Respiratory system
advertisement

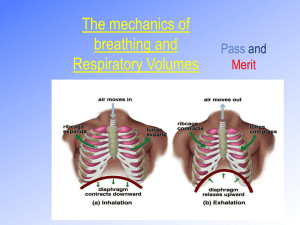
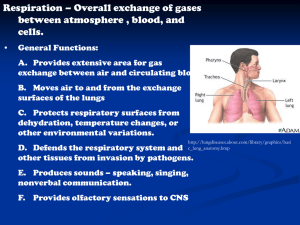
Respiratory system: anatomy & physiology Kaiu Prikk 2009 autumn The respiratory system: TWO LUNGS, CONDUCTING AIRWAYS Upper airways: nose, mouth, larynx, pharynx Lower airways: trachea, right & left main bronchi, secondary bronchi, bronchioles, alveoli Basic functions of respiratory system: 1. Air distributor 2. A gas exchanger O2, CO2, warming and humidifying 3. Acid-base balance 4. Phonation 5. Pulmonary defence & metabolism Respiration is an important homeostatic mechanism Defense Mechanisms of respiratory system The average person (moderately active) during the daytime breathes about 20,000 liters air/ 24 hours •small particles < 3 to 5 microns in diameter penetrate to the deep lung. Lung defence mechanisms: 1. Structural protection: hears in the nose, cilia in the upper and lower airways (trap and remove foregin bodies form airways) 2. Mucosal lining fluid upper and lower airways: warms and humidifies air 3. Irritant receptors in the nose and airways (recognize injurious agenst sneeze or cough reflex 4. Immune protection: respiratory tract mucosa and macropahges in alveoli Pulmonary ventilation & Control of Breathing Respiratory rate at rest is 15/per minute Pulmonary ventilation is the exchange of air between the atmosphere and the lungs. Breathing process: -automatic -controlled subconsciously by the respiratory center at the base of the brain. People control their breathing for example during speech, singing, or voluntary breath holding. For example: an increased concentration of carbon dioxide is the strongest stimulus to breathe more deeply and more frequently. Conversely, when the carbon dioxide concentration in the blood is low, the brain decreases the frequency and depth of breaths Respiratory Centers 1. The primary respiratory center: medulla Function: stimulation of basic inspiration for about 3 seconds and then basic expiration for about 2 seconds (5 sec/breath= 12 breaths/min). 2. Secondary respiratory center: pons contains 1) the pneumotaxic respiratory center; 2) the apneustic respiratory center. Function: Secondary respiratory center: modifies the basic respiratory rate The pneumotaxic respiratory center inhibits inspiratory time and increases breaths per minute. The apneustic respiratory center has not been clearly defined, (is postulated to prolong inspiratory time and reduces breaths per minute). Respiratory centers in the brain stem Respiration: 1. External respiration is gas exchange between the lung alveoli and the blood of the pulmonary circulation. This process depends on: 1) gas partial pressure differences; 2) the integrity of lung membranes, 3) blood flow in and out of the lungs. 2. Internal respiration is the exchange of gas between the blood and the cells of the body. This process generally depends on the same factors as external respiration Movement of gases between the alveoli, blood and cells depends on the partial pressure difference of a gas across these regions. According to the Law of Diffusion, gases always move from a region of high partial pressure to a region of low partial pressure. If your lungs have a higher gas pressure than your blood, then the gas will move into your blood and visa versa Respiration: 1. Quiet A.Quiet inspiration: The diaphragm contracts: causes an increase in volume of the thorax and the lungs which causes a decrease in pressure of the thorax and lungs air to enter the lungs, moving down its pressure gradient. B. Quiet expiration: The diaphragm relaxes The elasticity of the muscle tissue and of the lung stroma causes recoil returns the lungs to their volume before inspiration the reduced volume causes the pressure in the lungs to increase air leaves the lungs due to the pressure gradient. . 