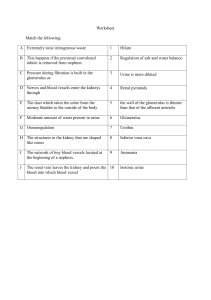
THE URINARY SYSTEM THE URINARY SYSTEM Urinary system consists of: Two kidneys Two Ureters The Bladder The Urethra GENERAL FUNCTION OF THE KIDNEYS Kidneys are organs that: Filters plasma and plasma constituents from the blood – filtrate Then selectively reabsorb water and useful constituents back from the filtrate. Ultimately excreting excesses and plasma waste products LOCATION OF THE KIDNEYS Located in the dorsal part of the abdominal cavity on each side of the aorta and vena cava just ventral to the first few lumbar vertebrae. In ruminants (filled rumen) the left kidney maybe pushed to the right as far as the medial plane or beyond. Thus, much more loosely attached to the body wall than the right kidney, and consequently the left renal artery and vein are longer than the right vessels. LOCATION OF THE KIDNEYS Kidneys are retro-peritoneal – located outside the peritoneal cavity. They are however more closely attached to the abdominal wall by fascia, vessels and peritoneum than other organs ANATOMY OF THE KIDNEYS Shape of the kidneys Somewhat bean-shaped in most domestic animals In cow the kidneys are lobulated Right kidney of the horse is heart shaped ANATOMY OF THE KIDNEYS Medial boarder of the kidney is concave and has a depression – renal hilus At the renal hilus – blood vessels and nerves enter Ureter and lymphatic vessels leave Expanded origin of the ureter within the kidney is called the renal pelvis Renal pelvis receives urine from the connecting tubules of the kidney. Cavity within the kidney containing the renal pelvis is called the renal sinus ANATOMY OF THE KIDNEY Medulla - portion of the kidney immediately surrounding the renal pelvis. It appears striated because of the radially arranged collecting tubules. These tubules form the basis for the renal pyramids which have their apices at the renal pelvis and their bases covered by the cortex. In addition to the collecting tubules, the medulla also contain the loop of henle. ANATOMY OF THE KIDNEY The Cortex – located between the medulla and the thin, connective-tissue capsule. Cortex has a granular appearance because of the large number of renal corpuscles Proximal convuluted tubules and distal convuluted tubules are also located in the cortex in close relation to the glomeruli and many loops of henle BLOOD AND NERVE SUPPLY TO THE KIDNEY BLOOD AND NERVE SUPPLY TO THE KIDNEY Blood supply is much more extensive than the size of the kidneys would suggest Two renal arteries may carry as much as 25% of total circulating blood. Renal arteries enters the hilus – divide into interlobar arteries Interlobar arteries pass peripherally between pyramids towards the cortex – forming arciform or arcuate arteries BLOOD AND NERVE SUPPLY TO THE KIDNEY Each arcuate artery – divide to form interlobular arteries which give rise to afferent arterioles Each afferent arteriole branches to form a capillary network called the glomerulus Efferent arterioles leaves each glomerulus – break up into capillary network that surrounds the rest of the nephron. BLOOD AND NERVE SUPPLY TO THE KIDNEY Arterioles leaving the glomeruli close to the medulla send branches directly into the medulla as arteriae rectae – these form capillary network around the collecting tubules and loops of henle Arcuate veins drain blood from the cortex and medulla – pass through the medulla as interlobar veins and enter the renal vein. Lymph drains from the kidney to the renal lymph nodes. BLOOD AND NERVE SUPPLY TO THE KIDNEY Kidneys are supplied with sympathetic nerves from the renal plexus, which follow the blood vessels and terminate largely on glomerula arterioles. Branches of the vagus nerve may also supply the kidneys. Both vasoconstrictor and vasodilator nerves are found in the kidneys URETERS Ureter – muscular tube that conveys urine from the pelvis of the kidney to the bladder. Each ureter passes caudad to empty into the bladder near its neck – area known as the trigone Ureter passes obliquely through the wall of the bladder – an effective valve is formed to prevent return flow of urine to the kidney. URINARY BLADDER Urinary bladder – hollow muscular organ – varies in size and position with the amount of urine it contains. Empty bladder – thick walled pear shaped structure located on the floor of the pelvis. Filled bladder – as it fills with urine, the walls become thinner and most of the bladder is displaced craniad toward the abdominal cavity. URINARY BLADDER Neck of the bladder is continuous with the urethra caudally – muscle of the bladder wall is arranged in a circular manner at the neck of the bladder – forming a sphincter that controls passage of urine into the urethra. TRANSITIONAL EPITHELIUM Pelvis, ureter, bladder and urethra are all lined with transitional epithelium. Important in these areas where distention of the lumen is required. Empty organ – lumen small – walls thick – lining epithelial cells are piled deeply to form a manylayered stratification. Distended