Bed Shortage Resolution
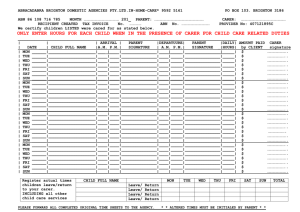
advertisement

Patient Flow Management System at Parker Adventist Hospital Jason Makaroff – Director of Process Improvement Jennette Bergstrom – Director of Acute Care Services Brandon Robertson – Administrative Resident Contents • • • • Introduction Patient Flow Committee Current State/Symptoms/Approach Solution: Patient Flow System – Structured Framework – Forecasting: Data Driven Decision Making – Daily Operations – Next Steps: Adding Granularity Patient Flow Committee: Mission Mission To design a process that promotes the flow of patients through the organization such that a patient’s hospital experience feels safe, timely, efficient and proceeds with minimal delays with bed utilization optimized. Patient Flow Committee: Objectives 1. Optimize utilization of existing patient beds (capacity) and associates caring for patients while providing the safest possible care. 2. Avoid diversions/transfers for patient safety, patient, physician and associate satisfaction and to promote organizational growth & viability. 3. Ensure compliance with regulatory guidelines and requirements for patient flow. 4. Establish (data/reports) infrastructure for real-time monitoring of organization capacity and demand for utilization by all appropriate managers that will provide guidance for optimal staffing. 5. Develop and establish methods e.g. guidelines/protocols/algorithms and mechanisms to facilitate appropriate patient flow. 6. Facilitate collaboration within the facility for PI projects, monitoring, and opportunities for improvement. 7. Celebrate Success! Current State • Frequent Bed Shortages in Acute Care Services • Highly Stressful, Reactive Environment • No Defined Processes for Managing Capacity vs. Demand • No Ability to Plan Ahead • Delays in Discharges on the Floor Due to Uncoordinated Resources Symptoms • Long delays in the Emergency Department • Excessive PACU Hold Times • No beds available for patients coming out of surgery • Average TAT for discharges is greater than 3 hours • Discharge orders being written late morning/early afternoon Understanding the Patient Flow Patterns Admits: 1st Flr vs. 2nd Flr Emergency department admissions influenced by natural variation. 11 10 Quantity of Admits Surgery Schedule influenced by artificial variation. 9 8 Admits 1st Floor 7 Admits 2nd Floor 6 Admits 2nd Floor Goal 5 4 3 Monday Tuesday Wednesday Thursday Friday Weekday Data indicates potential for bottlenecks to occur on Mondays and Tuesdays. Discharges: 1st Flr vs. 2nd Flr Quantity of Discharges 10 9 8 DCs 1st Floor 7 DCs 2nd Floor 6 DCs 2nd Floor Goal 5 4 3 Monday Tuesday Wednesday Weekday Thursday Friday Understanding the Patient Flow Patterns Inpatient Elective Surgery Schedule Fluctuations 3/15/2010 - 4/27/2010 14 12 Number of Cases 12 10 10 8 10 9 10 9 9 9 8 8 7 6 6 6 5 4 5 4 5 5 4 4 4 3 2 2 2 4 3 3 2 1 1 Mon Tue Wed Thu Fri Mon Tue Wed Thu Fri Mon Tue Wed Thu Fri Mon Tue Wed Thu Fri Mon Tue Wed Thu Fri Mon Tue Wed Thu Fri Mon Tue 0 12 11 Day of Week Highly variable elective surgery schedule makes it difficult to plan resources effectively and the hospital environment becomes more reactive than proactive. Approach • Develop & implement a plan for managing demand and capacity real-time. • Move the organization from being reactive to pro-actively responding to peaks in demand with regards to patient flow. Patient Flow System Managing Demand and Capacity Real-time. 1. Define facility-wide definitions for capacity and demand. • • Capacity Levels defined for Green, Yellow, and Red Efficient Capacity defined as 85% or less of maximum beds available Green: 85% of Efficient Capacity or Less Yellow: Between 85 and 95% of Efficient Capacity Red: Greater than 95% of Efficient Capacity • • • 2. • Working with clinical and ancillary support departments, define operational policies for each department that are dependent on the current level of demand vs. capacity. Defined policies and procedures for operating in green, yellow, and red capacity status levels. • Department specific operational functions for each capacity level • Defined standardized procedures for Administrative Managers and staff to conduct bed meetings. • Provide structured mechanisms for standardizing report out in bed meetings. • Provide focal point for Admin Managers to direct resources in relation to capacity and demand levels. 3. 1. 2. 3. 4. Define policies for Discharge Lounge and Overflow Areas for use during Yellow and Red Capacity Status events. Define policies for discharge lounge and overflow activation. Designate physical location and staffing for discharge lounge. Train Admin Managers on implementation of discharge lounge and overflow areas. Educate staff on discharge lounge usage and overflow area procedures. 4. 1. 2. 3. Define hospital-wide communication plan for Capacity Status Admin managers determine hospital’s capacity status based on current surgical schedule and planned discharges coupled with 90 days of historical data on patient volume. PBX operator is notified by Admin Manager to send house-wide communication of capacity status via pager and VOIP phones. Unit Secretaries and department leaders update capacity signage on each unit to reflect current state of capacity status house-wide. 5. 1. 2. 3. 4. 5. 6. Create marketing and training materials to promote cultural change and hardwire the process into the organization. Health stream module developed to train all organization leaders on the concepts of the Patient Flow System. Logo for Patient Flow System designed and used on all materials related to patient flow for associate recognition and acceptance. Discussion on Patient Flow System integrated into Employee forums through flyers mailed to associates residences and presentation in forum. Rounding logs created for hard-wiring the process into the organization. Rounding conducted on leaders. Rounding to be scheduled for associates. Patient Flow System: Forecasting 1. Develop tools for predicting current day forecast for admissions and discharges. 2. Integrate forecasts into day to day operations. Patient Flow System: Forecasting • Predictive ability: >75% • Uses data sources from MEDITECH and utilized by Admin Managers • Has the ability to forecast the current day’s capacity status color thereby initiating multiple house-wide processes Lessons Learned Lessons Learned • • • • • • • • • Adding a night-time bed meeting at 2230 hours is effective for preparing for next day discharges. Acute Care Services director position overseeing all areas of acute care has helped to promote best practices in each area (ICU, Gen/Surg, Med/Tele). Spread strategy for implementing Patient Flow System is effective. Discharge Lounge helps reduce the number of delayed discharges. Strong executive sponsorship is required to be successful. Data is available, but obtaining it in a usable format is challenging. Patient safety has increased. Opportunities exist for creating tools that allow forecasting for staffing Challenges hospitalists to work harder and more efficiently. Patient Flow System: Next Steps • • • Add more standardization around bed meeting report outs Next version of Patient Flow System will increase granularity and manage capacity on a department level. Future plan of Patient Flow System is to automate forecasting by pulling data from the enterprise database and building a forecasting tool for My Virtual Workplace. • • • • • Develop tools for predicting one week forecasts based on historical data pulled from Centura’s data repositories. Integrate forecasts into day to day operations to provide operational direction for ancillary departments based on anticipated volume. Provides a foundation for building staffing models based on historical data. Update policies with suggestions for increasing process efficiencies in ancillary and clinical departments during each capacity level. Patient Flow Dashboard with graphics that track metrics on Patient Flow in each department. (draft example) “Well done is better than well said.” -Benjamin Franklin