2. Forced A. Forced inspiration: Other muscles aid in the increase in thoracic and lung volumes. The scalenes - pull up on the first and second ribs. The sternocleidomastoid muscles pull up on the clavicle and sternum. The pectoralis minor pulls forward on the ribs. The external intercostals are especially important because they spread the ribs apart, thus increasing thoracic volume. It's these muscles whose contraction produces the "costal breathing" during rapid respirations B. Forced Expiration: The muscles aid in reducing the volume of the thorax and lungs: The internal intercostals - these compress the ribs together The abdominus rectus and abdominal obliques: internal obliques, external obliques- these muscles push the diaphragm up by compressing the abdomen. The work of breathing is done by the diaphragm, intercostal muscles, the muscles in the neck, and the abdominal muscles. When the diaphragm contracts and moves lower, the chest cavity enlarges, reducing the pressure outside the lungs. To equalize the pressure, air enters the lungs. When the diaphragm relaxes and moves back up, the elasticity of the lungs and chest wall pushes air out of the lungs Muscles of inspiration and expiration Gas exchange Air movement into and out of the lungs results: 1) differences in pressure brought about by changes in lung volume. Inspiration: intrapulmonary pressue < atmospheric presssue Changes in lung volume occur due to muscle contractions in the thorax and diaphragm Ventilation is influenced by the physical properties of the lungs: • compliance • elasticity • surface tension Compliance: the tendency of the lungs to expand, is due to the pulling action exerted by the pleural membranes. Expansion is also facilitated by the action of surfactant in preventing the collapse of the alveoli. Surface tension: action of surfactant Elasticity or recoil: is the process by which the lungs return to their original or resting volume. Elasticity is due to the elastic stroma of the lungs and the series elastic elements of the respiratory muscles, particularly the diaphragm. Ventilation - Inspiration Ventilation - Expiration Alveolus and gas exchange Respiratory regulation: Normal values exchange rates of O2 and CO2 at the tissues and in the lungs must be equal: •High pCO2 levels increase O2 dissociation in peripheral tissues •Low pO2 causes alveolar capillaries to constrict & send blood to lobules with high pO2 •High pCO2 levels cause bronchodilation to occur increasing airflow, reverse Changes in depth and rate of respiration are regulated by brain centers Normal Blood Gases Arterial pH 7.35 - 7.45 PaO2 80 to 100 mm Hg (The partial pressure of oxygen that is dissolved in arterial blood) PaCO2 35-45 mm Hg (The amount of carbon dioxide dissolved in arterial blood. Measured. Partial pressure of arterial CO2.) SaO2 95% to 100% (The arterial oxygen saturation) B.E. –2 to +2 mEq/lite (The base excess indicates the amount of excess or insufficient level of bicarbonate in the system. A base excess > +3 = metabolic alkalosis a base excess < -3 = metabolic acidosis HCO3 22 to 26 mEq/liter (21–28 mEq/L) The calculated value of the amount of bicarbonate in the bloodstream Hypoventilation: the state in which a reduced amount of air enters the alveoli in the lungs resulting in decreased levels of oxygen and increased levels of carbon dioxide in the blood. Hypoventilation can be due to breathing that is too shallow (hypopnea) or too slow (bradypnea) or to diminished lung function. Hyperventilation: is excessive ventilation of the lungs, beyond what is required to achieve normal arterial blood gases For example: Rapid or deep breathing in infection, bleeding, or heart attack Hyperventilation: -has little effect on arterial pO2 - no effect on oxygen saturation - main effect is to lower pCO2 and produce a respiratory alkalosis and secondary hypocalcaemia Causes of hyperventilation: 1. Disordered blood chemistry with normal homeostatic response to stimulate the brain's respiratory centre, increasing rate and depth of breathing. 