organ – lumen enlarged – thinner walls – transition to a much lower stratification of the lining. URETHRA Pelvic urethra extends from the bladder to the ischial arch. In the male it receives the ductus deferens and the ducts from the accessory sex glands. The pelvic urethra continues as the penile urethra which transfers the urine to the outside MICTURITION Micturition – expulsion of urine from the bladder. Reflex activity, stimulated by distension of the bladder from constant intake of urine from the ureter. The bladder expands to gradual inflow of urine until the pressure becomes high enough to stimulate reflex center in the spinal cord. Contraction of the bladder wall occurs by way of the sacral parasympathetic nerves. Voluntary control of external sphincter surrounding the neck of the bladder prevents reflex empting. THE NEPHRON The nephron – unit of structure and function of the kidney It includes: Glomerulus Glomerular capsule (bowman’s capsule) Proximal convoluted tubule Loop of henle Distal convoluted tubule (which is continued by the collecting tubule) NEPHRON Glomerulus – tuft of capillaries interposed on the course of an arteriole. Glomerular capsule (Bowman’s capsule) – expanded blind end of the tubule which is evaginated around the glomerulus and almost entirely surround it. The visceral (inner) layer of the glomerular capsule closely surrounds the capillaries. The parietal (outer) layer of the glomerular capsule is continuous with the proximal convoluted tubule NEPHRON The complex of glomerulus and inner and outer layer of glomerular capsule is called a renal (malpighian) corpuscle. The space between the inner and outer layers of the glomerular capsule communicates with the lumen of the proximal tubule. Renal corpuscle is the major site for filtration of fluid from the blood. 100 times as much blood passes through the filter as is eventually excreted in the urine. NEPHRON Blood pressure is important for effective filtration Blood pressure in the capillaries of the glomerulus must remain relatively high Ensured by capillary being on the course of an artery rather than between artery and vein. Both afferent and efferent arteriole (entering and leaving the glomerulus respectively) have smooth muscle, constriction of one or both can be used to regulate amount of blood entering the glomerulus and the pressure within the glomerulus. NEPHRON Blood pressure Afferent arteriole (as it approaches the glomerulus) is surrounded by a cuff of myoepithelial cells that has characteristics of smooth muscle and epithelium – juxtaglomerular cells Juxtaglomerular cells – site of renin production which is secreted in the blood when: Blood pressure in the afferent arterioles falls Na concentration of the plasma decreases Distal tubular osmolarity decreases Sympathetic nerve fibers innervating the afferent arteriole are stimulated. NEPHRON Renin In the blood renin acts on an alpha globulin, angiotensinogen to produce angiotensin. Angiotensin acts as a vasoconstrictor to increase blood pressure Angiostensin also act on the adrenal gland to secrete aldosterone. Aldosterone acts on kidney to conserve sodium ions NEPHRON Each human kidney has approximately one million nephrons Only 25% of these function at a given time under normal conditions Relative constriction of afferent and efferent arterioles determine whether or not a specific nephron is functioning. NEPHRON Proximal convoluted tubule, loop of Henle and distal convoluted tubule are supplied by capillaries from the efferent arterioles. Blood in the efferent arteriole has lost 20% of its water, and is more concentrated (higher potential osmotic pressure) and therefore is better able to reabsorb water from the tubules. NEPHRON Proximal convoluted tubule Longest and most winding portion of the nephron Forms much of the tissue of the renal cortex Proximal tubule reabsorbs most of the constituents of the glomerular filtrate that are needed by the animal body – including 7/8 of the sodium chloride and water. Facilitated by the more concentrated blood. In addition to selective reabsorption from the glomerular filtrate – cells of the proximal segment are able to secrete waste products from the blood into the fluid passing through the lumen of the tubule. NEPHRON Henle’s loop Situated between the proximal convoluted tubule and distal convoluted tubule U-shaped tube that continues from the proximal tubule close to the glomerulus. Descending limb is thin – extends variable distance into the medulla where it turns back on itself as the thick ascending limb of the Henle’s loop. Thin limb – simple squamous epithelial lining Thick limb – cubodial epithelial lining NEPHRON Henle’s loop Contains the most concentrated fluid, with the highest concentration at the lowest part of the loop, close to or within the medulla – due to countercurrent mechanism Distal convoluted tubule Shorter and less twisted than the proximal Extends from the termination of the ascending limb of the Henle’s loop to the