tissue from the plasma; they secrete large quantities of ADP; and their enzymes form thromboxane A2. The ADP and thromboxane in turn act on nearby platelets to activate them as well, and the stickiness of these additional platelets causes them to adhere to the original activated platelets. Therefore, at the site of any opening in a blood vessel wall, the damaged vascular wall activates successively increasing numbers of platelets that themselves attract more and more additional platelets, thus forming a platelet plug. This is at first a loose plug, but it is usually successful in blocking blood loss if the vascular opening is small. Then, during the subsequent process of blood coagulation, fibrin threads form. These attach tightly to the platelets, thus constructing an unyielding plug Blood clotting ; Normally the blood remaine in its liquid form, as long as it remain in the vesseles .if drawn outside the body ,it thicken& form a gel. ,the gel eventually separates from the liquid . The straw – colored liquid called serum (it is blood plasmsa minus clotting protens. The gel is called a clot , it contain network of insoluble proteins fiber called fibrin in which the formed elements of blood are trapped . The process of gel formation called clotting or coagulation process. < is a series of chemical reactions that culminates in formation of fibrin threads. If clotting involve undamged vesseles the result is thrombosis. If blood takes long time to clot, haemorrage can occure. Clotting involve many factores called ,clotting (coagulation factors). . Clotting can be devided into 3 stages.; 1- intrinsic & exrinsic pathways. 2- prothrombinase convert prthrombine to thrombine . 3- thrombine converts fibringen to fibrin which form thread of clot. Extrinsic pathway; it occurs within seconds if the trauma is sever , tissue facter(TF) known as thromboplastin leaks from the cells of damaged tissue to the blood ( that’s why called (extrinsic).it intiate formation of prothrombinase . TF is mixture of lipoproteins & phospholipids , in the presence of Ca , TF , begins a sequences of reactions that ultimatly activate facter X , once activated it combimne with facter V & presence of Ca To form prothrombinase . Extrinsic pathway ; Intrinsic pathway :So called because its activatores are either in direct contact with blood or or contained within the blood . If endothelial cells become roughened or damaged , blood come in contactr with collagen fibers in the connective tissue.around the endotheium of the blood vessels, in addition trauma causes damage to the platelates( result in release of phospholipids), , contact with collagen fibers activate factor XII which begin asquences of reactions that eventually activate facter X..then it combine facter Vto form prothrombinase Common pathway : Prthrombinase with Ca catalyze the conversion of prothrombin to thrombin . Which inturn with Ca activate the conversion of fibrinogen to fibrin ( insoluble, thrombin also activate facter XIII whch strengthen & stabilizethe fibrin thread Thrombine has 2 +ve feed back : 1)Involve facter V , it accelerate the formation o prothrombinase which accelerate the production of more thrombin. 2) Activate platelateswhich reinforce their aggrigation & release of phopholipids. Common pathway Clot retraction ; Is the consolidation or lightening of fibrin clot , the fibrin thread attach to the damaged surface of blood cvessels,gradually contract as platelate pull on them. Normal contraction depend on numberr of platlate in the clot.. Role of vitamine K in clotting : It is required in synthesis of clotting facters , it is fat soluble & absorbed through the intestinal linnig , in people suffering from disorder in absorption of lipid , for eg. Due to iadequate release of bile will experience uncontrloed bleeding. Hemostatic control mechanism: The fibrinolytic system dissolves clots at a site of damage once the damage is repaired , dissolution of clot is called fibrinolysis when clot is formed , an inactive enzyme ( plasminogens) is incorporated in to the clot, both body tissue & blood contain substances that activate plasminogen to plasmin (fibrinolysin), it can dissolve clot by digesting fibrin thread . The clott is localised to the damaged tissue because of 1- fibrin absorbe thrombin to the clot., 2- the disperasal of clotting facter by blood. 3- release of prostocyclin by endothelial cell , which inhibit platelat adhesion & release. 4- anticoagulants : antithrombin, heparin , activated proteins. Intravascularv clotting : Sometimes , clot formed within CVS , such clot may be intiated by roughened endothelial surface (due to trauma, infection , atherosclerosis), these conditions induces adhesion of platelates , or when blood flows slowly allowing clotting factores to accumelate locally in high concntration to intiate coagulatiobn . Clotting in unbroken blood vessel called thrombosis., if the thrombus remain intact it may disloged & sweptaway in the blood , ablood clot , bubbes of air , fat from broken bone or a piece or debris transported by the blood stream called embolus , when emblus lodges in the lung calle pulmnary embolism.