The Revenue Cycle
advertisement
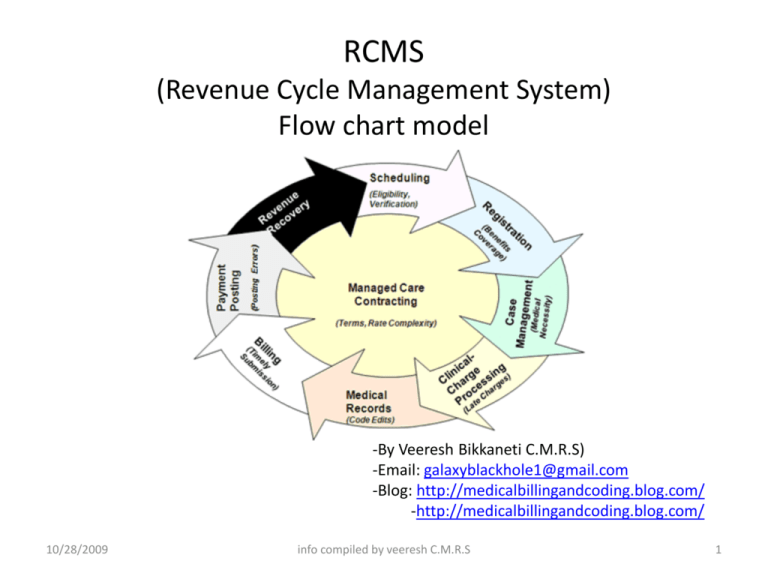
RCMS (Revenue Cycle Management System) Flow chart model -By Veeresh Bikkaneti C.M.R.S) -Email: galaxyblackhole1@gmail.com -Blog: http://medicalbillingandcoding.blog.com/ -http://medicalbillingandcoding.blog.com/ 10/28/2009 info compiled by veeresh C.M.R.S 1 New Employee •employee selects insurance payer •employer collects premium •employer pays premium to payer Pre-Visit •Patient makes appointment •Registration completed in system •Patient given office policies •insurance verified with payer •referrals & authorizations obtained. Contract •Finalize contract •educate practice on contract •Physician credentialing Check -IN/Visit •Patient pays co pays/ Bank Deductible •Insurance card copied •physician sees patient •payment posted to account •physician documents medical record •physician completes encounter form •Actual Vs. target reports •coding accuracy •payer performance Insurance & Patient Follow-Up •Account Follow-Up •Patient referred to collection agency •Credit balances resolved. Patient Medical Group Analysis & Reporting Employer Payer Charge Entry •Encounter Forms Audited •Charge entered into system •Charges scrubbed Payments •payer pays claims •Check and EOB received by Bank •Money deposited •Deposit reconciled at practice Denials •claim denied by payer •EOB received and posted •claim corrected •claim reset to payer Claims •claim Created •claim sent to payer •acknowledgment received. RCMS : Responsibility and Functionality Responsibility Functionality Administration Practice Registration coding Charge capture Reimbursement, Fees and credentialing Revenue cycle 10/28/2009 info compiled by veeresh C.M.R.S 3 RCMS : Responsibility and Functionality Responsibility Functionality Billing Office Billing Office Collection agency Claims transmission payment posting Insurance Follow- Up Patient Follow- UP Patient Collections Traditional “billing Office” Revenue cycle 10/28/2009 info compiled by Bikkaneti Veeresh C.M.R.S 4 RCMS : Responsibility and Functionality Responsibility Functionality Accounting finance reporting Revenue cycle 10/28/2009 info compiled by veeresh C.M.R.S 5 The Revenue Cycle: Billing Tasks Payer contracts Pre visit or Benefits determination Payer Rejections Front Desk Visit Edits Post the Visits & charge entry Billing & collections Reports & analysis 10/28/2009 info compiled by veeresh C.M.R.S 6 • Practices Need to Attend to Compliance issues though out the revenue cycle. • Billing process is often described as having both front End and back end. • As more care became “managed”, however, the End-to- End process evolved so that billing now starts, When the Patient calls to make an appointment. • All functions outlined below represent Reimbursement functions for the medical practice. Now this is clear that billing and collection is no longer only a back office responsibility. 10/28/2009 info compiled by veeresh C.M.R.S 7 Front end and back end billing functions Front End Functions Back End Functions Appointment scheduling Billing edits Registration(demographic and insurance) Claims to payers Check – in Process Account receivable follow-Up (by payer type) Check – Out Process Account receivable follow-Up (by payer type) Referrals and Pre-Authorizations Statement s to patients Coding Payment posting Charges Capture and entry Payment Variance Analysis Financial counseling Denials posting and resolution Cash at time of service Reporting results and analysis 10/28/2009 info compiled by veeresh C.M.R.S 8 Step1. Pre Visit Revenue cycle Business Pre-visit •Registration •Insurance verification •authorization Step2. Check-In Patient Check -in •Time-of-service payments •Real time system updates Provide service •Inpatient •Outpatient 10/28/2009 Step3. Charge Capture and Charge entry Service capture -Inpatient •Inpatient charge report •Hospital face sheet •Provider documents services •Provider identifies procedure and Diagnosis codes Service capture –outpatient •Outpatient charge report info compiled by veeresh C.M.R.S Review •Compare with provider schedule/contract with the payer •Missing charge reports •Hospital reports and logs •Audit coding to documentation 9 Charge entry •At site or central billing office •Daily recap balance Step4. claims process Generate and submit claim •Electronic or manual yes no review •Review edit report •Correct claim 10/28/2009 info compiled by veeresh C.M.R.S 10 Step 6&8 Follow –up and collections Transmit/mail claim •Electronic claim submission •Paper claim mailing Print confirmation report •Claims#, $ amount •Accepted , Yes/ No Account – Up and collections •Reviews outstanding A/R •Research /review •Request additional information •Resubmit/update claim No Step7. Denial Management Yes Open mail •Prepare batch. •Endorse checks •Prepare deposit. 10/28/2009 info compiled by veeresh C.M.R.S 11 Step5. payment posting Payment posting •Post batch. •Prepare secondary claims •Flag appeals, rejections, refunds. •Balance batch Yes Spend $$$$$$ No Research /review •Call provider relations •Follow instructions for appeal •Process refund •Continue to follow account 10/28/2009 info compiled by veeresh C.M.R.S 12 Thank you 10/28/2009 info compiled by veeresh C.M.R.S 13