collecting tubule. NEPHRON Collecting tubules Initial collecting tubules – referred to as the arched tubules – empty into the straight collecting tubules in the cortex of the kidney. Straight tubules enter the medulla and unite to form papillary ducts which empty into the pelvis of the kidney Lining cells move from cuboidal epithelium in the arched tubules to columnar epithelium in the papillary ducts. FUNCTION OF THE KIDNEY Excretion of many waste products of the body. Excretion – removal of waste products of metabolism – waste products made by the body itself. Accumulation will prevent the maintenance of a steady state. Excretion is different from egestion and secretion. Egestion is removal of undigested food from the gut (defaecation) Secretion – release of useful substances e.g. hormones FUNCTION OF THE KIDNEY Maintenance of homeostasis – relative constant condition of the internal environment of the body. Water balance pH Osmotic pressure Electrolyte levels Concentration of many plasma substances Control is achieved by – filtration through the glomerulus – and re-absorption passively (osmosis and diffusion) or actively (tubular cell transport) FUNCTION OF THE KIDNEY Factors affecting the action of the kidneys include: Composition of the blood Arterial blood pressure Hormones Autonomic nervous system ULTRAFILTRATION Ultrafiltration – filtration under pressure. Occurs in the renal capsule Pressure derived from blood pressure (pumping pressure or hydrostatic pressure) Diameter of capillaries in the glomerulus is much less than that of the arteriole - pressure rises Water and small solute molecules are squeezed out of the capillary and into the renal capsule. Large molecules like protein, RBC, platelets are left behind in the blood ULTRAFILTRATION Epithelium of renal capsule Made up of cells highly modified for filtration – podocytes Fit together loosely leaving slits called slit pores or filtration slits (25 nm wide) – filtered fluid pass through these slits. Filtered fluid in the capsule is called the glomerular filtrate (GF) GF has chemical composition similar to that of blood plasma – glucose, amino acids, vitamins, ions, nitrogenous waste, hormones and water. ULTRAFILTRATION Factors affecting the glomerular filtrate rate (GFR) Pressure of glomerular filtrate – lower than the pressure in the blood Solute potential on either side of the filtration barrier ( water moves from less negative to more negative solute potential i.e. less concentrated to more concentrated solutions) Filtration rate can be increased by: Raising blood pressure Dilating afferent arterioles (vasodilation) Constricting efferent arterioles (vasoconstriction) ULTRAFILTRATION 125 cubic cm of glomerular filtrate produced per minute in humans = 180 cubic dm/day 1.5 cubic dm of urine is produced daily so a great deal of reabsorption must occur. 80% of this reabsorption occur in the proximal covoluted tubule. SELECTIVE REABSORPTION IN THE PROXIMAL CONVOLUTED TUBULES Proximal convoluted tubules are adapted for reabsorption: Large SA due to microvilli and basal channels Numerous mitochondria Closeness of blood capillaries 80% of GF is absorbed here, including: All glucose, amino acids, vitamins, hormones 80% of sodium chloride and water SELECTIVE REABSORPTION IN THE PROXIMAL CONVOLUTED TUBULES (PCT) Mechanism of reabsorption Glucose, amino acids and ions diffuse into the cells of the PCT from the filtrate. They are actively transported (carrier proteins in cell surface membranes) out of the cells into the spaces between them and basal channels. Once in these spaces they enter the extremely permeable blood capillaries by diffusion and are transported away from the nephron. Constant removal of substances create a diffusion gradient – further substances passes SELECTIVE REABSORPTION IN THE PROXIMAL CONVOLUTED TUBULES Mechanism of reabsorption As sodium and other ions are reabsorbed (tubular filtrate (less negative solute potential) water leave the tubular filtrate by osmosis. 40-50% of urea is reabsorbed by diffusion – not needed but harmless – remainder excreted in urine. SELECTIVE REABSORPTION IN THE PROXIMAL CONVOLUTED TUBULES (PCT) Mechanism of reabsorption Small protein – removed by pinocytosis at base of microvilli – hydrolytic enzymes from lysosomes digest proteins – resulting amino acids are used by the tubules or passed to the capillaries by diffusion. Active secretion of some substances such as creatine and urea occur out of capillaries – they are eventually removed in the urine. LOOP OF HENLE Function To conserve water. Longer the loop of Henle, the more concentrated the urine that could be produced. Useful adaptation to life on land ( beaver vs Kangaroo rat) Loop of Henle together with vasa recta and collecting ducts – create and maintain osmotic gradient in medulla (less concentrated at the cortex to more concentrated at the tips of the pyramids). LOOP OF HENLE Water leaves the nephron by osmosis in response to this gradient – concentrating the