Bone Physiology
Bones are Classified by shape and structure
limbs
Carpals
tarsals
vertebrae
Skull bones
Ribs
Sternum
scapula
Epiphysis
Epiphyseal Line
Diaphysis
Periosteum
Articulating Cartilage
Compact Bone
•
•
•
•
Canaliculi
Haversian Canal
Lamellae
Osteon
Another picture of Compact Bone
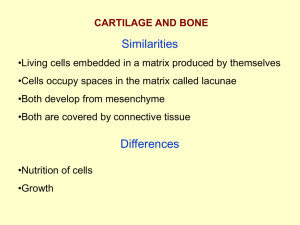
Spongy Bone
Located along the epiphyses of long bones
Site of Erythrocyte (RBC) formation
Collagen fibers are not arranged in concentric rings. But the lamellae form
rods called
. No Osteons or Haverian Systems are present.
Cells in Bones
– mature bone
cells; recycle Ca and PO4
– dissolve
bone by secreting enzymes
and acids. Release Ca to
be returned to blood
stream
– cells that
produce new bone cells
referred to as osteogenesis
Osteoclasts remove matrix,
osteoblasts adds matris.
When an osteoblast’s
lacunae is calcified the cell
becomes and osteocyte.
Endochondrial Ossification
• Bone tissue in a fetus begins as hyaline cartilage
• Inside is cartilage, cartilage becomes ossified.
• In 6 weeks cartilage is replaced to bone except at
growth plates.
In 6 weeks cartilage is replaced to bone except at growth plates.
Longitudinal Growth at the
Epiphyseal line
• Two growth plates
– Composed of
hyaline cartilage
– Longitudinal growth
is completed when
epiphyseal lines
become completely
ossified.
• Chrondroblasts closest to epiphyses begin
to undergo cell division
• Cells enlarge (hypertrophy)
• Cells die, bone eventually replaces
cartilage (invasion zone)
Resting
Zone
Mitosis
Zone
Hypertrophy
Zone
Ossification
Zone
• Resting Zone
Mitosis Zone
Maturation/Hypertrophy Zone
• Ossification Zone
Longitudinal Growth
• Controlled by 3 hormones
– Growth Hormone
• Baby to prepuberty
– Sex Hormones (estrogen/testosterone)
• Causes growth spurt at puberty
• Shapes your skeleton to your sex
– Thyroid Hormones (PTH & Calcitonin)
• PTH = parathyroid hormone
• Controls whether bone growth occurs
• Affects Appositional Growth – bone growth in
diameter
Bone Homeostasis
Bone Remodeling
• Osteons are formed by osteoblasts
• In healthy adults:
– Bone deposit = bone resorption
– Osteoblasts = Osteoclasts
• Bone Remodeling refers to the regular
mineral turnover that occurs in bone.
• In adults, 18 % of proteins and minerals
turns over yearly. Not uniform. I.e. Head
of femur is remodeled more. Why?
Bone Remodeling
Controlled by Negative Feedback Loop
• Bone Deposit
– Occurs where bone is
injured or added bone
strength is required
– Deposits Ca+2 into
bone
• Bone Resorption
– Osteoclasts break down
bone
– Calcium is taken from
bone and placed into
blood stream
– Lysosomes assist in the
process
– Ca and PO4 are
released; eventually
releasing the blood
stream
Bone Remodeling is controlled by 2 hormones by
a Negative Feedback Loop
• Blood Calcium is the original stimulus
• Normal Blood Ca is 9-11 mg CA/100 ml of
blood
• When blood Ca decreases (< 9 mg)
Parathyroid Hormone (PTH) is released
into bloodstream.
• Bone resorption occurs causing Ca to
leave bone and goto the blood stream
• Osteoclasts are working
High levels of blood Ca (>11mg)
• When blood Ca levels are high, Calcitonin
is released.
• Causes bone deposit to occur
• Ca from the blood is stored into bone.
• (Osteoblasts and Osteocytes are working.)
• 99% of all Ca is found in bone.
• Osteoclasts
cause bone
resorption
– Controlled
by PTH
• Osteoblasts
cause bone
deposit
– Controlled
by calcitonin
• Vitamin D – aids in the absorption of Calcium into
the bone. Part of vitamin D is converted to the
hormone calcitriol which allows Ca to pass through
the S.I.(What food is Vitamin D fortified?)
i.e. rickets results from Vitamin D deficiency
• Vitamin C – helps osteoblasts function
i.e scurvy – caused from a reduction in osteoblast
activity
• Calcium tablets • Diet -
2nd Response to Regulating Bone
Remodeling
• Wolff’s Law
– Bone grows or remodels in response to the
forces or stresses placed on it.
– Appositional growth – growth in diameter is
controlled by the amount of mechanical stress
and gravity placed on the bone
– Heavy usage leads to heavy bones; nonuse
leads to atrophy (bone loss)
Controlling Bone Remodeling
• Hormones PTH and Calcitonin determines
whether and when bone remodeling
occurs.
• Mechanical Stess determines where
remodeling occurs. High stress areas
grow appositionally.
• Body’s Needs for Calcium
– Transmit nerve impulses
– Muscle contractions
– Blood coagulation
– Cell division
If blood Ca levels are low for an extended
time, bones continually lose Ca.
Once bone density loss begins, women
lose 8% of their bone mass every
decade, men lose 3% every decade
Osteoporesis
• Osteoporesis
• Normal Bone
Risk Factors
Sex (females more affected than
males; especially after menopasue)
Insufficient exercise or too much
exercise
Poor diet (low in Ca and protein
Smoking
Race: Black > bone density
Change in Bone Density with Age
Bone Fracture and Repair
• Simple Fractures take
8-12 weeks to heal
• Healing time
increases age due to
poor circulation
Phases of Bone Repair
– A mass of clotted
blood appears
– Blood vessels
hemorrhage, causing
internal bleeding
– Blood pools and clots
around fx area; which
closes off injured
blood vessels
• Macrophages invade and
clean area
• Fibroblasts help form
chondroblasts and
collagen fibers
• Helps to form cartilage
splint that will connect
ends of broken bones
• Osteoblasts
replace the
cartilage with
spongy bone
• Bone cells replace
cartilage from the
outside fx toward
the inside
• Cells are not
organized in the
bony callus
Continues 4 months to a year
Removes excess material; a layer of compact
bone is produced