2. Voluntary and conscious act. 3. Psychological response to anxiety or stress, with little awareness. Dyspnea: Difficult breathing; shortness of breath. Dyspnea is a sign of serious disease of the airway, lungs, or heart. (Resting) Tidal Volume (TV): This is the volume of air taken into the lungs when you inhale. Tidal volume increases with exercise or activity. Residual Volume (RV): is the volume of air left in the lungs at the end of maximal expiration (ie. the volume of air which you cannot voluntarily exhale from your lungs). Vital Capacity (VC): is the volume of air expelled from the lungs during a maximal forced expiration strating after a maximal forced inspiration. Total Lung Capacity (TLC): The residual volume (air you cannot expire) + vital capacity (total volume available for use) = total lung capacity. Inspiratory Reserve Volume (IRV): Total lung capacity minus the volume of air in the lung at the end of a normal inspiration. Expiratory Reserve Volume (ERV): .is the volume of gas that is expelled from the lungs during a maximal forced expiration that strats at the end of normal tidal expiration Functional Residual Capacity: is the total volume of air left in the lungs at the conclusion of normal, resting expiration. This value includes the expiratory reserve volume plus the residual volume (ERV + RV). Forced Expiratory Volume 1 (FEV1): the volume of air that can be expired during the first second of expiration in a vital capacity determination.... generally about 80% of VC. Forced Expiratory Volume 1 (%) or FEV1(%): FEV1/VC, expressed as %, normal value >70% expressed as a percentage ratio PEF - peak expiratory flow rate - the peak flow rate during expiration Lung function tests or PFTs -evaluate how well your lungs work. 1. 2. 3. 4. 5. 6. 7. Spirometry Diffusion test Body plethysmography Inhalation challenge tests Cardiopulmonary exercise test Six-minute walk test A peak flor meter or PEF (A home lung function test uses a peak flow meter) 8. Blood Gas analysis . Spirometry: -is the first lung function test done. - detect the presence of lung disease. Spirometry is recommended as the “Gold Standard” for diagnosis of obstructive lung disease by: National Lung Health Education Program (NLHEP); National Heart, Lung and Blood Institute (NHLBI); World Health Organization (WHO) The lung function values measured with spirometry are: Forced vital capacity (FVC). This measures the amount of air you can exhale with force after you inhale as deeply as possible. Forced expiratory volume (FEV). This measures the amount of air you can exhale with force in one breath. The amount of air you exhale may be measured at 1 second (FEV1), 2 seconds (FEV2), or 3 seconds (FEV3). FEV1 divided by FVC can also be determined. Forced expiratory flow 25% to 75%. This measures the air flow halfway through an exhale (FVC). Peak expiratory flow (PEF). This measures how quickly you can exhale. It is usually measured at the same time as your forced vital capacity (FVC). Slow vital capacity (SVC). This measures the amount of air you can slowly exhale after you inhale as deeply as possible Spirogram Pred Act1 %Soll VC IN (L) 2,94 2,17 73,8 FVC (L) 2,96 1,99 67,3 FEV1 (L) 2,52 1,40 55,3 FEV1 % VC MAX (%) 79,41 64,20 80,8 PEF (L/S) 6,27 4,76 75,9 Body plethysmography : To measure total lung capacity (TLC), RV, airway resistance Diffusion test or transfer test: measures how well your lungs transfer a small amount of carbon monoxide (CO) into the blood. Diffusing capacity provides an estimate of how well a gas is able to move from your lungs into your blood. Atrerial blood gases analysis: to determine the amount of oxygen and carbon dioxide in your bloodstream. Cardiopulmonary exercise testing - is a non-invasive and objective method of evaluating both cardiac and pulmonary function Airway obstruction & restriction Airway obstruction Forced expiratory volume (FEV1) Lower with higher FEV2 and FEV3 FEV1 divided by FVC Lower < 70% Forced expiratory flow 25% to 75% Lower Peak expiratory flow (PEF) Lower Total lung capacity (TLC) (VT) Normal or higher Slow vital capacity (SVC) Normal or lower Functional residual capacity (FRC) Higher Residual volume (RV) Higher Expiratory reserve volume (ERV) Normal or lower RV divided by TLC ratio Higher Airway restriction Forced vital capacity (FVC) Lower than predicted value Forced expiratory volume (FEV1) Normal or lower with higher FEV2 and FEV3 FEV1 divided by FVC Normal or higher Forced expiratory flow 25% to 75% Normal or lower Peak expiratory flow (PEF) Normal or higher Total lung capacity (TLC) (VT) Lower Slow vital capacity (SVC) Lower