urine in the nephron. Descending limb – thin wall, highly permeable to water and most solutes Ascending limb – impermeable to water Cells in thick walled ascending limb actively reabsorb sodium, chloride, potassium and other ions. Fluid in ascending limb becomes very dilute by the time it reaches the distal convoluted tubule. DISTAL CONVOLUTED TUBULE (DCT) AND COLLECTING DUCT (CD) In these last two regions, fine tuning of the body fluid composition is achieved Roles DCT Fine control of precise amounts of water and salts important in osmoregulation Control of blood pH OSMOREGULATION AND ADH ADH – antidiuretic hormone – allows precise control of solute potential Diuresis – production of large amounts of dilute urine. Antidiuresis is the opposite. ADH is antidiuretic in its effect – concentrates urine. ADH – peptide also known as vasopressin ADH – produced in the hypothalamus OSMOREGULATION AND ADH When blood becomes more concentrated (solute potential more negative) When too little water is consumed Excessive sweating has occurred Large amounts of salt has been eaten Osmoreceptors in hypothalamus detect a fall in blood solute potential – signal is sent to posterior pituitary to release ADH ADH is sent to kidney where it increases permeability of distal convoluted tubule and collecting duct to water. OSMOREGULATION AND ADH Increased permeability is achieved by increasing the number of water channels in the membrane lining the tubules. When ADH secretion is stopped the process goes into reverse – reduction of water channels. OSMOREGULATION AND ADH In the presence of ADH Increased water channels Water moves from GF into cortex and medulla by osmosis Water is carried away in the blood Volume of urine is reduced and concentrated OSMOREGULATION AND ADH ADH also increases permeability of the collecting duct to urea Urea diffuses out of the urine into the tissue fluid of the medulla Increases the osmotic concentration Resulting in the removal of increased volume of water from the descending limb OSMOREGULATION AND ADH Opposite occurs with high intake of water Less negative solute potential of the blood ADH release is inhibited Walls of DCT and CD become impermeable to water Less water is reabsorbed from the filtrate Large volume of dilute urine is excreted. CONTROL OF BLOOD SODIUM LEVEL Maintaining blood plasma level at a steady state is controlled by aldosterone (steroid hormone) It also influences water absorption Secreted by the cortex (outer portion of adrenal gland) Decrease in blood sodium leads to a decrease in blood volume because less water enters the blood by osmosis. Results in a decrease in blood pressure CONTROL OF BLOOD SODIUM LEVEL Decrease in pressure and volume stimulates the juxtaglomerular complex - release renin Renin activates angiotensin – releases aldosterone from the adrenal cortex. Aldosterone acts on the DCT – stimulating sodium-potassium pumps – more sodium is pumped out of the filtrate in the DCT into the blood capillaries around the DCT K+ moves in the opposite direction – active transport CONTROL OF BLOOD SODIUM LEVEL Aldosterone also Stimulate sodium absorption in the gut Decrease loss of sodium in sweat Both effects assist in raising blood sodium level All together more water enters the blood by osmosis, increasing its volume and hence its pressure. CONTROL OF BLOOD PH Normal pH of blood plasma is 7.4 – must be kept in narrow limits as enzymes could become denatured – fatal Body produces more acids than bases – need to reduce acidity. Production of carbon dioxide increases acidity – carbonic acid (H₂CO₃) Carbonic acid – dissociate into hydrogen ions and hydrogen-carbonate ions CONTROL OF BLOOD PH Buffers – chemicals that resist pH changes Hydrogencarbonate ions can act as buffer. Hydrogencarbonaate and phosphate buffers help to prevent acidity. If the blood begins to become too acid Hydrogen ions are actively transported from the blood to the tubules of the collecting ducts. If source of the hydrogen ions is carbon dioxide, then hydrogen carbonate will move from tubule to blood by diffusion CONTROL OF BLOOD PH Fall in pH also stimulates the kidney cells to produce ammonium ions (NH₄⁺), which combines with acids brought to the kidney – excreted as ammonium salts. PATHOLOGY OF URINARY SYSTEM Nephritis – general term for inflammation of the kidneys – all or part of the nephrons, connective tissues or renal vessels may be affected. Nephrosis – non-inflammatory kidney disease Degeneration of tubules resulting in lowered albumin in the blood, albumen in the urine and edema – caused by toxins such as salts and heavy metals. Uremia – urine in the blood. Term used in conjunction with kidney failure. PATHOLOGY OF THE URINARY SYSTEM Urinary calculi – also called uroliths – stones in the urinary system. Kidney failure Result in the need for kidney transplant Or – haemodialysis – use of artificial membrane in a kidney machine Or – peritoneal dialysis – use of a natural membrane in the patients own body – peritoneum.